Costotransversectomy for Canal Decompression and Anterior Column Reconstruction via a Posterior Approach
Yu-Po Lee
Charles C. Chang
Ankur D. Patel
Steven R. Garfin
DEFINITION
The costotransversectomy uses a posterolateral approach to the thoracic spine. This approach provides access to the posterior spine, the lateral spinal canal, and also to the anterolateral portion of the vertebral body.
In comparison to the formal anterior thoracotomy, the costotransversectomy approach allows extrapleural access to the thoracic spine. Because the pleural cavity is not violated, this reduces the risk of pulmonary complications.4,13 Additionally, although anterior thoracotomy provides limited access in the regions of the thoracic inlet and the levels near the diaphragm, the costotransversectomy approach can expose any level of the entire thoracic spine.
Limitations of the costotransversectomy approach center on its poor visualization of the anterior canal. This makes addressing midline pathology such as broad-based calcified discs or central herniation more difficult via the costotransversectomy approach. Furthermore, a transthoracic approach may be advantageous in situations of multilevel involvement in order to avoid operative blood loss and thoracic cage instability from rib resection.
ANATOMY
The thoracic vertebrae are chiefly distinguished from the adjacent cervical and lumbar spinal regions by the presence of complex osteoligamentous articulations with the ribs.7,8,10
Two major articulations account for the costovertebral joint.
Ventrally, each thoracic rib articulates with the adjacent vertebral body and rostral intervertebral disc by the anterior costovertebral ligament, also known as the radiate ligament. Dorsolaterally, the costotransverse ligaments support the costal articulation with the transverse process.
The superior costotransverse ligament extends from the inferior edge of the transverse process to the superior margin of the caudally adjacent vertebrae.
The medial costotransverse ligament, also known as the capsular ligament, attaches the posterior neck of the rib with the anterior margin of the transverse process.
Finally, the lateral costotransverse ligament attaches the transverse process to the posterior costal tubercle.
The osseous variability along the length of the spine adds to the complex three-dimensional anatomy of the region, making thoracic spine surgery a technical process requiring a thorough understanding and proper preoperative planning.
There are 12 thoracic vertebrae, each with slight variations in measurable dimensions. Specifically, variations exist between vertebral body diameter, facet positioning, pedicle dimensions, and transverse process and spinous process dimensions.7,8,10
Pedicle widths gradually decrease from T1 to T4 and increase from T4 to T12. Pedicle width is approximately 4.5 mm at T4, whereas pedicle width at T12 is approximately 7.8 mm. Pedicle height and length tend to increase from T1 to T12. Medial orientation and transverse pedicle angle tend to decrease from T1 to T12.7,8,10
PATIENT HISTORY AND PHYSICAL FINDINGS
A thorough history and physical examination is the basis of complete preoperative planning. The history should include medical and surgical history, social history addressing functional disability and socioeconomic issues, and history of pain or neurologic symptoms.
The physical examination should consist of observation of deformity and gait, palpation for tenderness or masses, range of motion of the spine and joints, assessment of intact neurologic function with a sensory/motor examination, and rectal examination.
IMAGING AND OTHER DIAGNOSTIC STUDIES
As previously mentioned, safe preoperative planning relies on understanding the complex three-dimensional anatomy of the costovertebral articulations, vertebrae dimensions, and locations of the neurovascular bundles.
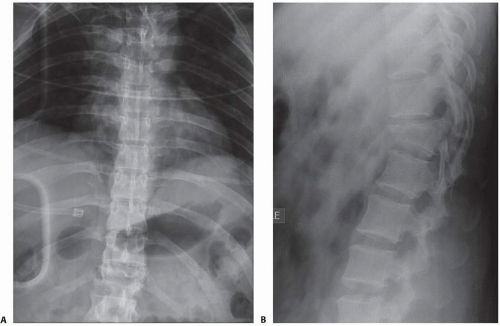
Proper imaging, including radiographs (FIG 1) and/or advanced imaging modalities, is essential to preoperative planning.
Magnetic resonance imaging (MRI) is the imaging modality of choice for most pathologies to characterize the soft tissue of the involved region, especially cases involving spinal cord compression.
Computed tomography (CT) myelography may offer comparable visualization of the neural elements and is especially beneficial in cases where spinal instrumentation has been used previously.
For bony anatomy, CT is the preferred modality. Sagittal reconstruction and three-dimensional CT imaging may be useful supplements to axial sequences.
Frequently, both MRI and CT imaging are obtained for preoperative planning to characterize both the regional soft tissue and bony anatomy, respectively.
NONOPERATIVE MANAGEMENT
The decision to treat a patient operatively or nonoperatively depends on the underlying disease.
With some tumors, radiation may be the first line of treatment.
With most thoracic disc herniations and other degenerative diseases, nonoperative treatment is often tried prior to consideration for surgery unless there is neurologic deterioration.
SURGICAL MANAGEMENT
Anterolateral spinal decompression of infection/abscess
Vertebral body biopsy or partial resection (neoplastic, traumatic)
Anterior intraspinal tumor
Removal of paracentral herniated disc
Congenital kyphosis or kyphoscoliosis
Sympathectomy
Various fusions, including limited anterior spinal fusion
Rib pain
Preoperative Planning
A thorough history and physical examination is essential. In cases in which a tumor or infection is suspected, the history may provide clues as to the origin of the tumor or infection.
Appropriate laboratory values should be obtained. These include a basic metabolic panel, complete blood count, prothrombin time, and partial thromboplastin time. In cases in which tumors or infections are suspected, an erythrocyte sedimentation rate and C-reactive protein are also recommended. In cases in which infections are suspected, blood cultures may be helpful in identifying an organism.
Arranging for appropriate blood products is recommended. In the case of tumors and infections, there can be considerable blood loss, and hemostasis may be difficult to achieve. In addition to packed red blood cells, fresh frozen plasma and platelets may also need to be called for ahead of time.
Appropriate imaging—including radiographs, MRI, and CT—is essential.
If time permits, a biopsy is recommended in the cases where tumors are suspected and a primary is not known. Embolization of tumors that have a propensity to bleed (renal cell carcinoma, hemangioma, hemangiosarcoma) is recommended.
Discussion with the anesthesiologist regarding maintaining mean arterial pressure above 70 mm Hg to ensure adequate perfusion to the spinal cord
Positioning
Various positioning techniques are available depending on the surgeon’s preference. It is the authors’ preference to use a prone position on the operating table. Longitudinal chest rolls with the arms tucked in on a radiolucent table is our preferred method to maintain stability during the corpectomy and allow access for fluoroscopy (FIG 2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree