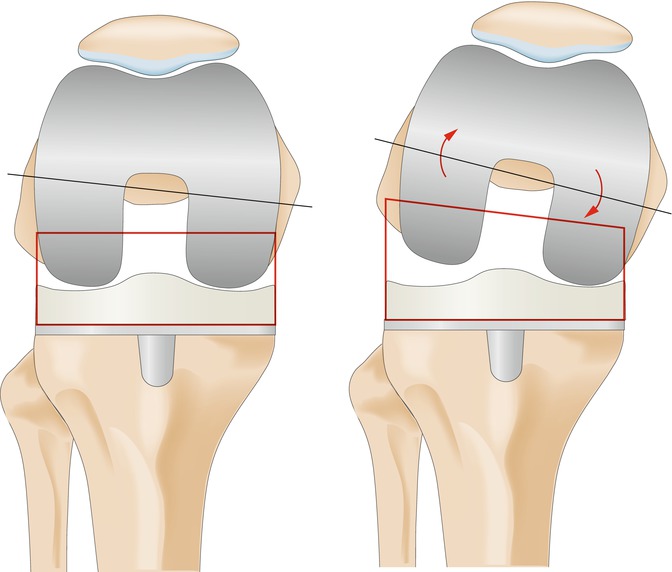
Fig. 1
Radiographs (anteroposterior, lateral and axial patella) of the left knee showing the posterior-stabilised rotating platform TKR. The patella has not been resurfaced. The TKR component position (varus-valgus) appeared normal on these radiographs. However, the femoral TKR component showed increased flexion
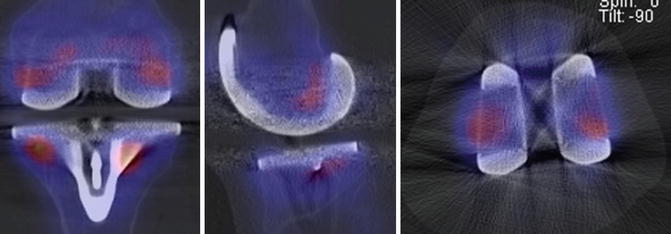
Fig. 2
99mTc-HDP-SPECT/CT images of the left knee showing only minor tracer uptake around the femoral TKR component, indicating a well-fixed TKR
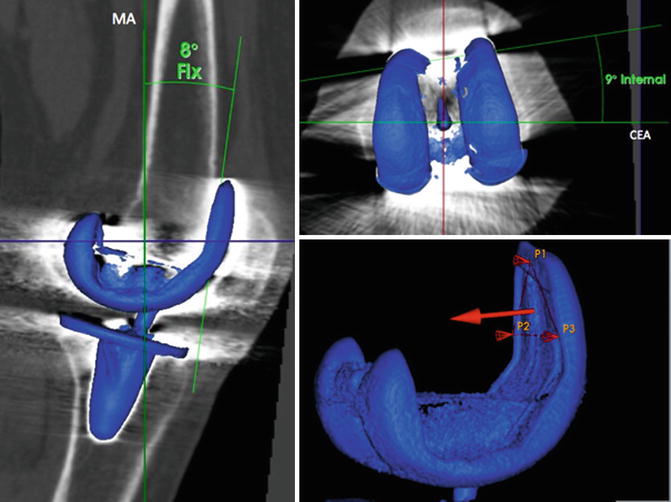
Fig. 3
Measurements of the left femoral TKR component position using a customised and validated software. Flexion (left) and rotation (right top) of the femoral TKR component was determined using standardised frames of reference (right bottom)
Questions
1.
What is your diagnosis and proposed treatment?
2.
How would you address the femoral component malposition?
3.
Would you do a secondary patellar resurfacing?
A complete revision TKR with secondary resurfacing of the patella was performed. At revision surgery, a remarkable femoral liftoff in the lateral compartment was seen at 60–90° of flexion. The femoral TKR component was clearly internally rotated. The femoral shield was then implanted in 3° external rotation with regard to the transepicondylar axis and to a balanced joint gap in flexion and extension. Postoperative radiographs showed a correct placement of the TKR components (Fig. 4).


Fig. 4
Radiographs (anteroposterior, lateral) of the left knee after total revision surgery
At discharge, no complications were reported, and the range of motion at 3-month follow-up was flexion/extension 115°/0°/0°. The patient was pain free and did not complain about instability while climbing stairs.
Discussion Points
Assessment of Component Position
Postoperative component position is most commonly assessed on radiographs or on axial CT scans [2, 18, 20, 22]. In this case, the position of the femoral component was assessed using a previously validated customised software, which is able to reconstruct three-dimensional images from CT data [7]. Rotational alignment was measured as the angle between the clinical epicondylar axis (CEA), which was determined as the line that connects the medial and lateral epicondylar prominences and a vertical plane defined by three points on the anterior femoral shield (Fig. 3). According to the work of Kanekasu et al. [12], the determination of CEA is more feasible than the surgical epicondylar axis (SEA), which is defined as the connecting line of medial sulcus and lateral epicondyle. In this study, it was reported that identifying the medial sulcus is often difficult due to osteoarthritic changes and that SEA is on average 4° internally rotated relative to CEA.
Intraoperative Rotational Placement of the Femoral Component
To achieve an optimal intraoperative rotational alignment, two techniques are commonly used in TKR surgery [22]. One method relies on the determination of bony landmarks such as the medial and lateral epicondyles, of which the connecting line (CEA) is considered to represent the flexion axis of the knee joint [4]. To maintain the flexion axis, the femur is cut with regard to the CEA. The posterior condyles or the anterior-posterior axis defined by Whiteside and Arima [21] are commonly utilised landmarks for rotational positioning of the femoral component. The other principal technique is the intraoperative balancing of the joint gap in flexion using ligament tensioners to achieve a rectangular joint gap with equal lateral and medial loading [5]. Disadvantages exist for both techniques: While the “landmark method” is subject to high variances in intraoperative defining of the CEA [11] and could result in an imbalanced joint gap [15], the “tension method” could shift the knee in varus malalignment in weight-bearing flexion [6]. Considering the possible limitations of both methods, Hofmann et al. [8] recommended the combined usage of both techniques to achieve optimal rotational alignment.
Effects of Femoral Internal Rotation
Internal malrotation strongly affects the flexion gap. It results in an increased lateral opening and consecutive instability in flexion movements such as stair climbing or downhill walking [22]. The observed lateral condylar “liftoff” in flexion (Fig. 5) is known to correlate with internal malrotation of the femoral component [10, 17]. However, its clinical relevance remains unclear as lateral condylar liftoff was seen in clinically successful TKRs as well [19]. It was not observed in this presented case, but it has been shown that patellofemoral maltracking and accelerated wearing of the tibial polyethylene inlay are highly associated with femoral internal malrotation [3, 13].