The Taylor Spatial Frame (TSF) is an external-fixator that corrects deformities in 6 axes, and can successfully manage disorders involving multiplanar deformities. In the developing-world, orthopaedic surgeons are often faced with deformities from neglected trauma and birth defects more severe than those typically seen in developed-countries. This article evaluates the applicability of TSF in the challenging medical environment of Haiti. At Haiti Adventist Hospital, the authors treated 80 cases using the TSF with a minimum follow-up of 1-year. Good results were observed in 99% of the cases (79 out of 80), approaching similar outcomes than those described in literature.
Key points
- •
There is a high prevalence of congenital, posttraumatic, and postinfectious limb deformities in Haiti.
- •
Haiti has a substantial need for external fixation, which can be used to treat complex deformities in a precise and efficient manner.
- •
Gradual correction with the use of distraction osteogenesis creates a new realm of opportunity for the treatment of severe deformities, bone deficits, and length discrepancies that are frequently seen in Haiti.
- •
The Taylor Spatial Frame has been shown to be an appropriate technology for the treatment of many patients in Haiti.
Introduction: nature of the problem
The reasons for the high prevalence of congenital, posttraumatic, and postinfectious limb deformities in resource-limited countries such as Haiti includes the following: lack of environmental regulation (teratogenic pollutants in the air, soil, and water), lack of education, urbanization, transportation-related injuries, natural disaster, lack of prenatal care, and limited access to health care. This high prevalence of limb deformities, many of which are severe, presents some unique challenges in the limited-resource environment and creates the need for improvisation and innovation. Ideally this must not be allowed to compromise results. Indications and surgical techniques may vary based on the type and severity of limb deformities being treated, but surgical principles should remain the same, independent of geographic location.
The basic principle of deformity correction involves normalizing the alignment of the mechanical axis of the affected limb. Essentially, the center of the knee falls on a straight line linking the femoral head to the center of the ankle. Lower extremity deformity correction requires precision to obtain good short-term and long-term results. Preoperative radiographic analysis of the hip or ankle deformity will reveal secondary/compensatory deformities. It is important to also include an analysis of sagittal plane alignment. The location of the apex (or apices), also called the CORA (center of rotation of angulation) must be determined. This location is found by first analyzing joint orientation angles, determining which bone is involved, and then defining the point where the proximal and distal axes intersect. These concepts have been elucidated elsewhere in great detail.
Globalization, communication, and technology have increased our ability to improve orthopedic care around the world. The Taylor Spatial Frame (TSF), with its Internet-based Total Residual Program (TRP), has made deformity correction easier and more accurate than the first-generation Ilizarov ring fixator technology. The widespread availability of the Internet has put the TSF technology within reach in austere environments, provided that reliable follow-up of patients is possible.
Economic challenges are a significant factor in developing nations such as Haiti. More than 90% of the population has no health care insurance, and most patients are only able to pay a small amount, if anything, for surgical operations. The cost of orthopedic hardware is prohibitive in many situations. The use of an expensive device such as the TSF may seem unrealistic in the developing world. Medicolegal considerations in North America have limited the reuse of external fixation components and thus have created a source for high-quality “pre-owned” external fixator equipment for the developing world. These “gently used” TSF parts are donated by volunteer surgical mission groups hospital, and constitute a viable and reliable supply chain.
The implications of reusing external fixators in resource-limited environments are different from those in North America, owing to perceptions and medicolegal issues. Is it safe to reprocess external fixators for multiple use? In most of Europe (where resources are not severely limited) and in developing countries, external fixators are reused on a regular basis, despite their being labeled “single use only.” With an eye toward cost containment and social responsibility, some hospitals in North America have sought pathways to reprocess single-use devices (SUDs). The Food and Drug Administration (FDA) has classified SUDs into 3 categories: noncritical risk (level 1), semicritical risk (level 2), and critical risk (level 3). The reuse of fixator clamps and bars that do not penetrate the skin are considered level 1 SUDs by the FDA. These SUDs have approved device reprocessing protocols, including cleaning to remove all biological material, dismantling the device, inspection of components for defects or fatigue cracks, and resterilization. In Haiti, the authors use similar methods of checking the components for defects, discarding damaged parts, lubricating struts, and cleaning and resterilizing all components in organized instrument trays.
Several clinical studies have been published showing no loosening of components, no loss of fixation, no increase in pin-site infections, and no mechanical failures when reusing fixators. In the rare event of mechanical failure of an external fixator component, it can usually be repaired in the clinic with noninvasive, nonoperative means.
Haiti Adventist Hospital (HAH) treats many complex cases of malunion, acquired deformities, and neglected congenital conditions. Orthopedic surgeons face considerable challenges when treating these deformities in Haiti. Patients often are not able to access health care in a timely fashion, and there may be barriers to follow-up. Many severe and sometimes previously operated deformities present to the national referral center. Often these are sequelae of simple issues that have been poorly treated. Although the Haitian immune system is generally strong, the lack of sterile conditions in surrounding hospitals and the often delayed or neglected treatment of postoperative or posttraumatic infections add significant challenge to the treatment of deformities that involve chronic osteomyelitis. These infections are treated with a very proactive approach to surgical debridement followed by a course of intravenous and/or oral antibiotics. Prolonged empiric protocols of intravenous antibiotic treatment that are common in the United States are often not possible in Haiti. This situation requires clinicians to depend on meticulous surgical debridement followed by limited use of oral antibiotics and close clinical follow-up. The TSF has enabled the authors to address many of these complex deformities, sometimes complicated by osteomyelitis and resultant bone defects and shortening ( Figs. 1–6 ).





Indications and contraindications
Indications
- •
Congenital deformities (eg, club foot, radial club hand, congenital pseudarthrosis of the tibia, fibular hemimelia)
- •
Developmental deformities (eg, rigid equinus, posttraumatic forefoot supination, Blount disease, lower leg deformities related to rickets)
- •
Posttraumatic deformities including malunion of the long bones (eg, cubitus varus, tibial deformity), nonunion, or pseudarthrosis
- •
Complex multiplanar deformities involving need for simultaneous combinations of angular, rotational, and longitudinal (length) correction
- •
Limb-length discrepancy
- •
Bone deficit after osteomyelitis requiring bone transport
- •
Deformities involving poor soft-tissue tolerance to acute correction or open surgery with internal fixation
- •
Acute fractures
Contraindications
- •
Inability to follow the postoperative regimen (noncompliant or mentally incompetent patients)
- •
Social and geographic barriers that preclude adequate follow-up
- •
Lack of Internet access
- •
Surgeon unfamiliarity with the TSF
Surgical technique and procedure
Preoperative Planning
Preoperative planning, understanding the principles of deformity correction, experience, and proper equipment, are essential elements of a well-executed operation.
- 1.
Clinical examination. During the initial examination, perform a thorough inspection of the limb, noting clinical deformities in all planes. Record range of motion for the hip, knee, and ankle, and note any contractures.
- 2.
Radiography. The best way to evaluate lower extremity deformities is with long (36-inch [91.5 cm] for children, and 51-inch [129.5 cm] for adults) standing lower extremity images taken with tube distance of 10 ft (3 m) to minimize magnification. At HAH these long cassettes are not available, so the authors compensate by taking weight-bearing orthogonal images of the area of interest and also including a standing anteroposterior (AP) image of the pelvis with blocks under the short leg as needed. Any hip, knee, and/or ankle contracture, in addition to any varus or valgus deformity, is taken into consideration when leg-length discrepancies are analyzed. The status of growth plates is checked on all images to determine if there is any growth arrest. Intraoperative fluoroscopy can also be used to clarify any preoperative measurements to more accurately program spatial frame corrections. The use of an electrocautery cord with fluoroscopy has been shown to be an accurate way of determining lower limb alignment in individuals who are not excessively obese.
- 3.
Analyze.
- a.
Determine the level(s) and magnitude(s) of the deformity.
- b.
Calculate limb-length discrepancy.
- c.
Plan the level of the osteotomy and the configuration of the frame.
- a.
- 4.
Prepare. Equipment preparation by the surgeon is essential in environments where vendor representatives are not available. The inventory must be checked, components must be clean and in good working condition, and trays sterilized and ready for surgery.
Patient Positioning and Preparation
- 1.
Position the patient supine on a radiolucent table. The whole extremity should be prepared so as to be able to use a sterile tourniquet if necessary.
- 2.
Position the C-arm on the side of the unaffected limb and place the monitor in the direct line of sight of the surgeon.
Surgical Approach: Bone
The basic principle is to apply the fixator to the intact bone first, then perform the osteotomy. Operations that involve gradual distraction using external fixation typically involve osteotomies that are performed percutaneously by 1 of the following methods:
- 1.
Tibia: 1-cm anterior longitudinal incision anteriorly; perform the osteotomy using multiple passes with a 3.8- or 4.8-mm drill bit and an osteotome for completion.
- 2.
Femur: 1-cm lateral longitudinal incision; perform the osteotomy using multiple passes with a 3.8- or 4.8-mm drill bit and an osteotome for completion.
- 3.
Fibula: 3- to 4-cm open approach via the peroneal/soleus interval. Perform the osteotomy using multiple passes with a 1.8-mm wire and an osteotome for completion.
- 4.
Tibia (metaphysis only): In the proximal and distal tibia the osteotomy can be performed with a Gigli saw passed via 2 (proximal) or 3 (distal) small stab incisions. Midfoot osteotomies can also be performed in similar fashion via 3 or 4 incisions, respectively.
Surgical Procedure: Taylor Spatial Frame
There is a wide variety of applications for the TSF. Proximal and diaphyseal tibial deformities are the most common indications and easily demonstrate the basic application principles for this prototype configuration.
- 1.
Choose the reference fragment. This description cites the proximal segment because it is the most common. The reference ring will be mounted perpendicular to the axis of the reference segment, suspended off a wire inserted perpendicular to the proximal axis. In the case of the proximal tibia where the normal medial proximal tibial angle is 87°, this wire is placed parallel to the joint or, more correctly, slightly convergent to the medial tibial plateau going from lateral to medial, and should be parallel to the floor with the tibial tubercle directly anterior. The reference ring is then attached to this transosseus wire, perpendicular to the reference axis on the AP view. One tab of the ring should be directly anteriorly, to function as the “master tab” where struts #1 and #2 come together on the proximal ring. Next a 6-mm anterior half pin is inserted directly anteriorly, suspended from a cube. This action is taken while checking the lateral radiographic view (image intensifier) and swiveling the ring on the tensioned reference wire until the ring is perpendicular to the reference axis on the lateral view. Considering that the normal posterior proximal tibial angle is 81°, this ring should be placed at a 9° angle relative to the joint line (converging posteriorly on the lateral view) to ensure that it is perpendicular to the anatomic axis of the proximal fragment in the sagittal plane. Using a 2/3 ring for the distal femur, proximal tibia, and distal humerus allows maximum joint range of motion (see Fig. 1 C). Mounting the reference ring orthogonal to the reference segment in both planes is the most critical part of the procedure. The knee should be ranged to make sure that it is not impinging on soft tissues. Once the ring is mounted, take an AP and lateral image-intensifier view gunsighting down the ring with a magnification marker, and with bolts marking the equator of the ring on AP and lateral projections. From these shots, the mounting parameters may be calculated (how far anterior/posterior and medial/lateral the center of the ring is relative to the reference axis).
- 2.
Place the second (“moving”) ring on the diaphysis. This ring need not be perpendicular to the axis of the moving segment, but it is more aesthetic to have it nearly orthogonal. Place an anterior-to-posterior 6-mm half pin at a comfortable distance from the proximal ring to fit medium-sized struts in between the 2 rings. An upright 4- or 5-hole cube is usually used near the mid anterior (antimaster tab) portion of the distal ring. The half pin is placed perpendicular to the tibial shaft looking from the lateral view and approximately in line with the second toe (see Figs. 1 C, 2D , and 3A ). Swivel this ring until it is approximately perpendicular to the distal mechanical axis segment. Secure this ring alignment by adding an anteromedial 4- or 5-hole cube suspended downward with a 6-mm half pin placed from medial to lateral.
- 3.
Connect the 2 rings with 6 telescopic struts numbered from 1 to 6, adjusting them as necessary to match the ring positions (see Fig. 2 D). Struts 1 and 2 must come off the master tab on the proximal ring, and numbers are always applied counterclockwise when looking from the top down. After the TSF struts are applied, ask the circulating nurse to record the strut sizes, lengths, and ring sizes for later programming.
- 4.
After the struts are attached additional points of fixation can be added, according to the available corridors between the struts. In general, use at least 3 points of fixation per segment for femur or tibial frames (2 per ring in upper extremity frames). Basic concepts of external fixator stability should be followed by placing the pins in widely separated positions in the axial plane (delta fixation), and also spaced as far apart as possible proximally and distally (see Fig. 6 C).
- 5.
Osteotomy: Detach the struts from the proximal ring. Make a small anterior longitudinal incision subperiosteally at the desired location, and perform an osteotomy via this small entry using a several passes with a 3.8- to 4.8-mm drill bit and 8- to 10-mm osteotome, or use the Gigli technique as described previously. In most cases, especially those that involve lengthening, a fibular osteotomy is also necessary, achieved via a small incision well distal to the peroneal nerve at the junction of the middle and distal thirds of the fibula. If lengthening is intended, proximal and distal syndesmotic fixation is added to prevent dislocation or subluxation of the ankle mortise or the proximal tibiofibular joint. The fibular osteotomy and prophylactic anterior compartment fasciotomy are best done initially, under tourniquet control, before application of the rings.
- 6.
Reattach the struts to the proximal ring at their original orthotopic lengths.
- 7.
Postoperative radiographs: AP and lateral plain radiographic orthogonal views are taken, with a magnification marker, gunsighting down the reference ring, including as much of the affected bone as possible. Mounting parameters may be measured from these films, or from previously positioned image-intensifier views made during surgery.
- 8.
TRP: Measure and enter the deformity parameters, the mounting parameters, and the frame parameters into the software program. The velocity of correction must then be determined, and may be based on a surgeon-selected Structure At Risk (SAR). The SAR is typically the concave cortex at the level of the osteotomy. In certain cases of valgus-to-varus correction, the SAR may be the peroneal nerve. The amount of distraction that should occur daily (usually 1 mm/d) is then entered. The Web-based TRP then will create a prescription for deformity correction, and store the program for future access and modifications.
- 9.
Seven to 10 days after surgery, the patient begins turning the struts on the frame. The patient refers to the computer-generated schedule to make the appropriate turns to the correct struts. It is important to teach the patient and family the correct way to adjust the struts, in addition to pin-care protocols.
The 6 deformity parameters are:
- •
AP view angulation (valgus or varus)
- •
Lateral view angulation (procurvatum or recurvatum)
- •
Axial view angulation (internal or external rotation)
- •
AP view translation (medial or lateral)
- •
Lateral view translation (anterior or posterior)
- •
Axial view translation (short or long)
The 3 frame parameters are:
- •
Diameter of proximal ring
- •
Diameter of distal ring
- •
Length of the various struts
The 4 mounting parameters are (reference ring relative to the origin):
- •
AP view frame offset
- •
Lateral view frame offset
- •
Axial view frame offset
- •
Rotary frame offset (for describing a master tab or antimaster tab that is not directly anterior)
Complications and management
- •
Nerve complications: Neuropraxia is usually avoided by respecting the anatomy during the surgery and also appropriately programming the SAR. Gradual corrections usually allow for the nerves to accommodate to the new length. Pain on the top of the foot is the first sign of gradual stretch injury of the peroneal nerve. Early judicious peroneal nerve decompression can reverse the damage.
- •
Growth plate injury: Use the image intensifier when inserting wires and half pins near joints.
- •
Malalignment: Axis deviation or incomplete correction of deformity can be treated if recognized before bone consolidation. The TRP allows easy recalculation of variables to produce a new schedule for the patient. Additional programs may be created as needed.
- •
Joint contractures: Physical therapy and stretching exercises are mandatory to prevent contractures. Knee-flexion contractures are common with proximal tibia applications, especially when lengthening is occurring. Equinus contractures also can occur, and can be prevented by placing a dorsiflexion orthosis and strap beneath the foot connected to the frame or including the foot in the construct. Gastrocsoleus recession is sometimes necessary if contractures do occur.
- •
Delayed union and nonunion: Monitor the bone formation every 2 weeks. If deficient, slow the rate of distraction, or even reverse it for a time. All patients should be on multivitamins and vitamin D 3 . Smoking and nonsteroidal anti-inflammatories should be forbidden. Rarely, bone grafting is needed.
- •
Pin-tract infections: Treat with oral antibiotics and local pin care. Deep involvement is heralded by osteolysis around the pins, requiring removal, debridement, and possible replacement with a new pin. Rarely, toxic shock and necrotizing fasciitis have been reported.
Postoperative care
- •
After frame application, the patient remains in the hospital for 3 or 4 days for pain management and frame management training (adjustments and pin care).
- •
The physical therapist starts mobilization on the day after surgery. It is crucial to maintain joint range of motion to prevent stiffness and contracture.
- •
Follow-up clinic visits with radiographs should take place every 2 weeks during the correction phase with additional visits for strut changes as necessary. During the consolidation phase, radiographs and clinical examinations are performed once every month.
- •
After deformity correction has been achieved, the TSF remains in place for an additional period of time (consolidation phase) to allow for complete consolidation of the regenerate bone (healing of 3 of 4 cortices). Frame removal is done in the operating room as an outpatient.
Outcomes
- •
From August 2011 to October 2012, approximately 900 orthopedic cases underwent surgical treatment at HAH. On average, 5 TSF surgeries are performed every month; however, during some busy weeks, more than 7 TSF procedures are performed each week.
- •
The TSF was used in 80 (9%) of these 900 cases.
- •
Sixty-nine patients (42 females, 27 males) underwent 80 procedures with the TSF.
- •
Of the 80 procedures, 79 (99%) achieved good healing and deformity correction. All of these patients are able to walk without limping or pain.
- •
One patient of the 80 (1%) developed an osteomyelitis of his tibia, which necessitated removal of the TSF to cure the infection.
The results achieved in Haiti with the use of TSF for complex limb reconstruction are comparable with reported results in the international literature.
Case examples
- 1.
A 14-year-old boy presented for bilateral tibia vara (see Fig. 1 ). He reported that he felt very uncomfortable walking in the streets going to school. His friends were laughing at him all the time. He and his mother requested correction of the bone deformity. Both legs were addressed at the same time.
- 2.
A 17-year-old boy presented to HAH for a neglected distal tibia malunion (see Fig. 2 ). He reported that he had an accident when he was 3 years old and that he had never obtained any care for this injury. He had an extreme valgus deformity of the distal tibia with external rotation. Treatment consisted of a supramalleolar osteotomy using the TSF to obtain gradual correction and lengthening.
- 3.
A 22-year-old man with a family history of hypophosphatemic rickets. He developed very severe genu valgum with both tibias and femurs involved (see Fig. 3 ). He was unable to walk and had to crawl on his knees and hands. The TSF was used on both tibias, and Orthofix LRS external fixators on the femurs. The 4 bones were corrected. The patient can now walk straight without any aids and is pain free.
- 4.
A 14-year-old girl with hyopophosphatemic rickets and severe genu valgum and malrotation of the legs (see Fig. 4 ). She was only able to crawl. Isolated, she could not attend school. One leg was treated (femur and tibia) and once this was healed, the second leg was similarly treated. LRS was used for the femurs and double-level TSF for the tibias. She can now stand and walk straight without pain.
- 5.
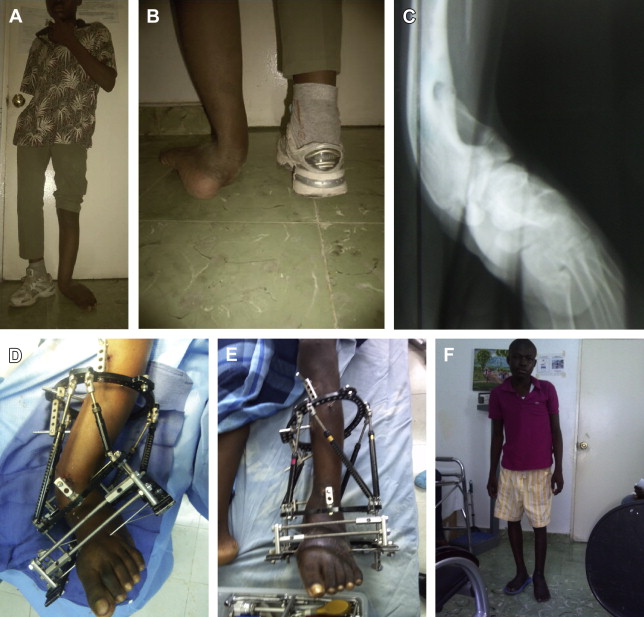
A 14-year-old girl with bilateral neglected clubfoot. Two options were considered: either shorten the foot via triple arthrodesis or apply a TSF. The TSF approach was chosen (see Fig. 5 ) to correct the congenital equino cavo varus deformity. She can now wear shoes and walk platigrade.
- 6.
A 27-year-old man with neglected bilateral tibia vara (see Fig. 6 ). He had to quit school because of this deformity. He was referred to HAH where he was treated for both Blount deformities with the TSF.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






