Digital Sympathectomy
Imran K. Choudhry
Beth Paterson Smith
L. Andrew Koman
INTRODUCTION
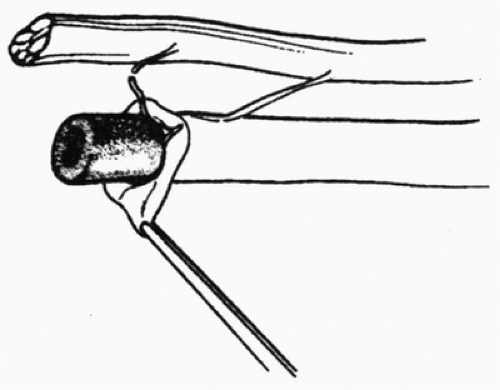
Digital sympathectomy is a surgical procedure that mechanically disrupts sympathetic connections between the parallel nerves and sympathetic fibers in the adventitia accompanying distal vessels (Fig. 31-1). These sympathetic neural structures can potentiate inappropriately prolonged vasospasm or stimulate inappropriate arteriovenous shunting. Following digital sympathectomy, arterial vasoconstriction decreases and nutritional perfusion improves, which, in turn, decreases symptoms and may facilitate healing of refractory ulcers or sores (1,2). Synonyms of digital sympathectomy include periarterial sympathectomy, peripheral sympathectomy, digital artery sympathectomy, and arteriolysis.
Peripheral vascular disorders of the upper extremity are challenging to diagnose, treat, and manage. Vascular insufficiency and vasospastic disease may produce pain, cold intolerance, numbness, digital ulceration, and/or infection. Vascular pathology negatively impacts health-related quality of life, function, and productivity. The pathoanatomy of peripheral vascular disorders can be secondary to congenital and/or acquired conditions that affect vascular structure or function (e.g., an occlusive event [thrombosis/embolism] or vasomotor control abnormalities [precipitated by trauma or disease]). Vasoconstriction is stimulated by sympathetic branches accompanying sensory nerves innervating distal arteries and by sympathetic nerves on arterial adventitia. Sympathetic excitation within vascular smooth muscle stimulates the release of á-adrenergic neurotransmitters, which bind with postsynaptic sympathetic receptors producing smooth muscle contraction (3,4,5). Increased sympathetic tone can occur after soft-tissue or bony trauma, nerve injury, or vessel injury or from disease states. Thrombosis or embolism often produces a reactive vasospasm, which, if it occurs concomitantly, produces inadequate collateral circulation, leading to digital signs and symptoms (2,6). Alleviating sympathetic tone via surgical digital arterial sympathectomy (DAS) can limit vasoconstriction and reduce hand ischemia by increasing nutritional flow (7,8,9,10,11).
The Wake Forest Classification of Vascular Disease (Table 31-1) is used to guide treatment options in patients with peripheral vascular disorders. Raynaud’s disease (Group I) is idiopathic and selflimited and patients rarely require surgical intervention. Although symptoms are common after nonvascular injury, patients with secondary vasospasm (Group II) almost never require sympathectomy. However, sympathectomy may be beneficial for managing refractory symptoms in patients with Raynaud’s phenomenon with inadequate collaterals (Group IIB) and secondary vasospasm from occlusive disease with inadequate collaterals (Group IIIB). Patients with Raynaud’s phenomenon who have adequate collaterals (Group IIA) and patients with secondary vasospasm from occlusive disease who have adequate collaterals (Group IIIA) rarely require digital sympathectomy (2).
The primary treatment of symptomatic vasospastic disease is medical, that is, treatment includes medications to treat the underlying disease and calcium channel blockers and environmental adaptations (e.g., appropriate clothing and gloves) to manage symptoms (2,5).
TABLE 31-1 The Wake Forest Classification of Vascular Disease | ||
|---|---|---|
|
INDICATIONS FOR DIGITAL ARTERIAL SYMPATHECTOMY
Symptoms and physical manifestations of vasospastic disease can be caused by or complicated by (a) occlusive events (thrombosis and embolism) or vasospastic disorders, (b) abnormal vasomotor control after trauma with or without occlusive events, (c) collagen vascular disorders, or (d) a combination of the above. Raynaud’s phenomenon and inappropriate vasospasm can produce pain, intolerance to cold, and functional impairment. When the phenomenon is associated with occlusive events, ulcers may result and progression to gangrene may occur. Patients who experience vasospasm after posttraumatic, acute thrombosis or embolism can benefit from digital sympathectomy when arterial damage is not reconstructible, collaterals are inadequate, or multilevel arterial damage is present (2,6,11,12,13,14,15,16,17,18,19,20,21,22).
Specific Indication for Digital Arterial Sympathectomy
To manage refractory vasospasm and inappropriate arteriovenous shunting in patients with vasospastic or vasoocclusive disorders under the following conditions:
Refractory symptoms that continue in spite of appropriate medical management
As an adjunctive treatment to compliment arterial reconstruction or resection and ligation in patients with occlusive disease
In patients with collagen vascular disease and refractory vasospastic symptoms with physical findings secondary to Raynaud’s phenomenon
For treatment of nonhealing digital ulcers or sores
As an adjunct to digital amputation in patients with vasospastic disorders in order to facilitate healing
Contraindications
Nonsalvageable distal structures should be amputated.
Patients with atherosclerotic peripheral vascular disease with vessel calcification and irreversible vasospasm.
Calcific arteritis with minimal or no response to vasodilators
Atherosclerotic disease associated with dialysis
Atherosclerotic Buerger’s disease without significant vasospastic disorder
Gross infection.
Concern over patient safety because of medical comorbidities.
PREOPERATIVE PREPARATION AND EVALUATION
Comprehensive history (2)
Document details of any trauma
Documentation of familial or personal coagulation issues
Drug use, especially intra-arterial/intravenous
Exposure to and/or use of smoke or smokeless tobacco products
Familial or personal history of collagen vascular disease
Symptoms and signs including pain, cold tolerance, swelling, digital color changes, sores or ulcers, and delayed wound healing
Triphasic digital color changes; the frequency and duration of color changes must be documented.
Physical Examination (2)
Evaluation of the neck and entire upper extremity
Assessment of capillary refill, turgor, and integrity of skin and nails
Evaluation of peripheral pulses
Allen test
Evaluation to determine the presence of thoracic outlet syndrome
Additional Testing