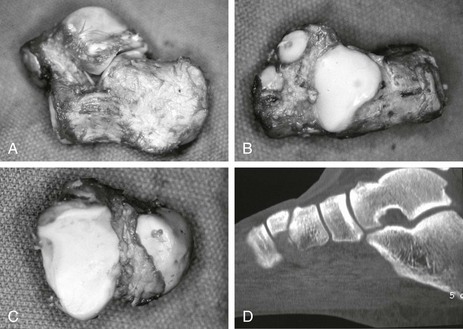
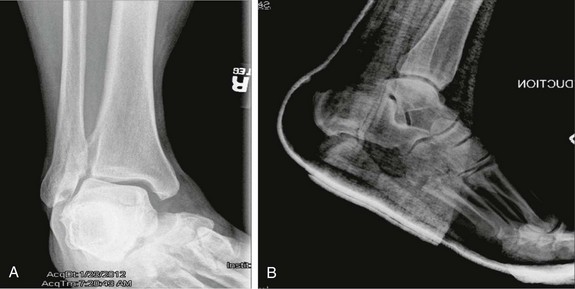
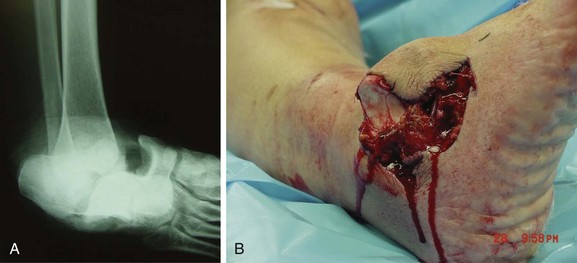
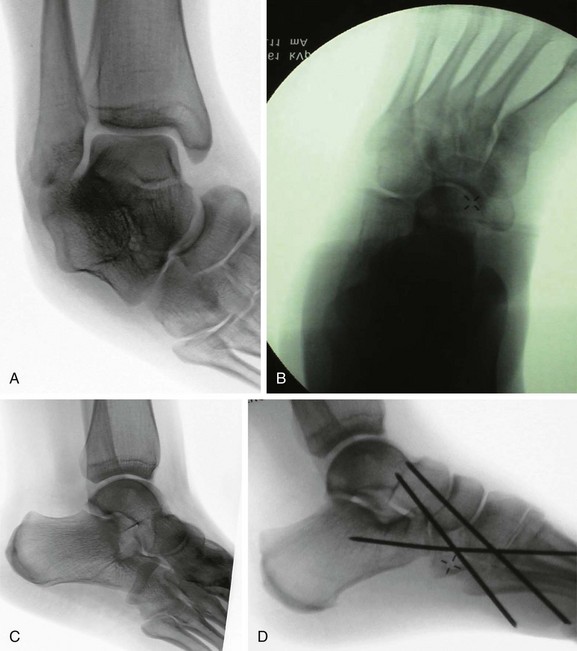
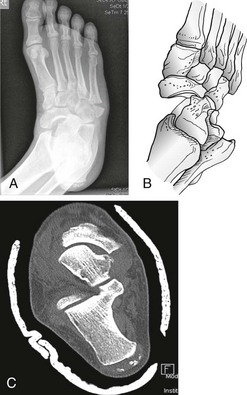
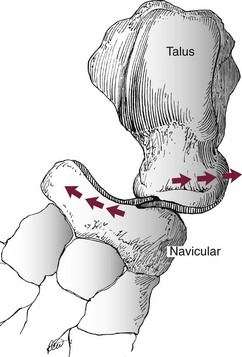
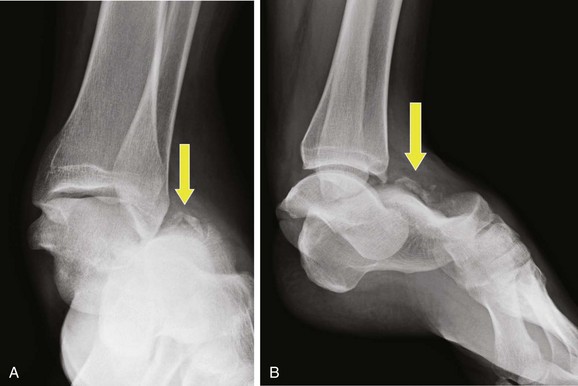
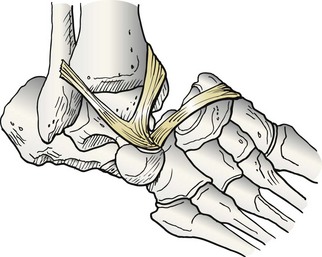
Chapter 35 Authors’ Preferred Method of Treatment METATARSOPHALANGEAL JOINT DISLOCATIONS Hallux Metatarsophalangeal Injuries LESSER TOE METATARSOPHALANGEAL DISLOCATIONS INTERPHALANGEAL JOINT DISLOCATIONS Subtalar dislocation, initially reported by DuFaurest67 and Judcy146 in 1811, defines the simultaneous dislocation of the subtalar and talonavicular joints without associated dislocation of the calcaneocuboid or tibiotalar joints and without talar neck fracture. These injuries occur infrequently, representing 1% to 2% of all dislocations18,55,80,163,247 and 15% of all injuries involving the talus.218 Men are 3 to 10 times more likely than women to sustain this injury,55,103,125,245 which typically occurs in the mid-30s.125,273 After Judcy’s and DuFaurest’s descriptions of subtalar dislocations in 1811, Broca23 classified these injuries in 1853 as medial, lateral, and posterior, in descending order of frequency. Malgaigne175 modified this classification in 1856, adding the rare anterior subtalar dislocation. This classification remains the most widely used, although some doubt has been raised regarding whether posterior and anterior dislocations truly represent separate injuries or are merely caused by secondary displacement after primary medial or lateral dislocation.19,84 These dislocations have been alternatively termed subastragaloid,245 subastragalar,247 peritalar,8 and talocalcaneonavicular.84 Other designations have included “basketball foot”109 and “acquired clubfoot,”253 both of which refer to medial dislocations, and “acquired flatfoot,” which describes lateral dislocation.159 Broca’s original classification,23 as modified by Malgaigne,175 remains relevant today and is the most widely used. Although the classification simply describes the direction of displacement, it also has prognostic value because of the varying pathomechanics and functional outcomes associated with the different types of dislocation. The classification is purely anatomic, describing, in descending order of frequency, medial (80%), lateral (17%), posterior (2.5%), and anterior (1%) subtalar dislocations.273 It is important to differentiate pure anterior and posterior dislocations from medial and lateral dislocations with secondary sagittal displacement. Lack of attention to this detail may have led to overreporting of anterior and posterior dislocations and subsequent skepticism about their actual existence.19,84 These pure sagittal plane displacements are indeed rare, representing 3% of all reported cases,273 but their presence as an entity distinct from their medial and lateral counterparts is well established.* The subtalar joint comprises three articular facets (anterior, posterior, medial) through which the talus articulates with the calcaneus, permitting inversion and eversion of the foot (Fig. 35-1). The joint is stabilized by its inherent bony structure and by supporting soft tissue structures. The dense talocalcaneal interosseous ligament within the sinus tarsi and capsular structures around each individual facet, strengthened medially by the superficial deltoid ligament and laterally by the calcaneofibular ligament, constitute the main capsuloligamentous supports. Cadaveric studies have demonstrated that the calcaneofibular, superficial deltoid, and talocalcaneal ligaments must all tear for either medial or lateral dislocation to occur, whereas the calcaneonavicular “spring” ligament remains uninjured.27 The posterior process of the talus, consisting of medial and lateral tubercles separated by a groove for the flexor hallucis longus tendon, serves as the posterior roof of the subtalar joint. The medial tubercle serves as an attachment for the deep deltoid ligament, and the lateral tubercle provides the insertion of the posterior talofibular ligament. Each of these in isolation or combination can be fractured in association with a subtalar dislocation (Fig. 35-2).34–36,72–74,204 Between 50% and 80% of subtalar dislocations are caused by high-energy injuries, such as motor vehicle accidents or falls from a height.13 The remainder occur after surprisingly trivial injuries, such as a simple inversion injury of the foot.13,109 These represent two distinct injury types, with generally a higher incidence of lateral dislocations, open injuries, associated fractures, and poor results after higher-energy injuries.103 Medial subtalar dislocation occurs with forceful inversion of the plantar-flexed foot, where the talar neck acts as a fulcrum about which the sustentaculum tali pivots (Fig. 35-3). The result is either a talar neck fracture or sequential medial dislocation of the talonavicular and then the subtalar joints.120,159,247 Figure 35-3 Anteroposterior radiograph demonstrates medial dislocation of both talonavicular and subtalar joints. Lateral subtalar dislocation occurs with forceful eversion of the plantar-flexed foot (Fig. 35-4). In this instance, the anterolateral talus acts as a fulcrum about which the anterior process of the calcaneus pivots, similarly resulting in a talar neck fracture or in sequential lateral dislocation of the talonavicular and subtalar joints.120,159,247 Considerably greater force is required to cause a lateral subtalar dislocation. This fact likely explains the observation that lateral dislocations are much more commonly associated with severe soft tissue damage, open injuries, and associated fractures.55,38,125 Continuation of the forces that cause either medial or lateral dislocation produces a variant of subtalar dislocation with associated tibiotalar subluxation (Fig. 35-5).153 Often, the tibiotalar subluxation resolves once the subtalar dislocation is reduced. This situation represents the intermediate stage between a true subtalar dislocation and a complete pantalar dislocation (Fig. 35-6). Although the calcaneocuboid joint usually remains intact after subtalar dislocation, another variation involves dislocation of the subtalar joint and the entire transverse tarsal joint, known as a peritalar dislocation (Fig. 35-7). Finally, the few documented true posterior subtalar dislocations have been caused by severe plantar-flexion forces.10,136,157 Pure anterior dislocations occur when anterior traction on the foot first tears the talocalcaneal interosseous ligament, followed by the medial and lateral ligaments. The low probability of exposure to this distractive type of force makes anterior dislocation very unusual.135 Medial subtalar dislocations represent 80% of reported cases273 and can occur after high-energy injuries, such as motor vehicle accidents, or after trivial inversion injuries of the ankle,27,55,69 as in the case of “basketball foot.”109 Forty percent of these dislocations are associated with an open injury.69,192 Although the presence of a hindfoot deformity is obvious,55 the injury is often misinterpreted as an ankle dislocation before radiographic evaluation establishes its true nature.112 The deformity is consistent, with the heel displaced medial to the leg because of severe inversion, plantar flexion, and adduction of the entire foot, with apparent shortening of the medial border.84 The resulting deformity has inspired the term acquired clubfoot.253 If the skin is intact, it is usually tented over the prominent, palpable talar head dorsolaterally and over the lateral malleolus. Lateral dislocations constitute approximately 17% of subtalar dislocations.104,273 Because of the increased force required to produce the injury, lateral dislocations rarely occur after trivial trauma, and greater than 50% present as open injuries.55,56,192 The deformity is clinically obvious, with lateral displacement of the heel, severe pronation and abduction of the foot, and apparent shortening of the lateral border.27,84 In these cases, the talar head is prominent medially, and intact skin is tented over both the talar head and the medial malleolus. The normal longitudinal axis of the foot is maintained in both posterior and anterior dislocations, which constitute only 2.5% and 1% of all subtalar dislocations, respectively.273 Although the deformity is much less pronounced than in medial and lateral dislocations,8 the foot appears foreshortened in posterior dislocations and lengthened with apparent flattening of the heel in anterior dislocations.135,136,149,159,247 Medial subtalar dislocation results in medial and plantar displacement of the navicular relative to the talar head and medial displacement of the calcaneus relative to the talus. In the majority of cases, the calcaneocuboid articulation remains intact, but in rare instances, all three hindfoot joints will be dislocated (see Fig. 35-7). Associated fractures include impaction of the dorsomedial talar head and lateral navicular and fracture of the medial and lateral tubercles of the posterior process of the talus.34–36,73,84,204 Fractures may be more evident after reduction. The talonavicular impaction in particular can serve as an obstruction to closed reduction27,38,153,163 and should therefore be recognized (Fig. 35-8). Lateral subtalar dislocations are identified by lateral displacement of the navicular relative to the talar head and of the calcaneus beneath the talus with an intact calcaneocuboid joint. As with medial subtalar dislocations, impaction of the navicular on the talar head can result in fracture of the lateral aspect of the talar head and prevent reduction (Fig. 35-9). Associated fractures commonly involve the cuboid, anterior calcaneal process, lateral talar process, lateral talar head, and the lateral malleolus (Fig. 35-10).27,84,237 Posterior dislocations are characterized by minimal displacement in the frontal plane and posterior displacement of the subtalar and talonavicular joint such that the superior lip of the navicular lies against the undersurface of the talar neck.10,136 Anterior dislocations have little frontal plane displacement, but anterior translation of the subtalar joint occurs such that the posterosuperior margin of the posterior calcaneal facet lies against the undersurface of the talar neck at the sulcus.135 After prompt reduction of the dislocation, AP and lateral radiographs of the foot, as well as AP and mortise views of the ankle, are essential to confirm a successful reduction and to demonstrate restoration of appropriate overall foot alignment and reduction of the talonavicular and subtalar joints. Because of the absence of deformity, postreduction radiographs are usually of much better quality than those obtained at the time of injury and should therefore be scrutinized for associated fractures. It should be emphasized that the majority of subtalar dislocations occur with concomitant fractures of the hindfoot, including osteochondral fractures, calcaneus fractures, and fractures of the posterior process and tubercles of the talus. These fractures have been reported to occur in 50% to 100% of subtalar dislocations.55,189,147 Intraarticular osteochondral fractures are particularly common, occurring in 50% to 71% of all subtalar dislocations and in up to 100% of lateral dislocations,13,55,125,273 the majority of which involve the subtalar joint.38 These fractures are less common in medial dislocations, occurring in only 12% to 38% of injuries.55 Because associated intraarticular fractures can prevent anatomic reduction and worsen the overall prognosis,8,55,147,245,247 and because of the difficulty in detecting them on plain radiographs,17,55 routine postreduction computed tomography (CT) has been recommended to identify these fractures more accurately (Fig. 35-11).13,55 A prompt reduction is essential in avoiding skin necrosis and circulatory compromise.8,44,154,179 The principles of reduction involve flexion of the knee to relax the proximal pull of the gastrocnemius–soleus complex on the calcaneus, followed first by accentuation and then by reversal of the deformity.84,109 Traction is applied to the heel as this maneuver is performed, and countertraction is applied to the posterior aspect of the thigh proximal to the flexed knee. Direct pressure on the prominent talar head facilitates the reduction, which is often seen, heard, and felt.27,55,125 If performed shortly after injury, reduction can be achieved in a majority of patients with minimal sedation.125 Delay in treatment renders the reduction considerably more difficult and can require regional or general anesthesia.With medial dislocations, the reduction maneuver consists specifically of plantar flexion and inversion of the foot, followed by eversion and dorsiflexion while plantar-medial pressure is applied to the dorsolaterally displaced talar head. With lateral dislocation, reduction is achieved by eversion, followed by inversion of the foot while lateral pressure is applied to the medially displaced talar head.27 Posterior dislocations are reduced by first plantar flexing the forefoot to disengage the superior edge of the navicular from the undersurface of the talar neck. The heel is then translated distally as longitudinal traction is applied, and the foot is finally dorsiflexed while plantar pressure is applied to the dorsally displaced talar head.10,59,136 In anterior dislocations, longitudinal traction must be applied to the foot to disengage the posterosuperior edge of the posterior facet from the talar sulcus. Proximal translation of the foot while maintaining longitudinal traction of the heel completes the reduction.135,159 In approximately 5% to 10% of closed medial dislocations and 15% to 20% of closed lateral dislocations, reduction cannot be achieved by closed methods. In these cases, open reduction is warranted. With medial dislocations, impediments to closed reduction include buttonholing of the talar head through the extensor retinaculum (Fig. 35-12)115,120,125,163 or the talonavicular capsule,38,125,151 interposition of the deep peroneal neurovascular bundle (Fig. 35-13)120 or the peroneal tendons, and impaction of the lateral navicular into the medial talar head (see Fig. 35-8).13,27,38,153,163 Buttonholing of the talar head through the extensor digitorum brevis tendon has also been described,162,163 although cadaveric studies have shown this to be an unlikely occurrence because the muscle belly is considerably plantar to the talar head (see Fig. 35-13).120 Impaction of the medial navicular onto the lateral talar head and superolateral displacement of the posterior tibial or flexor digitorum longus tendon over the talar neck are largely responsible for blocking reduction of lateral subtalar dislocations (Fig. 35-14).13 Incisions extending from the prominent talar head to the medial malleolus or to the sinus tarsi have been recommended to provide access to each of these potential obstructions during open reduction.
Dislocations of the Foot
Subtalar Dislocations
History
Classification
Anatomy
Mechanism of Injury

Clinical Evaluation
Radiographic Evaluation
Treatment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Dislocations of the Foot