Fig. 3.1
Plain film of the great toe demonstrates typical plain film findings of osteomyelitis including cortical erosion and destruction at the medial tip of the distal phalanx, lytic changes, and destruction of the trabecula in the proximal portion of the bone, soft tissue swelling, and air in the soft tissues
There can be false positives when the patient has an underlying arthropathy or neuropathy which can mimic the findings of osteomyelitis on plain films [2]. For this reason at our institution, many patients with positive X-rays still go on to have an magnetic resonance imaging (MRI) in order to delineate the extent of disease and soft tissue findings prior to surgery.
Computed Tomography
Computed Tomography (CT) is not frequently used for diagnosis of early osteomyelitis as it shares several of the deficiencies associated with radiographs. Early osteomyelitis which has not yet progressed to cortical destruction is not well seen and thus CT is not particularly sensitive in early osteomyelitis. In addition, CT has a high radiation dose relative to the clinical information, which can be obtained, and thus CT is primarily used in patients who have a contraindication to MRI scanning. The findings of osteomyelitis on CT are similar to those seen on radiographs and include trabecular rarefaction, cortical destruction and erosion, and periosteal reaction. These findings are often seen in better detail on CT scan than on X-rays due to the thin slice thickness. In addition, small pockets of gas can be seen and CT can often identify fluid collections when they are not visible by X-ray [5, 6].
Nuclear Medicine Scans
Technetium 99m Phosphate Bone Scans
Bone scintigraphy is a very sensitive test and is usually performed as a three-phase study. The patient is injected with Technetium 99m-labeled diphosphonates, usually methylene diphosphonate (MDP), and images are obtained immediately after injection for a dynamic flow phase. This is followed with static images during an immediate blood pool phase and then delayed imaging 2–4 h later for a bone phase. Focused spot views are very helpful when evaluating the foot and ankle. On a 3-phase bone scan hyperfusion, hyperemia, and focal increased uptake in the bone of interest are seen with a diagnosis of osteomyelitis (Fig. 3.2a–c). The scan will be positive in early phases of osteomyelitis within 24–48 h of initial symptoms. Although the sensitivity of bone scan is reported at 80–90 % in multiple studies [7, 8], the specificity is much lower and is closer to 50 % in multiple studies [9–12]. A meta-analysis by Termaat et al. found a pooled specificity of 25 % for bone scintigraphy [13]. The binding of the 99mTc-MDp to the hydroxyapatite in the bone is responsible for the radiotracer uptake and thus any condition which causes bone turnover with osteoblastic activity will demonstrate increased radiotracer uptake on a bone scan. Disease processes such as neuroarthropathy, fracture, prior surgery, or malignancy can all cause a false positive bone scan in a patient who is being evaluated for osteomyelitis. In addition, the lack of anatomic detail on bone scan can make exact delineation of extent of disease difficult.
Fig. 3.2
3-Phase bone scan demonstrates typical findings of osteomyelitis. (a) Blood flow image, (b) blood pool image, and (c) delayed image all demonstrate increased uptake of Tc 99m MDP in the region of the base and proximal right fourth metatarsal
Given the known lack of specificity, Jay et al. evaluated whether the results of the bone scan, either positive or negative, affected amputation rates or clinical treatment and found that there was no difference in treatment or in amputation rates based on whether the bone scan was positive or negative. Jay et al. recommend that bone scan not be used in evaluation of foot and ankle osteomyelitis due to its lack of specificity and unlikely effect on treatment decisions [14].
For these reasons, bone scan is not often used as the imaging method of choice following plain films; however, 3 phase Tc99m-MDp scanning remains a reasonable imaging technique in patients who cannot have an MRI particularly if they do not have underlying arthropathy or neuropathy or a recent history of trauma.
Labeled White Blood Cell Scans
Indium-labeled leukocytes have been used extensively for evaluation for osteomyelitis. The radiolabeled white blood cells accumulate at the site of infection and will not accumulate in locations without infection such as fractures, malignancy, or neuropathic joints. This makes labeled white cell scans particularly useful in diagnosing osteomyelitis in patients with underlying neuropathic joints. The sensitivity of the test reported in the literature extends from 72 to 100 % [12, 15, 16]. Despite the high sensitivity the Indium-labeled leukocyte study has disadvantages that include a 24-h waiting period before imaging can begin as well as low resolution of the images which makes it difficult to determine the exact location of the osteomyelitis (Fig. 3.3). Schauwecker et al. used a concurrent bone scan for determining anatomic location and found improved sensitivity and specificity with a sensitivity of 100 % and a specificity of 83 % [17]. There can be false positives as well due to the accumulation of white cells in the infected soft tissues and the fact that low anatomic resolution can make exact location of infection difficult to determine.
Fig. 3.3
Indium-111-labeled white blood cell scan performed on the patient who had the bone scan in Fig. 3.2. Focal uptake of Indium-labeled white cells seen in the same region of the foot confirms osteomyelitis. Lack of anatomic detail makes delineation of location of uptake difficult without the bone scan which was performed contemporaneously
Technetium 99m hexamethylpropylamine oxine (HMPAO)-labeled leukocytes are also used and are more cost effective than Indium-labeled cells. Tc-99m HMPAO scanning is also based on the accumulation of white blood cells at sites of infection and thus it shares the advantages of higher specificity due to lack of accumulation in patients with arthropathy, neuropathy, and trauma that Indium scanning has. In addition, it can be performed and completed on the same day, allowing for a more timely diagnosis than Indium white blood cell scanning affords. The sensitivity of the exam is between 85 and 90 % [9, 11]. Despite high sensitivity and specificity of the labeled white cell scans, these are still usually a problem-solving technique used in unusual situations such as patients with extensive hardware which cannot be imaged by MRI or in patients with equivocal findings by other imaging modalities due to underlying neuropathic changes.
Positron Emission Tomography Imaging
Positron emission tomography (PET) has also been studied as an emerging tool for the evaluation of osteomyelitis. PET scans are very expensive and not available in many hospitals on a routine basis and thus PET is unlikely to become a mainstay of imaging for the infected foot and ankle. PET scanning involves injection of fluorodeoxyglucose (FDG). Metabolically active tissues including infected tissues use more glucose and thus accumulate more radiotracer. Data regarding the sensitivity and specificity of PET scans is variable. Nawaz et al. compared PET, MRI, and plain films in patients with diabetic foot ulcers. They found a sensitivity of 81 % and a specificity of 93 % for PET and a sensitivity of 91 % and specificity of 78 % for MRI. They concluded that PET scan is a reasonable alternative in patients who have a contraindication to MRI scanning [3]. Kagna et al. found that PET/CT had a sensitivity of 100 % with a specificity of 93 % for diagnosis of osteomyelitis in the diabetic foot [18]. Basu found that PET was very useful in diagnosing infection in patients with underlying Charcot foot and PET had a sensitivity of 100 % in this setting in comparison to MRI which had a sensitivity of 76.9 % in the setting of Charcot [19]. Although these researchers found high sensitivity for PET, there are conflicting data in the literature. Familiari found only 43 % sensitivity and 67 % specificity for PET/CT [20]. The data are discordant and it is uncertain as to why these scientists have obtained dramatically different results [21]. Given these conflicting data, PET is best used in complex situations in which standard imaging techniques such as MRI and white blood cell scanning cannot be performed easily.
Magnetic Resonance Imaging
MRI is usually the preferred method of imaging for diagnosis of osteomyelitis. MRI is widely available, fairly quick to perform in most centers, and does not use radiation. In addition, scans can be obtained in multiple anatomic planes. MRI images have excellent spatial resolution and are very useful for evaluation of bone marrow as well as of soft tissue structures providing significantly more anatomic detail than nuclear medicine scans. The anatomic detail is helpful in defining the extent of disease which is very important to surgical planning. MRI is also very useful in depicting soft tissue complications in addition to bony involvement. MRI demonstrates abscesses, tendon involvement, and cellulitis with much greater detail than US or CT [22]. Finally MRI has been shown to be cost effective [23].
A standard MRI of the extremity for evaluation of osteomyelitis usually involves a combination of T1 weighted and T2 weighted sequences in multiple anatomic planes as well as imaging after intravenous administration of a gadolinium contrast agent. The exam should be tailored to the site of ulceration and suspected infection. Dedicated smaller field of view imaging of the forefoot or hindfoot is preferable to using a larger field of view in an attempt to include the entire foot and ankle in one exam. Given the size of most feet, the large FOV required to include the entire foot and ankle leads to a decrease in resolution of smaller structures such as the smaller bones of the midfoot and forefoot. This renders the study less useful since less anatomic detail is available. A dedicated extremity coil designed for the foot and ankle should be utilized.
At our institution the exam includes sagital short tau inversion recovery (STIR) images and sagital T1 weighted images, coronal T1 weighted images, and coronal FSE T2 weighted images with fat saturation, axial T1 weighted images, and axial FSE T2 weighted images with fat saturation. The coronal images are helpful for visualization of ulcerations along the plantar aspect of the forefoot. The relationship of the ulcer to the underlying bone is well seen on coronal imaging. The coronal images are also useful for evaluation of the marrow. Sagital imaging often demonstrates calcaneal ulcerations better than the coronal or axial imaging. Use of fat saturation is important on the T2 weighted exams so that marrow edema can be adequately visualized. Frequently in the distal toes the fat saturation is uneven and thus the bone marrow appears high signal on the T2 weighted images which renders diagnosis of marrow edema impossible. During scanning if the fat saturation in the toes is not adequate, STIR imaging can be substituted for the fat suppressed T2 weighted images. STIR imaging often is lower in resolution but it does not rely on chemical fat saturation and thus can be very useful for visualization of marrow edema particularly in the distal phalanges.
The majority of cases of osteomyelitis in the foot result from direct spread of infection from an ulcer in the skin down into the soft tissues and to the bone. These ulcerations typically occur in patients with diabetes who have developed peripheral neuropathy due to microvascular disease. The vascular disease both causes the neuropathy and also causes impairment in wound healing which predisposes the patient to ongoing infection at the site of the open ulcer. The distribution of foot ulcers depends to some degree on gait and activity and will vary from patient to patient; however, the vast majority of ulcers in the forefoot occur at the fifth metatarsal, first metatarsal, and at the distal phalanx of the great toe. In the hindfoot, the calcaneus is the bone which is most frequently affected. Ledermann et al. demonstrated in a study of 161 ft in 158 patients there were 130 cases of osteomyelitis. Of these 130 cases of osteomyelitis, all but one spread from a skin ulcer or defect down to the subjacent bone [24].
Callus formation is often a precursor to ulceration and calluses are seen frequently in diabetic patients. The distribution of callous is similar to the sites of maximal skin pressure. Thus, calluses are seen in the feet under the metatarsal heads, adjacent to the first metatarsal base, and in patients with a neuropathic foot adjacent to the cuboid. Calluses appear on MRI as soft tissue prominences which are focal and low signal on T1 weighted scans with variable signal on T2 weighted scans. The variability of the signal on T2 weighted scans is due to the variable amount of granulation tissue and inflammation in the callus. The callous will often enhance and care must be taken not to confuse the enhancing callous with focal infection. Repeated micro-trauma to the callus can result in an ulceration in the callus which as described above is often slow to heal in diabetics with vascular disease [25].
Ulcerations on MRI appear as a skin defect often with heaped up margins due to the presence of an underlying callus. The ulcerations are often high signal on T2 weighted scans due to surrounding infection and cellulitis and they will often enhance avidly as well. The ulceration can extend down to the surface of the bone or alternatively a sinus tract may be present extending from the ulceration to the surface of the bone. The presence of an ulcer and the contiguous abnormal signal extending from the ulcer to the bone is a hallmark finding in the diagnosis of osteomyelitis by MRI [26, 27] (Fig. 3.4). The presence or absence of an ulceration can help differentiate marrow edema related to osteomyelitis from reactive marrow edema or marrow edema related to other causes such as stress reaction or trauma. In patients without an ulcer, marrow edema in the bone is less likely to represent osteomyelitis [26, 27].
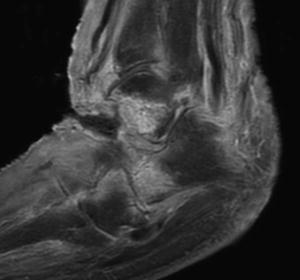
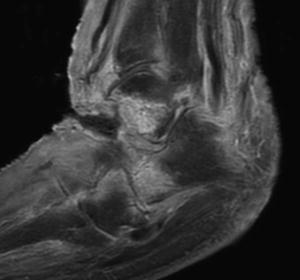
Fig. 3.4
Soft tissue ulceration over the dorsum of the foot extending down to the talus. Erosion of the talus with cortical destruction and marrow enhancement. Extensor tendons are also disrupted
Diagnosis of osteomyelitis by MRI is made by identifying abnormal marrow in the bone that is typically signified by low signal replacing the marrow on T1 weighted scans and high signal in the same location of T2 weighted scans. Enhancement of the bone on fat suppressed T1 weighted images can also be useful in making the diagnosis. Marrow signal changes are always present in osteomyelitis but can also be present due to other disease processes such as reactive edema secondary to inflammation, trauma, stress reaction, or tumor. There are several factors that can help differentiate marrow edema secondary to osteomyelitis from marrow edema related to one of these other causes. These factors include presence of an ulcer with extension to the bone as well as the relative signal intensity of the edema, confluence of the abnormal signal, and presence of the abnormal signal on more than one type of sequence [27, 28] (Fig. 3.5a–c).
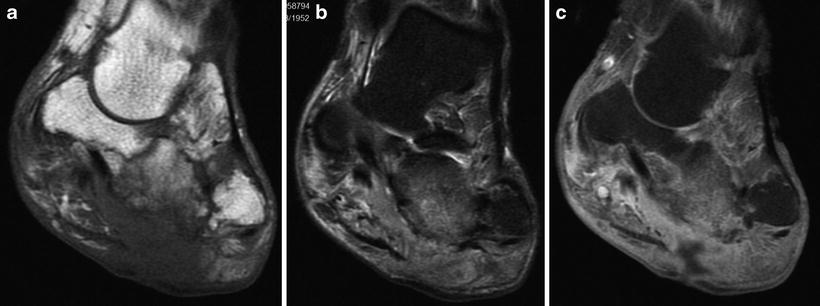
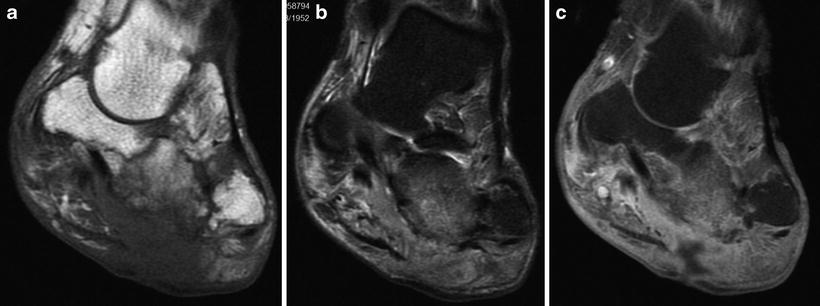
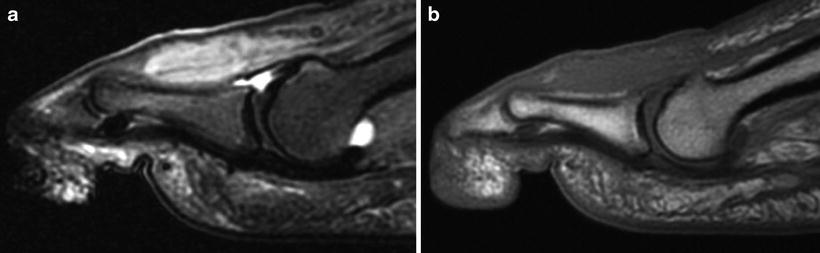
Fig. 3.5
Diabetic patient with foot infection and an ulceration deep to the cuboid. (a) On the T1 weighted image, there is abnormal signal within the marrow and cortical destruction. On the T2 weighted image, (b) there is marrow edema in the cuboid. (c) A sinus tract extends down to the bone and the bone enhances post gadolinium administration. Diagnosis is aided by the presence of the ulceration as well as of abnormal signal on multiple sequences
On T1 weighted imaging, the signal in cases of osteomyelitis is lower than the normal marrow and typically isointense or hypointense to the musculature [28]. The marrow changes on the T1 weighted images are due to infiltration of the marrow by infection with replacement of the normal marrow with pus and necrosis. Features of the abnormal T1 weighted signal that are highly correlated with true positive cases of osteomyelitis include a geographic medullary distribution of the abnormal signal as well as a confluent pattern of the abnormal marrow signal [29] (Fig. 3.6a,b). Collins et al. found that in 100 % of their study cases with surgically proven osteomyelitis there was decreased signal in the marrow on T1 weighted scans in a geographic distribution and a confluent pattern with T2 marrow signal intensity in the same location [29]. Johnson et al. confirmed these findings and found that in 19/20 cases of confirmed osteomyelitis, decreased marrow signal on T1 weighted images was present with a geographic distribution and confluent pattern. None of the cases of confirmed osteomyelitis in this study had hazy reticulated abnormal signal on the T1 weighted scans. The sensitivity of the combination of the findings of geographic distribution of abnormal signal and confluent pattern of abnormal signal was 95 % and the specificity was 91 % in this study using T1 weighted imaging features alone [28]. Morrison et al. also found that using the abnormal signal on T1 weighted scans yielded an average sensitivity of 92 % and a specificity of 86 % [26].
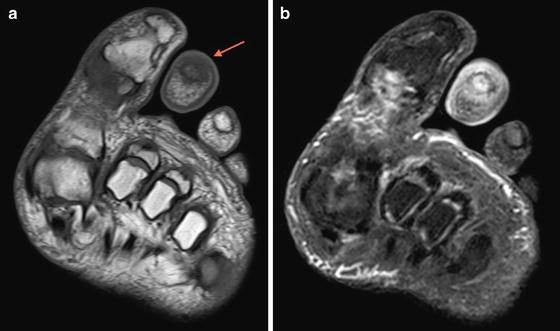
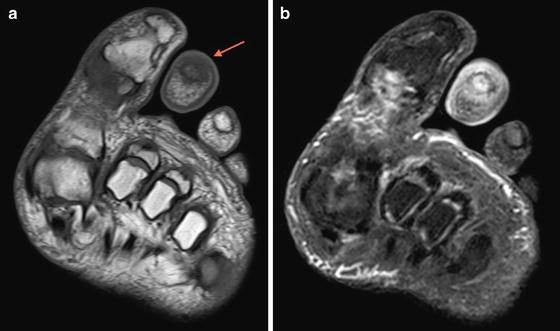
Fig. 3.6
T1 weighted axial image (a) of the toes in a patient with osteomyelitis demonstrates low signal in the marrow of the second distal phalanx completely replacing the normal bright fatty signal (arrow). Normal marrow signal can be seen for comparison in the distal phalanges of the first and third toes. Coronal T2 weighted image (b) of the toes demonstrating concordant increased T2 signal in the second distal phalanx
In several studies the presence of abnormal signal in the marrow on T1 weighted scans which has a hazy or reticulated pattern is more suggestive of reactive marrow edema than of osteomyelitis [26, 27, 29, 30]. On T2 weighted scans osteomyelitis is visualized as increased signal due to marrow edema at the site of infection. Marrow edema on the T2 weighted scans is a nonspecific finding as there are many conditions beside osteomyelitis which can also cause increased signal on the T2 weighted scans [27]. Frequently in patients with soft tissue ulceration there will be reactive marrow edema in the adjacent bone. This will typically be reticulated in appearance and less confluent that marrow edema secondary to osteomyelitis. It is helpful to review the T2 weighted scans in conjunction with the T1 weighted scans. When patients have normal signal on the T1 weighted scans and edema on the T2 weighted scans, osteomyelitis is less likely to be present than if the marrow is abnormal on both T1 weighted scans and T2 weighted scans [29] (Fig. 3.7a,b). The T2 weighted scans are also particularly useful when they are normal as normal marrow signal on T2 weighted imaging excludes the diagnosis of osteomyelitis [27].