Decompression, Posterolateral, and Interbody Fusion for High-Grade Spondylolisthesis
Nanjundappa S. Harshavardhana
Dino Colo
John P. Dormans
DEFINITION
Spondylolisthesis is derived from the Greek words (spondylo = spine and olisthesis = to slip). It is the forward displacement of a vertebra relative to its neighboring vertebra (ie, adjacent caudal vertebral segment).
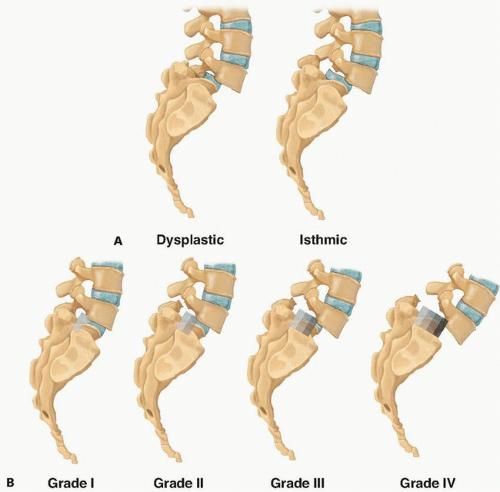
In children and adolescents, spondylolisthesis most commonly occurs due to a pars defect (ie, nonunion of the pars interarticularis). Wiltse called this an isthmic type of spondylolisthesis. It may also occur in the presence of inherent spinal anomalies such as deficient or maloriented lumbar and lumbosacral facets (ie, dysplastic or congenital type).2,11,12,16,27,29
It has been grouped into five different types under the Wiltse-Newman classification28:
Type I: dysplastic
Type II: isthmic
Type III: degenerative
Type IV: traumatic
Type V: pathologic
Pars interarticularis is “the place between two joints”.17 Most spondylolisthesis cases are of dysplastic (congenital), isthmic, and degenerative types. Degenerative listhesis is common in adults and most commonly seen at L4-L5 level. The dysplastic and isthmic types most commonly affect L5-S1 level and are usually seen in children (FIG 1A).
The Meyerding classification is used to quantify the severity of slippage (FIG 1B) and has five grades19:
Grade I: 0% to 25% slip
Grade II: 26% to 50% slip
Grade III: 51% to 75% slip
Grade IV: 76% to 100%
Grade V: corresponds to spondyloptosis
Marchetti and Bartolozzi divided spondylolisthesis into low- and high-grade slips irrespective of underlying etiology.17 Anterior slippage of 50% or more (Meyerding grade III and above) of the transverse width of the caudal segment is termed a high-grade slip.
ANATOMY
The vertebral bodies increase in size and dimensions with progression caudally from the cervical spine. This increase is believed to be related to the demands of increased stress and weight bearing placed on the lumbosacral spine.
The lumbar vertebrae have a wider transverse diameter in comparison to the anteroposterior (AP) diameter. The lumbar foramina appear trefoil-like. The spinous processes have a larger surface area and have an oblong appearance. Transverse processes are long, slender, project laterally, and are more oriented in the sagittal plane allowing for flexion and extension motion.24,30
The neurovascular structures in the lumbar spine run a similar course as in the thoracic spine. The segmental vasculature arises directly from the aorta and runs dorsally around the lateral aspect of each vertebral body. Branching occurs near the pedicles, wherein one branch supplies the spinal canal and the other supplies the paraspinal musculature. These vessels run between the transverse processes and are susceptible to bleeding in lateral dissection while performing a posterolateral fusion.
The spinal cord usually ends at the upper border of L1 or L1-L2 disc. The conus medullaris extends from the most distal portion and innervates the bowel and bladder. Beneath the conus, the lumbar and sacral nerve roots are arranged to form the cauda equina. Each of these roots exits below the pedicle of the corresponding vertebrae from the neural foramen and form the lumbar/lumbosacral plexus that innervates the lower extremities.6
The pedicles are cylindrical structures with a cortical shell that bridge the posterior elements of the spine with the vertebral body.
The height and diameter as well as the transverse diameter of the pedicles increases from the thoracic to the lumbar spine. T5 has the narrowest and L5 has the widest transverse diameter.
They are directed medially in the transverse plane, increasing gradually from L1 to L5.
The sagittal plane orientation of the lumbar spine pedicles is neutral at L2 and L3.
The spinal cord and the dural sac lie within the vertebral canal protected by vertebral body ventrally, pedicles laterally, and posterior elements dorsally. The exiting nerve roots are in proximity with the inferior aspect of the pedicle.24
The orientation of the facet joints in the lumbar and lumbosacral spine is related to function. In the upper part of the lumbar spine, the orientation of the joints allows for multidirectional stabilization. This is in contrast to the lumbosacral facet joint, which is flat and more coronally oriented and acts to resist shearing forces through the joint.10
PATHOGENESIS
Spondylolisthesis is a disorder related to upright posture and seen in bipedal mammals due to increasing forces acting on the lower segments of the spine. It is never seen in quadrupeds and nonambulatory individuals.
The lumbar spine is subject to high shear forces and compressive loads. The “bony hook,” consisting of the pedicle, pars interarticularis, intervertebral disc, and the facet joints, provides stability by resisting these shear forces by preventing forward slippage.
Gravity, paraspinal, and anterior abdominal muscle contraction on the lordotic lumbar spine and pelvis apply forces to the lower lumbar vertebra with a caudal-ventral vector. If left unchecked, these forces would cause the lower lumbar vertebrae to slip and rotate forward relative to the sacrum.
Congenital anomalies of the posterior elements in spina bifida (ie, dysplastic spondylolisthesis) can significantly compromise their normal buttressing function and stability offered by the facet joints. The spine has a tendency to slip even if the posterior elements are intact. This is brought about by the structural abnormality in the facet joint’s inability to resist the load and shear forces.
In the isthmic type of spondylolisthesis, secondary to a pars defect, there is loss of posterior restraint. The high shear and compressive forces occurring through the lumbar spine and lumbosacral joint are less well resisted.11,12,13
Observing the spectrum of spondylolisthesis developing owing to such dysplastic elements prompted Marchetti and Bartolozzi to further subdivide this category into low and high-grade dysplasias.17 Of the high-grade spondylolisthesis, they identified mainly two subtypes: (1) with elongation and (2) with lysis.
In low-grade spondylolisthesis, the L5 vertebral body maintains its rectangular shape. The superior endplate of the sacrum is flat and lumbar lordosis remains within the normal range. However, high-grade spondylolisthesis has a trapezoidal L5 body and rounding of the superior sacral endplate (dome-shaped sacrum). The sacrum tends to be vertical with loss of lumbar lordosis (flat back). This distinction between high and low dysplasia also has prognostic value, as high-grade dysplasias lead to progressive deformity and predisposition for lumbosacral kyphosis with worsening of symptoms over time.17
Some of the changes seen in high-grade slips are secondary to forward displacement of vertebrae. They are mainly seen as Modic endplate changes in discs with degeneration. High-grade slips may already occur by adolescence and the severity of deformity makes it highly unlikely that these teenagers remain asymptomatic or progress into adulthood without progressive worsening of symptoms.
NATURAL HISTORY
Harris and Weinstein13 reviewed 38 cases with high-grade spondylolisthesis treated nonoperatively and with in situ fusion with a mean follow-up of 24 years and showed that 36% of patients treated nonoperatively were asymptomatic, 55% had back pain, and 45% had neurologic symptoms.
Beutler et al2 in a 45-year follow-up study of 30 patients diagnosed with spondylolysis, screened in the 1950s from
a pool of 500 first-grade children, showed that no patients with unilateral pars defects developed spondylolisthesis. They also showed that cases with bilateral pars defects and low-grade slips follow a course similar to that seen in the general population. Slowing of slip progression was observed with each decade.2
In a comparison of patients with dysplastic and isthmic spondylolisthesis, it was found that dysplastic spondylolisthesis progressed more rapidly and to a greater Meyerding grade than isthmic spondylolisthesis.18
PATIENT HISTORY AND PHYSICAL FINDINGS
In symptomatic patients, the most common clinical manifestation is low back pain, with or without radicular pain radiating through the L5 or S1 dermatome. Onset of pain is usually chronic and insidious, but acute episodes do occur. Pure radiculopathy in the absence of back pain is uncommon. Adolescents and teenagers most often complain of back pain with little or no leg pain.16
In patients with radicular symptoms, unilateral involvement is more common.
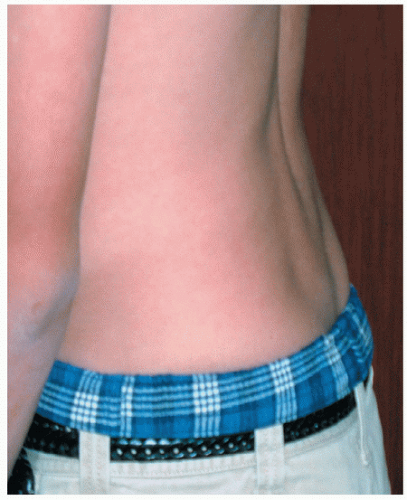
Flattening of the lumbar lordosis is commonly seen on physical examination (FIG 2).
A palpable step in the spinous processes is often seen in isthmic spondylolisthesis.
Abnormal gait exemplified by a flexion at hips and knees gait pattern and tight hamstrings may be present (Phalen-Dickson gait).
Hamstring tightness is recorded by measuring the popliteal angle. Many patients with high-grade slips will have a tendency to develop tight hamstrings owing to the development of abnormal biomechanics in the lumbar spine.
Straight-leg raise should be done to test for nerve root compression or hamstring tightness. A positive examination with radicular pain denotes either an L5 or S1 nerve root compression. Radicular pain elicited between 30 and 70 degrees is indicative of nerve root compression, whereas that elicited above 70 degrees might denote extraspinal compression of the sciatic nerve. Pain in the posterior thigh denotes hamstring tightness.
Examination should also include the Lasegue test. Exacerbation of the pain is suggestive of nerve root tension (most commonly L5). Femoral nerve stretch test might be positive in degenerative listhesis (L4 being most commonly affected).
A digital rectal examination should be done in suspected cases of bladder and bowel dysfunction as a part of preoperative neurologic assessment.
IMAGING AND OTHER DIAGNOSTIC STUDIES
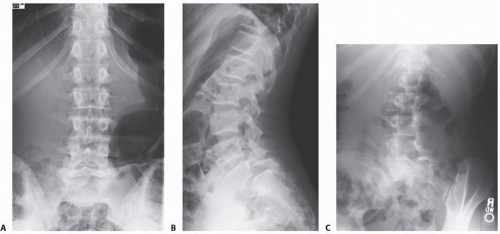
Initial imaging includes standing posteroanterior and lateral radiographs of the spine (FIG 3A,B). Oblique views (FIG 3C)
may provide additional information in certain cases, but their use for diagnosing spondylolysis without listhesis in adolescents is controversial.1
Plain radiographs are used to establish the overall alignment of the spine in both the coronal and sagittal plane. The sagittal alignment should be noted, particularly the degree of lumbar lordosis above the lumbosacral kyphosis. Any structural abnormalities in the spine in addition to the slip should be noted. These abnormalities include the presence of spina bifida occulta, scoliosis, or sagittal plane abnormalities. Other spinal problems should be treated as per individual merits.
Coned down view of lumbosacral junction and Ferguson view (20-degree cranially angulated AP x-ray centered over lumbosacral junction) may also be performed to rule out coexistent far out syndrome.
Computed tomography (CT) scans with three dimensional (3-D) reconstruction are valuable in defining the exact bony abnormality and will help in preoperative planning (FIG 3D,E).
Magnetic resonance imaging (MRI) studies are indicated when there is evidence of neurologic compromise. MRI provides good visualization of nerve roots, spinal stenosis, and cauda equina compression (FIG 3F).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree