Fig. 1
MRI of the right knee confirmed the diagnosis of a predominantly medial osteoarthritis
For this indication a medial unicondylar knee replacement (UKR) was performed. As the medial-sided pain still persisted half a year after UKR, an ischemic necrosis of the posterior, superior part of the medial condyle was suspected, and a CT-guided biopsy was performed. The histology of the biopsy did not reveal a clear cause of the patient’s problems. Histology showed an unspecific inflammatory process.
Questions
1.
Night pain can be related to what?
2.
What would you do with such a histological result?
3.
How would you treat the patient’s pain?
As the pain still persisted 12 months after UKR, the orthopaedic surgeon decided to revise the UKR to a TKR. As the cause of the patient’s persistent pain, an ischemic necrosis of the posterior-superior part of the femoral condyle was identified. The surgeon decided also to debride the bone lesion using a curette and fill the osseous defect with cement, which was done by the interventional radiologist before TKR. A histological assessment was not performed at this stage.
Questions
1.
Would you have revised the UKR or would you have insisted on further diagnostics?
2.
Would another biopsy at revision from UKR to TKR important?
3.
What would you do differently?
However, again the patient’s pain still persisted after cruciate-retaining TKR.
At first presentation to our clinic, the patient localised his pain to the posterior and lateral part of the knee joint. The pain was worse during the night, keeping the patient awake. In addition, the patient reported an increased pain level when drinking a glass of wine. Clinical examination showed no signs of infections, no swelling and no wound-healing problems. There was no joint tenderness on palpation. The knee was stable in varus-valgus and anterior-posterior direction. It showed a good range of motion (flexion-extension 130°–0°–0°). The patient’s pain was not able to be provoked while examination.
Questions
1.
What are your next diagnostic steps?
2.
What is your differential diagnosis?
Conventional radiographs (anterior-posterior, lateral and patella skyline view and long-leg standing, Fig. 2) did not reveal a gross malposition of TKR. In the posterior part of the femur, an osteoblastic lesion around the cement was suspected. On long-leg radiographs the mechanical axis passed through the centre of the knee joint representing a neutral alignment.
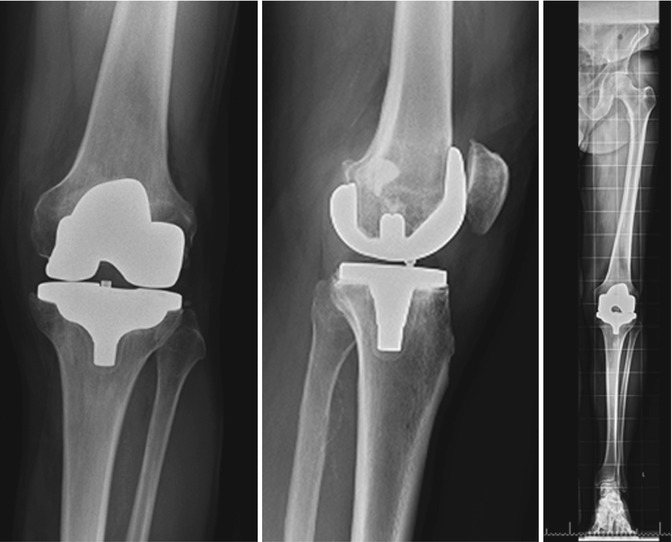
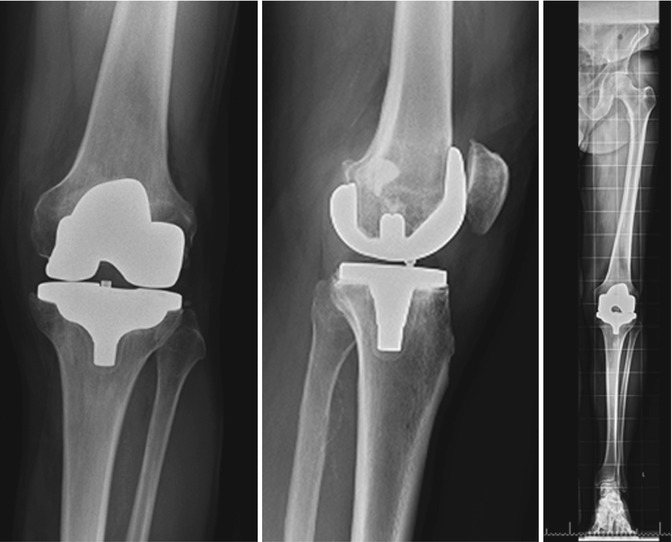
Fig. 2
Anterior-posterior, lateral and long-leg standing view of the right knee after cruciate-retaining TKR showed no gross malposition of TKR, but an osteoblastic lesion around the cement in the posterior femur was suspected
Questions
1.
What are your next diagnostic steps?
2.
Is component malposition ruled out?
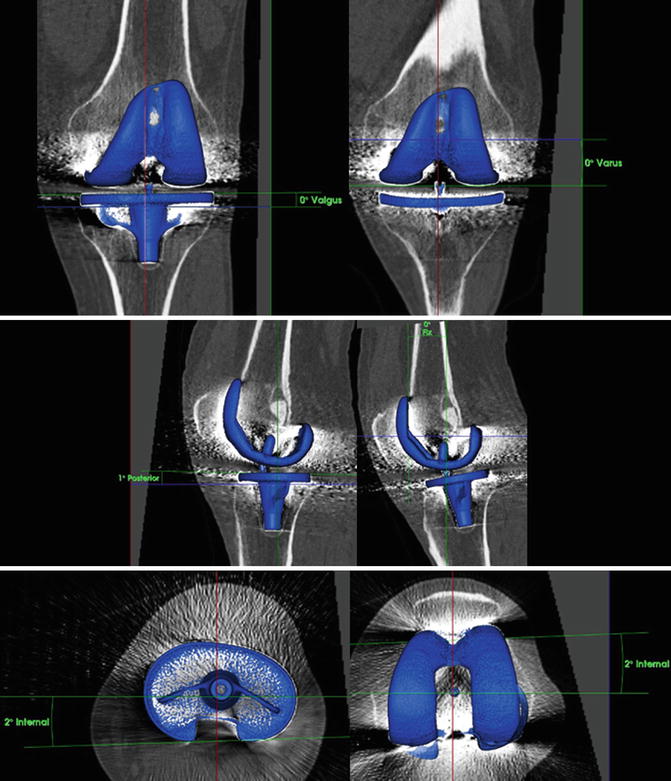
A 99mTc-HDP-SPECT/CT was performed. TKR component position was determined using 3D-CT as part of SPECT/CT (Figs. 3 and 4). The TKR prosthesis was well positioned in all six degrees of freedom.