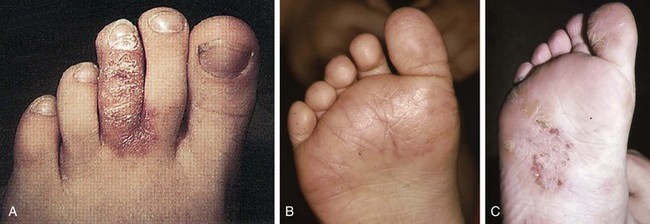
Chapter 16 Atopic dermatitis describes the spectrum of red, scaly pruritic rashes seen in individuals with a family history of atopy. Atopy describes a group of disorders that run together in families, which have historically included asthma, allergic rhinitis, food allergies, and atopic dermatitis. Most recently, a number of experts now also include eosinophillic gastroenteritis as part of the spectrum of atopy. In very young children (younger than 1 year), the characteristic rash of atopic dermatitis is limited to the face and scalp. As children get older, the rash is seen mainly on the flexors, specifically on both the popliteal and antecubital fossae. Atopic dermatitis often is manifested on the feet or hands, or both, of adults, where it is seen as a diffuse, pruritic, scaly, erythematous eruption (Fig. 16-1). Toe web spaces are usually spared, which can help differentiate atopic dermatitis from dyshidrotic eczema and tinea pedis. Combination therapy usually works best for atopic dermatitis of the feet. This includes potent and ultrapotent topical steroid ointments to help treat the dermatitis. An oral antihistamine is often helpful to decrease the associated pruritus. In severe cases, tar derivatives can be compounded with topical steroids to increase the effectiveness of the topical preparation and to allow the use of a milder, and thus safer, topical steroid. It is important to have patients take at least 1 week off per month from the use of strong topical steroids. During this break, the best maintenance treatment is the use of over-the-counter moisturizers that contain ceramides. Ceramides are a family of proteins which help to maintain the skin’s barrier function and are deficient in the skin of patients with atopic dermatitis.4,7 A group of agents known as topical immunomodulators (TIMs) has been approved for the treatment of atopic dermatitis. However, their poor penetration significantly limits their use on the thick skin of the soles and palms. There are several systemic treatments available for severe cases of atopic dermatitis, such as cyclosprine, methotrexate, and azothioprine; however, discussion of their use is beyond the scope of this chapter.18 Dyshidrotic eczema is a common eczematous dermatitis limited to the feet and hands. The earliest clinical lesions are pruritic microvesicles along the side of the toes, fingers, feet, and hands (Fig. 16-2). However, the eruption usually progresses to take on a papulosquamous appearance. Dyshidrotic eczema was previously thought to be a response to excessive or abnormal sweating, thus the term dyshidrosis. Although patients with this condition often do have hyperhidrosis, this is no longer thought to be the cause. Treatment is identical to that of atopic dermatitis in most cases. Psoriasis is a common papulosquamous skin disease affecting 1% to 2% of the population. It most often affects the elbows, knees, scalp, feet, and hands. The primary skin lesion of psoriasis is a well-demarcated, erythematous plaque with an overlying thick, silvery scale (Fig. 16-3). A helpful clue in diagnosing psoriasis is the finding of a pinpoint of blood when one of the overlying scales is removed. This is the Auspitz sign. Psoriasis lesions on the feet can be very hyperkeratotic. Pitting of the nails is seen in 35% of patients with psoriasis and up to 85% of patients with psoriatic arthritis. Treatment for psoriasis begins with potent topical steroid ointments. If these are not effective as monotherapy, tar soaks can be used before application of the topical steroids. Several new topical preparations are also available for the treatment of plaque psoriasis, including vitamin D cream and ointment and several retinoic acid derivatives. For the most severe cases of psoriasis of the feet, treatment with either cytotoxic agents (such as methotrexate and cyclosporine) or any of the antitumor necrosis factor biologic therapies are reasonable options but are beyond the scope of this chapter.8 Allergic contact dermatitis is a specific eruption that requires a previous exposure to an allergenic compound and is mediated by the immune system. Chronic contact dermatitis is seen as a well-demarcated area of scaling and erythema (Fig. 16-4), whereas acute contact dermatitis can also show vesiculation. Both are very pruritic. The most common causes of contact dermatitis on the feet are components used in the production of rubber or the tanning of leather.17 Stasis dermatitis is a common papulosquamous eruption seen in elderly persons, usually those who have lower extremity edema or poor venous return. In either case, RBCs extravasate from the blood vessels of the skin into the connective tissue of the skin itself. Clinically, this is manifested as a swollen leg with overlying, pruritic scaling and erythema (Fig. 16-5). This eruption is usually limited to the anterior tibial surfaces and below, often affecting the ankles and the dorsa of the feet as well. Figure 16-5 Chronic stasis dermatitis. Note the edema, erythema, and scaling of the lower extremity. The most severe and worrisome complication of stasis dermatitis is venous stasis ulceration (Fig. 16-6). These ulcers most often are seen on the medial aspect of the ankles. They usually result from mild trauma to an atrophied area of epidermis with compromised blood supply. The ulcers usually have a well-demarcated edge and thick, adherent yellow exudates at their bases. Most wound healing centers have found that optimum treatment includes daily application of silver sulfadiazine cream to the wound under Ace wraps. If this is not effective, Unna boots can be placed and changed weekly. Secondary infection must be treated with oral antibiotics on an as-needed basis. For severe recalcitrant ulcerations, especially in diabetics, platelet-derived growth factor is now available as a topical preparation, but it is extraordinarily expensive. Lichen planus is a skin disease characterized by numerous polygonal, violaceous, flat-topped papules. These lesions often have very thin overlying white scales known as Wickham striae. The most common areas of involvement are the dorsal aspects of the ankles and wrists (Fig. 16-7). Oral and genital mucous membranes also can be involved. An uncommon variation is hypertrophic lichen planus. This condition manifests with large hyperkeratotic, violaceous plaques over the anterior tibial surfaces. If left untreated, the chronic inflammation associated with this condition can predispose the affected area to a squamous cell carcinoma.12 Lichen planus also exhibits the Koebner phenomenon (see the earlier discussion of psoriasis). Pityriasis rubra pilaris (PRP) is an uncommon skin condition, but it is included here because it often manifests with a characteristic eruption on the soles and palms. In its most extreme form, PRP presents as an exfoliative erythroderma, a condition in which patients are red and scaly from head to toe. The soles and palms of most patients with pityriasis rubra pilaris have a carnauba wax appearance (Fig. 16-8). This refers to the massive palmoplantar hyperkeratosis and its resemblance to the yellow wax once on to treat surfboards. Pityriasis rubra pilaris can be confused with widespread psoriasis. Treatment of this condition is usually with methotrexate or etretinate, which is an oral vitamin A derivative. Keratodermas are a group of conditions associated with a thickening of the cornified layer of the epidermis. Keratodermas can be widespread or localized. Both types almost always involve the skin of the soles and palms (Fig. 16-9). More than 20 types of keratoderma are described in the literature. Discussion of their individual features and treatment options is beyond the scope of this chapter.21 Three types of tinea pedis are seen. Interdigital tinea pedis most often begins with involvement of the fourth interdigital web space. Clinical findings include erythema, scaling, and maceration in the web spaces. Involvement can spread to include the soles and the dorsa of the feet. When involvement of the top and bottom of the feet predominates, the term moccasin tinea pedis has been used to define this second type (Fig. 16-10). The somewhat more unusual third type, bullous tinea pedis, shows numerous small blisters and can be confused with bullous dyshidrotic eczema. The only way to confirm this diagnosis is by potassium hydroxide (KOH) examination.
Dermatology of the Foot and Lower Extremity
 Bulla: Raised, fluid-filled lesion greater than 1 cm in diameter.
Bulla: Raised, fluid-filled lesion greater than 1 cm in diameter.
 Macule: Flat skin lesion seen only as an area of color change on the skin surface and not palpable.
Macule: Flat skin lesion seen only as an area of color change on the skin surface and not palpable.
 Nodule: Raised solid legion with indistinct borders and a component felt deeply below the skin surface.
Nodule: Raised solid legion with indistinct borders and a component felt deeply below the skin surface.
 Papule: Solid raised lesion less than 1 cm diameter.
Papule: Solid raised lesion less than 1 cm diameter.
 Plaque: Solid raised lesion greater than 1 cm in diameter and with distinct borders.
Plaque: Solid raised lesion greater than 1 cm in diameter and with distinct borders.
 Pustule: Papule filled with pus, giving it a yellow-white appearance.
Pustule: Papule filled with pus, giving it a yellow-white appearance.
 Vesicle: Raised, fluid-filled lesion less than 1 cm in diameter.
Vesicle: Raised, fluid-filled lesion less than 1 cm in diameter.
 Atrophy: Thinning of the skin seen as a shiny, wrinkled skin surface.
Atrophy: Thinning of the skin seen as a shiny, wrinkled skin surface.
 Crusting: Dried exudate that sits on the skin surface during and after an acute dermatitis.
Crusting: Dried exudate that sits on the skin surface during and after an acute dermatitis.
 Erosion: Depression into the skin, with the base of the lesion still within the epidermis.
Erosion: Depression into the skin, with the base of the lesion still within the epidermis.
 Excoriations: Linearly oriented crusted lesions secondary to scratching and typically seen in pruritic dermatoses.
Excoriations: Linearly oriented crusted lesions secondary to scratching and typically seen in pruritic dermatoses.
 Lichenification: Thickening of the skin as manifested by accentuation of normal skin tension lines.
Lichenification: Thickening of the skin as manifested by accentuation of normal skin tension lines.
 Scaling: Excess amount of stratum corneum that appears as white plates on the skin surface.
Scaling: Excess amount of stratum corneum that appears as white plates on the skin surface.
 Ulcer: Depression into the skin, with the base of the lesion into the dermis.
Ulcer: Depression into the skin, with the base of the lesion into the dermis.
Papulosquamous Diseases
Primary Skin Conditions
Atopic Dermatitis
Dyshidrotic Eczema
Psoriasis
Contact Dermatitis
Stasis Dermatitis

Lichen Planus
Pityriasis Rubra Pilaris
Keratoderma
Skin Eruptions Caused by Infections
Tinea Pedis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Dermatology of the Foot and Lower Extremity