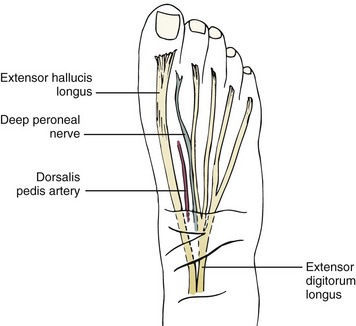
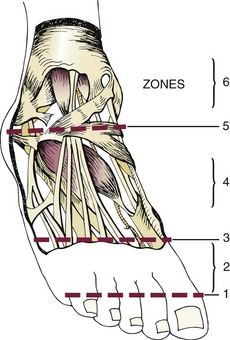
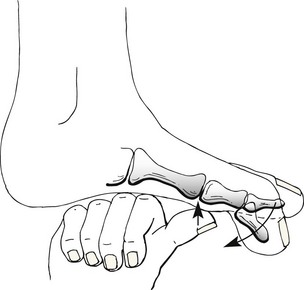
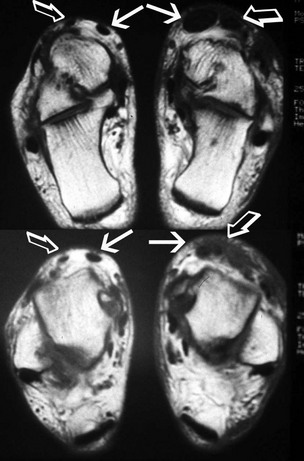
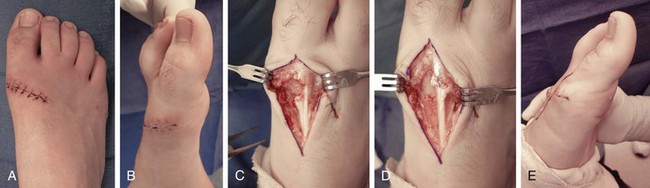
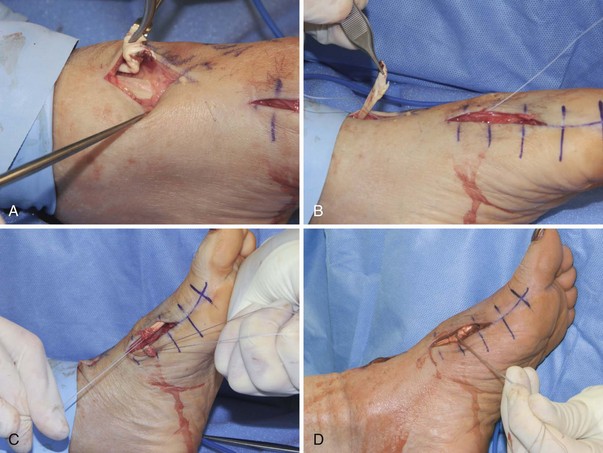
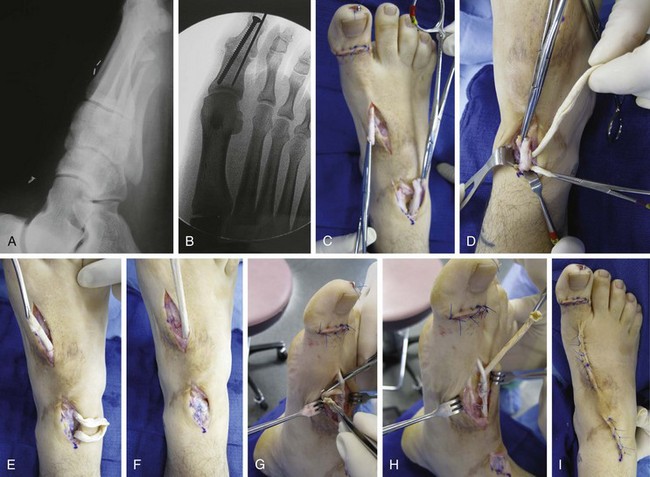
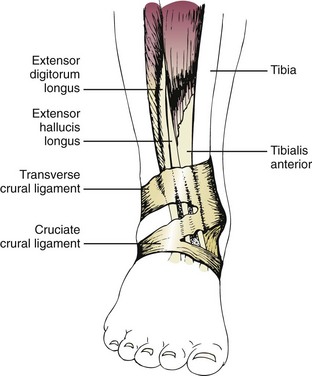
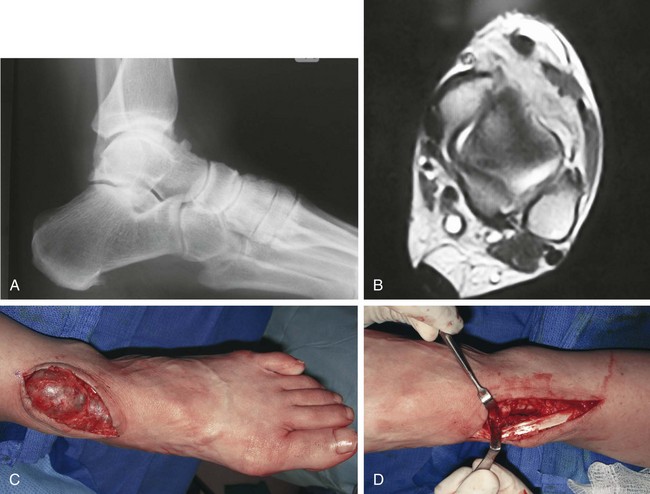
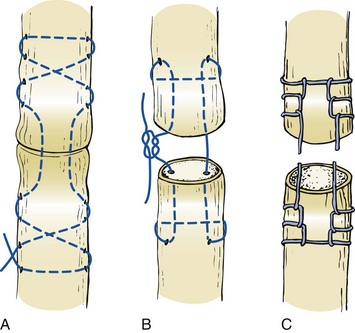
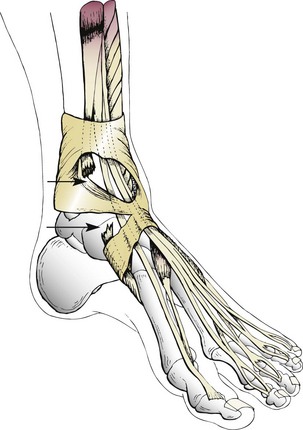
Chapter 24 ANTERIOR TIBIAL TENDON RUPTURE Flexor Digitorum Longus Tenosynovitis Flexor Hallucis Longus Tenosynovitis Flexor Hallucis Longus Rupture Peroneal Tendon Subluxation–Dislocation Intrasheath Peroneal Subluxation Posterior Tibial Tendon Subluxation–Dislocation Anzel et al3 evaluated 1014 cases of tendon injuries at the Mayo Clinic and noted that 21 injuries were to the extensors to the toes, a 2% incidence. They did not differentiate between injuries to the extensor hallucis longus (EHL) and extensor digitorum longus (EDL). Bell and Schon4 have noted that the EDL proper can only be lacerated between the ankle and the midfoot because individual tendons are found below this level. Above the ankle, the EDL tendons are in a more centralized location, but their slips are separate, making multiple EDL lacerations possible. Obliquity of the lacerations that occur above the ankle are indicative of a common mechanism, that being the falling of a sharp object against the leg or ankle (Fig. 24-1). One may be deceived when looking at these injuries because the superficial laceration may reveal intact tendon below, only to have the deeper tendon laceration occur more distally below intact skin. The EDL is relatively superficial and easily lacerated with trauma (Fig. 24-2). Because the main function of the EDL is extension of the metatarsophalangeal (MTP) joint and the proximal and distal interphalangeal (PIP and DIP) joints of the lesser toes, when it is transected and not repaired, a claw toe deformity can develop. Patients with chronic extensor tendon lacerations report difficulty controlling the toes when attempting to put on socks or slide into shoes. During these activities, the toe tends to catch on the fabric or insole and passively flex underneath the foot. Often, because of the proximity of the anterior tibial tendon to the extensor hallucis longus and the neurovascular bundle, injury to these structures can occur simultaneously. The EDL divides into two separate tendons beneath the superior retinaculum and then further divides into two lateral tendons to the fourth and fifth toes and two medial tendons to the second and third toes (Fig. 24-3). The individual tendon of the EDL to each toe is joined on the lateral aspect by the tendon of the extensor digitorum brevis. These individual tendons are anchored at the level of the MTP joint by a fibroaponeurotic dorsal digital expansion.24 Bell and Schon4 recommend that the EDL be primarily repaired using a modified Kessler suture technique. Alternatives include a modified Bunnell or Krackow technique (Fig. 24-4). Postoperatively, the foot is protected for 3 to 4 weeks with the foot and ankle in neutral position, with subsequent gradual initiation of passive range-of-motion exercises. The authors suggest night splinting after cast immobilization is discontinued. Figure 24-4 Technique of tendon repair. A, Modified Bunnell technique. B, Kessler technique. C, Krackow technique. Rooks23 reviewed reports of EDL injuries9,10,16,28,33 and noted 26 cases of EDL disruption. A preponderance of satisfactory results occurred after surgical repair. Lipscomb and Kelly16 reported on six lacerations of the EDL in combination with other tendon injuries and reported 50% good results. Floyd et al9 reported on eight EDL disruptions, seven of which were primarily repaired. The one tendon that was not repaired had a poor result. Other reports note generally good results with surgical intervention.10,28,33 Wicks et al33 reported on four lacerations of the EDL and concluded that those not repaired did not have a significant problem. Floyd et al9 reported a high incidence of painful dorsal scars after laceration of the dorsum of the foot. Rooks23 advised surgical repair of a disrupted EDL if it could be accomplished with minimal extension of the wound. He advised careful attention to associated nerve injuries as well. Akhtar and Levine1 reported a case of spontaneous dislocation of the EDL after a rupture of the inferior extensor retinaculum. They repaired the retinaculum and relocated the tendon successfully. The EDB is located on the lateral aspect of the forefoot and covers the lateral aspect of the subtalar joint. The tendons are quite small and are often injured after a laceration on the dorsolateral aspect of the foot. Bell and Schon4 suggest that if the tendons are easily identified at the time of an EDL repair, an EDB repair should be performed as well. If the EDB is not repairable, EDL repair alone is adequate. No series have been reported on repairs of the EDB. Kriza and Mushlin13 reported an avulsion fracture of the EDB from its origin on the calcaneus. It was treated nonsurgically with a successful result. An avulsion fracture of the EDB should be distinguished from an os peroneum, a fracture of the anterior process of the calcaneus, the peroneal trochlea, a fracture of the cuboid, or a rupture of the calcaneofibular ligament. The EHL originates on the midportion of the anterior fibula and the interosseous membrane and inserts onto the base of the distal phalanx of the hallux. Innervated by the deep peroneal nerve, it extends the hallux and everts the foot. The EHL receives its motor supply much farther distally than the anterior tibial muscle and the EDL. The motor branch to the EHL travels in close proximity to the fibula for about 10 cm before penetrating the muscle belly.25 The EHL is connected to the base of the proximal phalanx by the extensor aponeurosis, which receives contributions from the abductor and adductor hallucis. At the level of the ankle joint, the EHL becomes tendinous as it enters three successive soft tissue tunnels beneath the superior extensor retinaculum and inferior extensor retinaculum and within the extensor hood of the hallux (Fig. 24-5). These three areas play a role in a tendon entrapment or in preventing proximal retraction of the EHL tendon after injury.12 Lipscomb and Kelly16 noted that as the EHL passes beneath the extensor retinacular ligaments, it is enveloped in a separate sheath, providing a gliding mechanism on the anterior aspect of the tibia and ankle. Attritional ruptures can occur at or around the level of the ankle joint.19 Spontaneous ruptures of the EHL tendon occur, but lacerations are more common.2,6 On occasion, calcification can occur with associated tendinopathy.31 The patient might experience a sudden pop with a subcutaneous rupture of the EHL. Development of ecchymosis in the area of the tendon and tenderness to palpation are coupled with an inability to dorsiflex the great toe (Fig. 24-6). Tearing of the skin over the hallux IP joint may occur in association with the EHL ruptures that occur after severe IP plantar-flexion injuries. The tendon typically is not painful after rupture. An obvious defect may be present in the region of the anterior ankle with disruption of the EHL, and a gap may be noted. The tendon might not be palpable. EHB substitution can allow weak extension of the IP joint of the hallux.28 Patients having difficulty pulling on socks and shoes because of the weakened extension of the hallux readily experience the toe getting caught in the toe box or sock. Walking barefoot can be problematic because the patient can stub the hallux on the floor. In this situation, the toe tip has friction against the ground that, because of the forward motion and the lack of a full lift-off, results in a disruption of normal gait, making the patient vulnerable to tripping and/or falling. Depending on the location of the tendon disruption, some function might remain. Lacerations over the dorsum of the foot and the anterior ankle may be accompanied by injury to the anterior tibial or dorsalis pedis artery, deep and superficial peroneal nerves, and the anterior tibial tendon (Fig. 24-7). Al-Qattan2 classified the zones of injury of the extensor hallucis tendon lacerations into six areas: Zone 1: at the insertion site on the distal phalanx Zone 2: the area between zones 1 and 3 Zone 3: over the first metatarsophalangeal joint Zone 4: on the dorsum of the foot between zones 3 and 5 Zone 5: laceration of the tendon beneath the extensor retinaculum Zone 6: in the lower leg proximal to the extensor retinaculum (see Fig. 24-5). Extension of any laceration should be performed in a longitudinal direction to assess an injury to the EHL. Evaluation of the anterior tibial tendon, deep peroneal nerve, or other elements of the neurovascular bundle is important. The tendon is approximated and repaired with a 2-0 nonabsorbable suture with a modified Kessler or Krackow technique (Fig. 24-8; see Fig. 24-4). If the tendon is retracted, a more proximal incision or an extension of the exposure may be necessary in the area of the anterior ankle (Fig. 24-9), and a tendon graft may be necessary to bridge a substantial defect in the case of a delayed repair (Fig. 24-10).8,30,32 The tendon may become caught beneath the more proximal extensor retinaculum. It is also very helpful to dorsiflex the ankle and the toes to passively deliver the tendon ends into the wound. Once the ends are found, the surgeon can insert a long 25-gauge needle perpendicularly to skewer the tendon, and this keeps it from retracting. This is a relatively atraumatic way to hold the tendon during repair. After a primary repair, a posterior splint, brace, or cast is used for 4 weeks. Once the wound is stable, early passive and active assistive dorsiflexion of the MTP joint exercises can be initiated. Poggi and Hall22 recommend a below-knee cast with the ankle positioned at a 90-degree angle and further plantar flexion blocked. A removable boot brace is best used in compliant patients because it permits controlled passive and active assistive dorsiflexion but not active dorsiflexion of the toe and ankle, to minimize adhesions. One should avoid passive or active plantar flexion or active dorsiflexion until 4 to 8 weeks after the repair. At the time of an EHL injury, the foot often is in a dorsiflexed position, with the EHL under tension. Significant retraction can develop depending on the level of the laceration. Laceration of the digit distal to the extensor expansion may be evidenced by no significant tendon retraction because the extensor expansion prevents proximal migration.7,20 Scaduto and Cracchiolo26 reviewed the world literature and noted only 43 reported cases of extensor hallucis longus tendon lacerations. Undoubtedly, there are many more cases, but experience may be diluted by the small number of cases repaired at any one institution. Al-Qattan2 reported a large series of 15 patients treated with surgical repair of the EHL over a 12-year period. These included distal injuries as well as lacerations in zone 4 (over the dorsum of the foot). The author advocated temporary Kirschner wire fixation of both the interphalangeal and metatarsophalangeal joints for 6 weeks during the acute healing phase after the primary tendon repair. He reported a high level of satisfactory results. Duke and Greenberg7 recommend nonsurgical treatment after a distal injury. Noonan et al20 reported on three patients who sustained lacerations of the base of the nail with Salter fractures and concluded that these could be treated conservatively. More proximal EHL injuries have been reported by a number of authors.9,10,16,27–29,33 Floyd et al9 reported on 13 EHL lacerations, of which 11 underwent a primary repair. One was not repaired, and one had a secondary repair. Using a modified Kessler suture technique or a modified Bunnell technique, they reported seven good and six fair results. They concluded that a primary repair of the disrupted EHL is indicated. Wicks et al33 reported on 11 lacerations of the EHL, with 7 of 9 showing good results. They suggested that patients with a late, unrepaired tendon disruption may be better cared for by conservative treatment. Simonet and Sim28 reported on 5 lacerations of the anterior ankle treated with a primary repair with satisfactory results. Griffiths10 reported on six cases of EHL disruption in younger patients (ages 4, 19, 21, 22, 23, and 25), five of which were repaired acutely. Based on the one patient who did not have a surgical repair, the author concluded that “formal repair of the extensor hallucis longus seems unnecessary. Its natural tendency for spontaneous repair after tenotomy is well known.” Although this suggests that the EHL does not need to be repaired, Floyd et al9 noted that the sole justification for not repairing this tendon appears to be Griffiths’s one patient, who recovered spontaneously. Indeed, Griffiths did not even note the actual location of the injury. Kass et al12 observed that after an isolated tenotomy with the foot in a plantar-flexed position, minimal retraction occurs. On the other hand, with the EHL under tension, significant retraction can occur, and a significant gap can develop that precludes later tendon healing. Floyd et al9 did note significant proximal retraction of the EHL in two cases. Kass et al12 and Floyd et al9 concluded that tenotomies are quite different from lacerations of the EHL. Duke and Greenberg7 reported on 75 distal tenotomies of the EHL and found no evidence of weakness of the great toe in 16 patients seen in follow-up. Bell and Schon4 noted that the EHL, according to the literature, if left unrepaired, suffers no sequelae. They concluded, however, that these notions are based on the experience of Griffiths and thought it was imprudent to extrapolate that spontaneous recovery of EHL function routinely occurs and that EHL repair is not warranted. Since the time of that article, the authors have seen several minor chronic sequelae from a neglected laceration. The primary problems observed are clumsiness donning shoes or boots and plantar-flexion deformity of the hallux. In general, based on our clinical observations, efforts to repair the tendon should be undertaken when possible. Isolated rupture of the EHL occurs infrequently. Menz and Nettle18 described a case with rupture at the musculotendinous junction. Poggi and Hall22 reported on a closed rupture of the EHL at the level of the MTP joint that occurred several years after a cheilectomy. Sim and Deweerd27 reported on a spontaneous rupture of the EHL on the anterior aspect of the ankle in a skier. Spontaneous ruptures have also been reported after a hyper–plantar-flexion injury in a taekwondo athlete15 and from chronic impingement because of a dorsal talar osteophyte.8 One case of delayed rupture after injury from radiofrequency ablation during arthroscopic surgery has also been reported.32 McMaster17 stated that spontaneous rupture of a tendon rarely occurs without predisposing factors such as chronic disease. Successful surgical treatment centers on early diagnosis and prompt surgical intervention. Sim and Deweerd27 and Skoff29 repaired the tendon primarily, Langenberg14 used a free tendon graft, and Menz and Nettle18 transferred the peroneus tertius tendon to reconstruct the EHL. All had excellent results. With delayed treatment of an old EHL rupture, Berens5 noted that on initial exploration the proximal portion of the tendon could not be identified. Therefore the extensor hallucis brevis tendon was transferred into the distal stump of the extensor hallucis brevis. Menz and Nettle18 noted that a primary repair was not possible and used the tendon of the peroneus brevis that was mobilized and sutured it directly to the EHL. Hoelzer and Kalish11 also reported an EHL tendon disruption and noted at exploration 4 months after injury that the proximal end had retracted. The tendon of the EDL to the second toe was split and anastomosed to the distal stump of the EHL. Allografts and autografts have also been reported as a means to bridge significant defects with delayed treatment of EHL injuries with satisfactory results8,21,30,32,34 Postoperative scarring and adhesion formation can lead to diminished postoperative motion29 and may be a source of pain, but this is uncommon. Floyd et al9 reported that 38% of those injured had a painful scar. The actual site of injury is an important factor in developing a plan for treatment of a disruption of the EHL. If the injury is distal to the extensor expansion, nonsurgical treatment is considered, as long as the hallux can be maintained in a neutral position with tendon apposition. An injury proximal to the extensor expansion may be treated with a primary repair. Treatment of EHL injuries 6 weeks or later after injury is often associated with an inability to reapproximate the tendon ends. A tendon transfer or tendon graft may be necessary to bridge the interval gap (Fig. 24-11 and Video Clip 114 Aggressive surgical treatment of open lacerations about the foot is most important. Adequate exploration and debridement and anatomic restoration of tendons are usually appropriate. Although Griffiths10 noted that the EHL tendon might heal spontaneously and that formal repair is not indicated, review of the literature does not support the notion that conservative management is warranted. Surgical repair of the EHL is important when feasible. On the other hand, with significant soft tissue loss, an EHL repair might not be feasible, but secondary tendon grafting can be considered if there is a distal stump, pliable tissues without extensive fibrosis along the tendon path, and no evidence of infection. Subcutaneous rupture of the anterior tibial tendon has received little attention in the literature, and relatively few ruptures have been reported. Anagnostakos et al36 reviewed the literature and noted 110 published cases of anterior tibial tendon disruption; in only four series were there more than four cases, the remaining being case reports or very small series.3,16,68,77 In one of the largest series reported to date, Markarian et al68 described 16 anterior tibial tendon disruptions, including 10 ruptures and 6 lacerations. At this time, less than 150 cases (case reports or series) of anterior tibial tendon rupture have been reported in the literature. The anterior tibial tendon functions as the major dorsiflexor of the ankle,48 primarily during the swing phase, heel strike, and early stance phase of the walking cycle.41,81 It originates from the proximal half of the anterior tibia, the lower lateral tibial condyle, lateral tibia, and the interosseous membrane and inserts on the plantar medial aspect of the first cuneiform and the plantar base of the first metatarsal (Fig. 24-12). At the level of the lower and middle thirds of the tibia, it becomes tendinous and is surrounded by a synovial sheath. Anagnostakos et al36 reported on the dissection of 53 cadaveric specimens and reported three different patterns of insertion of the anterior tibial tendon into the medial midfoot. In 36 cases (68%), the tendon inserted into the medial cuneiform and base of the first metatarsal, and in 13 cases (25%), it inserted only into the medial aspect of the first cuneiform. In four feet (7%), the tendon inserted into both the cuneiform and the metatarsal, but there was an additional accessory tendon that inserted onto the base of the first metatarsal. Innervated by the deep peroneal nerve, the anterior tibial tendon functions to dorsiflex and invert the foot and provides controlled plantar flexion at heel strike. The tendon is active in heel-strike phase in an eccentric mode because it allows the ankle to slowly plantar flex until foot flat. It is active again in the swing phase in a concentric mode, dorsiflexing the ankle and keeping the forefoot from dragging. Congenital absence of an anterior tibial muscle and tendon is a rare occurrence42 and may be associated with clawing of the toes because of recruitment of the EHL and EDL to assist in dorsiflexion of the foot and ankle. The tendon passes beneath the superior extensor retinaculum and the upper and lower limbs of the inferior extensor retinaculum. Petersen et al78 investigated the structure and vascular pattern of the tibialis anterior tendon by using injection techniques, light and transmission electron microscopy, and immunohistochemistry. They found a well-vascularized peritenon, with blood vessels penetrating the tendon and anastomosing with a longitudinally oriented intratendinous network. Despite a well-vascularized posterior surface of the tendon, they found an avascular zone where the tendon runs under the superior and inferior retinacula. This results in an area 1 to 2 cm from the insertion that is at risk for rupture. Not only is the tendon vulnerable to spontaneous rupture here but, as the tendon passes beneath these retinacular structures, it also lies on the distal surface of the tibia and is at risk for injury with fracture of the tibia or a laceration.69 Lipscomb and Kelly16 stated that the tendon had 6 to 7 cm of excursion at this level. An acute disruption of the anterior tibial tendon can occur with trauma at any age from fracture of the tibia or laceration.43,45,65,68,69 Three quarters of these disruptions occur in male patients. A spontaneous rupture can occur from an underlying degenerative process.50,51,66 Inflammatory arthritis,49,62 gout,58 rheumatoid arthritis,46,68,77 impingement from an underlying exostosis, a local steroid injection,* and diabetes† have all been cited as contributing factors in anterior tibial tendon rupture. A ganglion in the region of the anterior ankle can masquerade as a rupture of the anterior tibial tendon, with the formation of an enlarged mass (Fig. 24-13).82 Ruptures occur near the anterior tibial tendon’s insertion, most often close to or within 2 to 3 cm of the insertion (Fig. 24-14). They can be caused by chronic wear from an exostosis at the talonavicular, naviculocuneiform, or metatarsocuneiform joints or by attrition from rubbing against the edge of the inferior extensor retinaculum.54 McMaster17 noted that ruptures occur in the presence of an abnormal tendon structure. This correlates well with the deficiency in the tendon’s vascular supply. Figure 24-14 Spontaneous rupture of anterior tibial tendon (arrows) typically occurs in distal 3 cm of tendon. Markarian et al68 have described “acute on chronic” tears manifesting as a degenerative tear in the anterior tibial tendon. These ruptures usually occur in men between the fifth and seventh decades of life and most often are reported in the seventh decade.38,44 They appear to develop as an age-related phenomenon. A prodromal phase is unusual, and patients do not routinely complain of pain before tendon rupture. Patients may notice an enlarged nodule on the degenerative tendon before rupture. Anterior tibial tendon ruptures occur with forced or excessive plantar flexion against a contracted anterior tibial muscle.38,64,71,81 An acute rupture is usually one of two different clinical presentations. With acute trauma in a younger patient who is involved with a higher functional level of activity, the rupture is associated with the acute onset of pain but infrequently with severe trauma. Walking down a ramp or slope can trigger eccentric contracture of the anterior tibial muscle, which may precipitate a tendon rupture. Decreased dorsiflexion strength is noted at the time of injury, which usually prompts the patient to seek medical evaluation and treatment soon after injury. On the other hand, an older patient typically has no history of antecedent trauma and often presents several months after the incident with a complaint of a painless footdrop.79 Frequently, a patient does not remember a precipitating event,81 and the older patient often is unaware of the condition.44 Markarian et al68 reported an average 10-week delay in diagnosis in their series of 16 anterior tibial tendon disruptions. Late diagnosis is common, and permanent disability is rare. The patient often experiences a snapping sensation that is associated with a brief episode of sharp pain over the anterior aspect of the ankle and is accompanied by swelling. Ambulation may be difficult in the initial few hours after rupture, but the pain subsides rapidly. A patient might note lack of coordination, a slapping gait, or an inability to clear the toes with ambulation. In time, the anterior tibial muscle atrophies. Both Frigg et al50 and George et al51 have reported cases of simultaneous degeneration of the anterior tibial and posterior tibial tendons that required hindfoot arthrodeses and anterior tibial tendon reconstructions. The anterior tibial tendon, on occasion, may be involved with tendinopathy (tendinitis or tendinosis), as described by Burman,39 Goldman,53 and Hamilton.56 Beischer et al37 has described a series of 29 cases of tendinosis that were characterized by swelling over the insertion, nocturnal pain, and, on examination, point tenderness over the insertion of the anterior tibial tendon. Beischer et al observed longitudinal split tears in the distal tendon in 19 of 29 cases and typical tendinosis on those that were explored. They found a much higher incidence of involvement in females in this series and speculated that this may be a different clinical entity than the typical patient (typically elderly males) who sustains a spontaneous rupture of the tendon. Beischer et al suggested a provocative “stretch” test to assess tendinosis, which included forced ankle plantar flexion, midfoot eversion, and abduction with a pronation force applied to the foot in an attempt to acutely passively stretch the anterior tibial tendon. A positive test was characterized by aggravation of the typical pain the patient had previously experienced. In a follow-up study on the operated patients in this series, Grundy et al54 reviewed the results of 12 cases, mostly women, who were explored for tendinosis and longitudinal tears of the distal anterior tibial tendon. Although there was evidence of macroscopic tendinosis in all cases, those with less than 50% degeneration were treated with a debridement while those with greater than 50% degeneration were treated with debridement and an EHL tendon augmentation. Later rupture in those who only had a debridement, led the authors to recommend more aggressive reconstruction and use of the EHL augmentation on a routine basis. Insertional tendinopathy can occur after prolonged walking or running. Besides the localized pain, patients may complain of pain in the anterior ankle and lower leg. At times, it will manifest as anterior “shin splints” or even chronic exertional compartment syndrome. The repetitive eccentric load at the bone tendon interface of the contracted anterior tibial tendon musculotendinous unit during impact on heel strike induces microtears that generate a localized inflammatory response. The condition can be exacerbated while descending slopes or inclines, when the sudden jarring at the insertion of the anterior tibial tendon at the cuneiform is maximized. Avoiding these stresses and wearing cushioned heeled shoes can help the tendon to recover. For more intractable cases, patients will benefit from a CAM-boot or an ankle–foot orthosis (AFO). Platelet-rich plasma derived from peripheral blood, or bone marrow injected at the tendon insertion can be helpful in conjunction with immobilization when bracing alone is unsuccessful.59 Steroid injections at this location should be avoided to minimize the risk of tendon rupture (Fig. 24-15).
Disorders of Tendons
Extensor Tendons
Extensor Tendon Injuries
Extensor Digitorum Longus
Anatomy
Surgical Treatment
Extensor Digitorum Brevis
Extensor Hallucis Longus
Anatomy
History and Physical Examination
Surgical Treatment
Results and Complications
Conclusion
![]() ). In these cases, one should assess the amount of tendon loss by placing moderate tension on the tendon ends and placing the ankle and hallux in neutral position. When the tendon ends cannot be opposed without excessive tension, a tendon slide, using healthy proximal EHL tendon for defects up to 4 to 5 cm, may be attempted. For anything greater than a 5-cm gap, a tendon transfer may be performed. Although in the past a common reported transfer was the peroneus tertius,18 a split of the extensor to the second toe for use in lacerations distal to the ankle joint11 is a good alternative. Allograft and autograph tendon transfers have become more popular to bridge obvious tendon gaps.8,21,30,32,34
). In these cases, one should assess the amount of tendon loss by placing moderate tension on the tendon ends and placing the ankle and hallux in neutral position. When the tendon ends cannot be opposed without excessive tension, a tendon slide, using healthy proximal EHL tendon for defects up to 4 to 5 cm, may be attempted. For anything greater than a 5-cm gap, a tendon transfer may be performed. Although in the past a common reported transfer was the peroneus tertius,18 a split of the extensor to the second toe for use in lacerations distal to the ankle joint11 is a good alternative. Allograft and autograph tendon transfers have become more popular to bridge obvious tendon gaps.8,21,30,32,34
Anterior Tibial Tendon Rupture
Anatomy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Disorders of Tendons