Design of the Trauma Operating Room
Richard Leslie George
Arpan K. Limdi
For many surgeons, getting involved in a major building project is a once-in-a-lifetime experience. Our focus throughout this chapter is to educate the reader about the core concepts and current trends in planning, design, and medical technology surrounding the operating room (OR) environment. In understanding the language, asking the correct questions, and providing the answers the consultants seek, the opportunity to build a durable and functional facility that embodies the visions of all members of the design team is realized. Furthermore, understanding the points along the project timeline beyond which the process cannot be revisited will set forth appropriate goals and expectations. In so doing, the reader will be a more effective leader in the design process.
The 2007 Construction Survey conducted by Health Facilities Management and the American Society of Healthcare Engineers (ASHE) indicates a significant and sustained surge in hospital construction activity.1 Ongoing construction in excess of $40 billion is addressing aging facilities, accommodating new technology, providing larger private patient rooms, improving operating efficiency, and responding to population-based demand and competition.1,2,3,4,5 In its 2006 survey, more than 20% of responding hospitals indicated ongoing construction projects in emergency departments (EDs) and surgery suites, with another 25% indicating plans within 3 years; areas of specific interest to this reader.6 Flexibility, modularity, evidence-based design, and infrastructure for emergencies are the significant criteria driving the planning and design of new facilities.1,2,7,8 With building costs in 2007 exceeding $300 per sq ft (and approximately twice as much in California to address new seismic requirements), the development of a new OR suite is a significant economic investment for a health care institution.1,9,10 Providing thoughtful and well-balanced input into this process will help the institution make optimal use of the usually limited capital funds.3,11,12,13
OVERVIEW OF THE PLANNING, DESIGN, AND CONSTRUCTION PROCESS
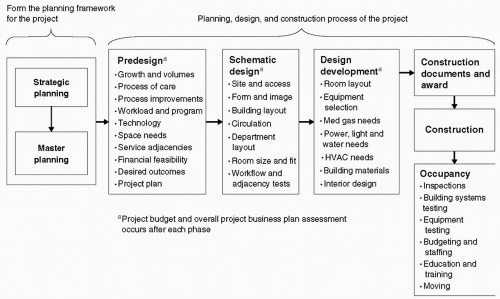
The planning, design, and construction process, shown in Fig. 1, may be broadly organized into six categories: strategic planning, master planning, predesign, design and award, construction, and occupancy.
Strategic Planning
On the basis of institution’s vision and mission, strategic planning is the process through which the institution comprehends its situation in the context of its environment, defines key organizational objectives to achieve its vision, and develops broad strategies to achieve these objectives.14,15 In simpler terms, the strategic plan establishes the criteria and parameters around which business decisions are made by the institution.
Master Planning
Before initiating a significant building program, it is necessary to assess whether the physical and functional design of the facility provides an appropriate, effective, and efficient environment to satisfy the mission and strategic plan of the institution.3,16,17,18 The master planning process incorporates this assessment, identifies assets and constraints associated with the environment, and develops the actions
necessary to address the constraints and implement the planned business initiatives.3,16,19 Integrating the physical and functional evaluation with the future needs of the institution leads to a facility master plan that defines the overall planning criteria and articulates the highest and best use of available resources.20 The facility master plan defines broad initiatives such as land acquisition, parking development, building replacement, and utility capacity development to accommodate projected future needs.20,21 The master plan is reviewed and updated on a regular basis along with the strategic plan and the associated financial plan.3,12
necessary to address the constraints and implement the planned business initiatives.3,16,19 Integrating the physical and functional evaluation with the future needs of the institution leads to a facility master plan that defines the overall planning criteria and articulates the highest and best use of available resources.20 The facility master plan defines broad initiatives such as land acquisition, parking development, building replacement, and utility capacity development to accommodate projected future needs.20,21 The master plan is reviewed and updated on a regular basis along with the strategic plan and the associated financial plan.3,12
Predesign
Planning for a specific project begins with the predesign process. In essence, this is the phase in which the specific needs and desired outcomes associated with the project are defined within the broader context of the strategic plan and facility master plan. Activities undertaken during predesign include more detailed facility and operational assessments, assessment of demand, development of growth projections, a financial feasibility study, and determination of project goals.15,17,19,20 Once the financial and operational viability of the project is established, the team proceeds with development of the program.15,20
Program development involves determination of workload followed by preparation of the functional program, space program, and conceptual building plan.17,22 The project implementation plan, preliminary project budget, and project schedule are also developed at this time.16,19,23 Medical and communication technology planning traditionally occurs during the design phase; however, it is important to identify transformational technologies (that have significant impact on care processes and outcomes) to be included in the project.
Determination of a design and construction delivery method is necessary to establish the project implementation plan. Design-award-build is the traditional method of project delivery based on a clear, formal, and standardized process.16 Other options for project delivery focus on managing financial risk and accelerating implementation schedules. An increasingly common approach is for the owner to retain a construction manager (CM). The CM may work with the owner and architect to coordinate the design and then become the general contractor (often guaranteeing cost and schedule) or continue to manage the construction by coordinating with a builder on behalf of the owner.16 The CM approach allows the team to benefit from the contractor’s expertise in several areas such as building methods, prevailing costs, and early purchase of long-lead items.16,19,24
Design
Design is the process where the solution to address the needs specified during predesign is synthesized. Design activities are organized into two phases—schematic design and design development. The image, form, size, structural
grid, and circulation plan of the building (project) are established during schematic design. The size, location, and arrangement of functional areas and building utility systems are also established at schematic design.16,19 Each individual space in the building program is located within its assigned functional area using the size, dimensions, and desired adjacencies described in the functional program. However, not all desired adjacencies are achievable. A primary purpose of the schematic design review with the owner is to evaluate the developed plans against the desired functional program. Solutions for individual rooms or services that do not fit expectations are developed by reevaluating program, size, workflow, and prioritizing adjacencies.19 A schematic level budget estimate is also prepared and titrated against the desired scope, proposed design, and the financial plan.
grid, and circulation plan of the building (project) are established during schematic design. The size, location, and arrangement of functional areas and building utility systems are also established at schematic design.16,19 Each individual space in the building program is located within its assigned functional area using the size, dimensions, and desired adjacencies described in the functional program. However, not all desired adjacencies are achievable. A primary purpose of the schematic design review with the owner is to evaluate the developed plans against the desired functional program. Solutions for individual rooms or services that do not fit expectations are developed by reevaluating program, size, workflow, and prioritizing adjacencies.19 A schematic level budget estimate is also prepared and titrated against the desired scope, proposed design, and the financial plan.
The design development phase takes the approved schematic design further to a level of detail necessary to describe the project for construction. The workflow within and between rooms is finalized, and medical equipment and associated utility systems required within each room are selected. The lighting, power, water, and medical gas requirements along with the heating, ventilation, and air-conditioning (HVAC) system requirements for each space are defined. Detailed design of the building interiors is undertaken, and building materials, interior finishes, and furnishings are selected and specified.16,19 All this information is recorded on room data sheets prepared for each space within the building program.16 Detailed drawings (floor plans, reflected ceiling plans, room elevations, and sections) and specifications are prepared from the gathered information showing the size, exact dimensions, exact location, and installation requirements for the items specified on the room data sheets.16,19 The design team also prepares an updated project cost estimate to evaluate against the available project budget. With owner approval of the design development drawings and specifications, the team proceeds with preparation of construction documents. Any changes to the project scope and program after completion of design development will cause additional design expenses. In addition, if the changes are significant, it may also extend the project schedule and increase the cost of the project.
Construction Documents, Bidding, and Award
Construction documents or contract documents form the basis for a legally binding agreement between the owner and a builder to construct the specified project within a specified time and for a specified cost.16,19,23 The documents consist of drawings, specifications, and general contract conditions. Contractors use the bid documents and issued addendums to determine the construction cost (and their profit), schedule, and means and methods of building the project. The owner and design team review bids or negotiate with interested builders to obtain the lowest responsible and fair cost and appropriate quality of construction for the project.16,19,23 Changes in scope, program, or design after contract award will cause significant increases in the construction cost and delay the completion date of the project.
Construction and Occupancy
During the construction process, the owner’s team is responsible for several issues. Construction progress is monitored against the schedule. The contractor’s pay requests are reviewed against progress and approved for payment. Field inspections are performed to assure quality of construction and conformance to specifications. Changes to the design or specified materials, requested by the builder or end users, are evaluated and addressed. The specification, bidding, evaluation, award, and installation of owner-provided furnishings and equipment are also undertaken.
Another important set of activities for the owner’s team is preparing the end users to take occupancy of the project at its completion. Occupancy planning involves orienting staff to the new facility, training to operate new systems, developing budgets, hiring staff, developing new procedures, and performing preoccupancy testing of clinical systems. The relocation plan for existing departments and the activation plan for the new facility is developed and communicated. Special attention should be placed on testing the environment for mold and spores, and if applicable, moving critically ill patients. For large building projects, a commissioning agent is hired to test, balance, and tune all electrical and mechanical (another term referring primarily to HVAC) systems; to prepare building systems documentation; and to provide enhanced training to facility maintenance staff.25 Tuning building automation systems to produce energy efficient operations right from building start-up can avoid significant unnecessary expenses for an institution.25
GETTING ORGANIZED FOR THE PROJECT
Activities necessary to get organized for the project include selecting consultants, organizing the owner’s project management team, and developing a project management and decision-making structure. With the team in place, the project delivery plan is developed and the predesign process can begin.16,19,23,26
Selecting Consultants
Selecting well-qualified and experienced professionals is essential to a successful building project. Key members of this team include the programmer or functional planner, the architect and associated engineers, and the contractor
or CM. Additional criteria to evaluate include skill and experience, size of the firm and proposed team, knowledge of local conditions, commitment to the project, and their design fee. Consider the experience of not only the principals but also the staff that will be handling the bulk of the project development. Other consultants who may be necessary for the project include medical equipment planners, communication system planners, the developers or development consultant, financial consultants, and cost estimators.
or CM. Additional criteria to evaluate include skill and experience, size of the firm and proposed team, knowledge of local conditions, commitment to the project, and their design fee. Consider the experience of not only the principals but also the staff that will be handling the bulk of the project development. Other consultants who may be necessary for the project include medical equipment planners, communication system planners, the developers or development consultant, financial consultants, and cost estimators.
The Owner’s Team
The owner’s team, at a minimum, is represented by three groups—the project management team, the end users, and administration. The project management team is responsible for all aspects of the administration of the project. It should be staffed by individuals with extensive experience in planning, design, and construction of facilities. Physicians, nurses, and allied health professionals are the end users who will utilize the facility. They should be heavily involved in the planning and design of the project. Administration is responsible for setting direction and making all final decisions on the project.
A comprehensive view of the clinical and functional requirements from a multidisciplinary perspective is necessary to develop an effective surgical suite design.23 Therefore, be as inclusive as possible without making the team dysfunctional. In addition, tailor the structure of the team to the complexity of the project and to complement the social and operational dynamics of the organization. Being knowledgeable about workflow and paying attention to details are two important attributes necessary for members of the user team. To be effective, the teams need to develop trust and a sense of ownership in the process and design, eventually becoming strong advocates for the design.
Guiding Principles
At initiation, the executive team and key stakeholders should be clear about the objectives of the project. The strategic and financial plans, coupled with the facility master plan, provide the framework to define these objectives. A set of planning and design principles derived from the objectives should be used in evaluating options and making decisions throughout the course of the project.23 Some of the common themes driving the current building boom are discussed in the subsequent text:
A predominant theme that will continue for several years is the need to address aging facilities while incorporating flexibility for the future.1,16,17,27 For facilities built in the 1950s and 1960s, right-sizing and reorganizing core diagnostic and treatment space are essential to accommodate new technology, improve operational efficiency, address competition, and maintain marketshares.1,2,8,28
Patient care spaces built using a standards-based, modular design approach experience construction cost reductions, assure operational flexibility, bolster patient safety, and ease adaptation in the future.29
Medical technology has served as one of the major drivers of innovation in health care. These innovations are powering significant improvements in patient outcomes, productivity, and efficiency. However, due to rapid improvements, the useful life of major technologies (telecommunication systems, imaging, laboratory, pharmacy, and surgery) has shortened considerably. Therefore, planning for future flexibility in replacing technology has become a core guiding principle of building projects.16
There is a trend toward utilization of an evidence-based design approach reflecting an increasing level of maturity in the health care design process. Features such as larger private rooms with family space, introduction of natural light and nature into the care environment, improving ceiling design, introduction of art and color, and taking active measures to reduce noise levels are results of studies conducted, showing their beneficial effects on patients, family, staff, and revenues.30,31
Building project costs are rising at significant rates beyond inflation.10 Health care institutions are caught between reduced reimbursement for services rendered and greater (and justifiable) demands for safety and efficiency (which require improved workflow and new technology).3 Investment in the physical plant is essential, but the financial outlook is negative (reduced revenues from operations, deteriorating debt capacity, and lower bond ratings). Therefore, to extend the reach of available funds, executives are exploring functional flexibility through multiuse procedure spaces and acuity adaptable or universal patient rooms. In addition, heretofore unglamorous (but expensive) areas such as building structure, emergency generators, power plants, utility systems, and wiring conduit are also being planned with future expansion in mind.
THE PREDESIGN PROCESS
From the owner’s perspective, most significant operational and financial decisions related to a project occur during the predesign or programming phase of the project.11,17,23 The axiom “form follows function” is central to the planning of health care facilities, and the definition of function begins in the predesign process.11 The tendency to begin drawing once the architect is selected should be curbed until the predesign process is completed. As reviewed in section II, the predesign process has several activities, which we will expand upon in this section.
Physical and Operational Assessment
For a renovation project, the assessment of existing physical, operational, and environmental conditions is
an important task. As standards of care and technologies evolve, facilities accrue deficiencies requiring operational workarounds. Issues to evaluate in the existing OR include size; power, communication, and medical gas capacity; HVAC capacity and performance; and the ability to locate and power larger imaging equipment. Issues to evaluate in the existing surgery suite include preoperative holding and recovery capacity; equipment, instrument, and supply storage capacity; location and adjacency of key support services; and the workflow of patients, sterile supplies, and soiled goods. This evaluation, conducted by the architect, functional planner, or medical programmer, is best handled through tours, interviews, and a well-organized questionnaire system.22
an important task. As standards of care and technologies evolve, facilities accrue deficiencies requiring operational workarounds. Issues to evaluate in the existing OR include size; power, communication, and medical gas capacity; HVAC capacity and performance; and the ability to locate and power larger imaging equipment. Issues to evaluate in the existing surgery suite include preoperative holding and recovery capacity; equipment, instrument, and supply storage capacity; location and adjacency of key support services; and the workflow of patients, sterile supplies, and soiled goods. This evaluation, conducted by the architect, functional planner, or medical programmer, is best handled through tours, interviews, and a well-organized questionnaire system.22
Scope of Program
To develop the appropriate functional program, space program, and required adjacencies, the medical planner needs to develop an understanding of the scope and extent of the trauma program. Some of the key questions to address include the following:
Is the trauma program a Level I or II service within the community?32 Is there a full-time trauma surgical service at the institution?33 Is the institution the only significant community resource for trauma care?
Who are the other providers of trauma service in the local and regional geographic area? What level of service do the other providers support? Is this expected to change in the short- to medium-term future?
How does the local or regional emergency management system operate?
Are there any specific community social and behavioral trends that dictate specific arrival patterns to the trauma service?
What are the demographics of the geographic area serviced by the institution? What are the long-term population trends? Are there seasonal and peak demand trends?
What are the surge capacity requirements in the event of a mass casualty event?32
What are the current and projected trauma patient volumes expected at the institution?
Answers to such questions (or a consensus, where clear data are not available) are used by the medical planner to understand future population trends, and develop volumes and capacity requirements for the functional and space programs.
Workload Projection
The number of ORs (or any other key room) is generally determined by the projected volumes for each type of procedure, the average length of each type of procedure (turnaround time) coupled with the hours of operation of the surgical suite, and a proposed utilization (or efficiency) factor.22,32,34,35 A trauma surgery suite should be able to handle all emergency general surgery procedures. Institutions can elect to configure their ORs so that a trauma surgical procedure can be performed in any OR. However, for hospitals with a large trauma population, it would be advisable to have a block of rooms (on the basis of projected volumes) dedicated to trauma surgery. One OR should always be kept ready and available to handle emergency procedures. These arrangements not only assure availability of resources in critical situations, but also allow optimization of workflow, and improvements in efficiency and delivery of patient care for the entire surgical service.
Functional Program
The functional program is a detailed document that describes the planned future functions and operations of a service or department.27 The program documents existing care processes, associated inefficiencies, future care processes, and associated improvements. A thorough understanding of workflows (patients, staff, and materials), operating metrics, shared resources, critical adjacencies, and special design concepts is assimilated and documented in the functional program.22,27,36 Analyzing routine tasks, eliminating redundancies, and optimizing workflow can produce operating efficiency, additional capacity, and improved financial performance.27,37,38,39
The nature of the surgical disease of trauma mandates critical management. Rapid and timely access to resources is essential to successful management of a trauma service patient. In the development of efficient workflow, it is important to understand that the ED, the trauma bay, the OR, the postoperative care unit, the intensive care unit (ICU), and the surgery ward form an interdependent system through which the trauma patient will transit during their stay at the hospital.40 Separating urgent surgical cases from the scheduled case workflow will significantly improve the throughput for both areas.40
There are several functional adjacencies to consider when planning a trauma program. Intake to the trauma surgical service generally occurs from the ED or a specified trauma unit within. Access to the ED and OR by helicopter and ambulance through dedicated circulation (including large elevators when required) facilitates timely and efficient patient flow. The adjacency of the principal care delivery spaces such as the ED, ICU, and OR is also an important functional planning consideration. Within the ED, the location of decontamination facilities;32 location of the trauma pod and adjacency to dedicated imaging services; and adjacency to supply and medication rooms requires careful consideration. In the OR environment, location of ORs to large trauma elevators; quick access to the blood bank, pharmacy, anesthesia laboratory, and portable imaging equipment; and adjacency to the computed tomography (CT) service should be considered.
Associated adjacencies important to successful operation of the trauma suite include location of postanesthetic care unit (PACU) (recovery); location of sterile instrument trays and supplies; and location of central supply services where instruments may be washed, packed, sterilized, and transported to and from surgery.
Associated adjacencies important to successful operation of the trauma suite include location of postanesthetic care unit (PACU) (recovery); location of sterile instrument trays and supplies; and location of central supply services where instruments may be washed, packed, sterilized, and transported to and from surgery.
Space Program
For large projects, space program development occurs at a conceptual level and is followed by a detailed, roomby-room development. The conceptual space program is a rapid method for the programmer to establish the total space need. The method is based on multiplying the total number of revenue generating spaces planned, also called key rooms (e.g., the OR), by a space assignment factor which incorporates the size of the key room as well as the size of all support spaces needed to make it functional. The factor most commonly used for this activity is the department gross square feet (DGSF) factor. Space needs for a surgery department are estimated using a factor ranging between 2,700 DGSF per OR and 3,500 DGSF per OR. The conceptual space program provides the design architect initial feedback regarding the total size of the project (building), and serves as a benchmark for the development of the detailed space program.
The detailed building or space program is a roomby-room space list organized by department, service, functional area, or building component. The program tabulation, prepared by the medical planner (or programmer), shows name, number, size, and purpose of all rooms, spaces, areas, and services to be included in the project and necessary to address the needs defined in the functional program.22,34,35 A brief narrative describing the character of the key space and the criteria used to establish its size may be included in the tabulation.16,19,22 The size of individual rooms in the space program is shown in net square feet (NSF). NSF represents the clear usable space within the walls of the room. Medical planners generally apply two factors to the total NSF of a department or functional unit. The first factor converts the NSF to the DGSF, which accounts for the space for walls, internal circulation, and interior building structure. A second factor is applied to the DGSF to account for common building areas such as lobbies and atria, primary building circulation, inter-departmental circulation, elevators, stairwells, mechanical and electrical shafts, and telecommunication risers.16,22,41
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree