Correction of Posttraumatic Extensor Tendon Ulnar Subluxation of the Metacarpophalangeal Joint with a Dynamic Lumbrical Tendon Transfer
Keith A. Segalman
Beatrice L. Grasu
E. F. Shaw Wilgis
INDICATIONS/CONTRAINDICATIONS
Posttraumatic failure of the sagittal bands (SBs) at the level of the metacarpophalangeal (MCP) joint results in extensor tendon instability. When the extensor tendon is no longer centered over the MCP joint, there is a resultant loss of extension of the finger. Legoust first described traumatic extensor tendon instability in 1866. Paget, Krukenberg, and Marsh provided later descriptions of the condition. The technique described here has not been previously published.
PHYSICAL EXAMINATION
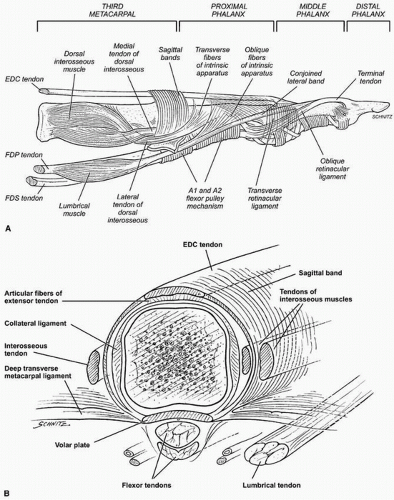
The SB is the main stabilizer of the extensor digitorum tendon at the level of the metacarpal phalangeal joint. The SB forms a cylindrical tube surrounding the metacarpal head and the MCP joint (Fig. 13-1). The sagittal fibers are superficial to the MCP joint capsule, and there
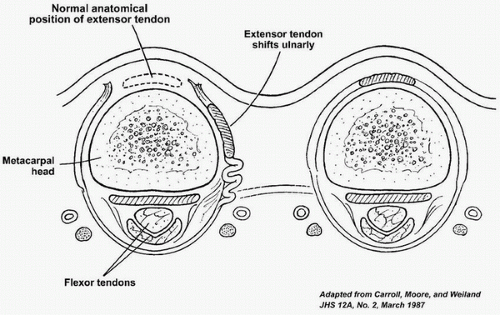
is no communication between the sagittal fibers and the collateral ligaments. The radial SB is thinner and longer than are the ulnar fibers. The SB is thicker in the central digits and thinner in the peripheral digits. The greatest tension in the SB is noted with MCP flexion and radioulnar deviation, with a vast majority of the injuries occurring on the radial side. Biomechanical studies have shown that greater than 50% of the proximal radial fibers must be torn to create extensor tendon instability (Fig. 13-2).
is no communication between the sagittal fibers and the collateral ligaments. The radial SB is thinner and longer than are the ulnar fibers. The SB is thicker in the central digits and thinner in the peripheral digits. The greatest tension in the SB is noted with MCP flexion and radioulnar deviation, with a vast majority of the injuries occurring on the radial side. Biomechanical studies have shown that greater than 50% of the proximal radial fibers must be torn to create extensor tendon instability (Fig. 13-2).
The usual mechanism of injury is a blow to the hand with the MCPs flexed, such as a boxing injury. SB injuries occur when the finger is forced into flexion with the wrist flexed and ulnarly deviated. Rarely,
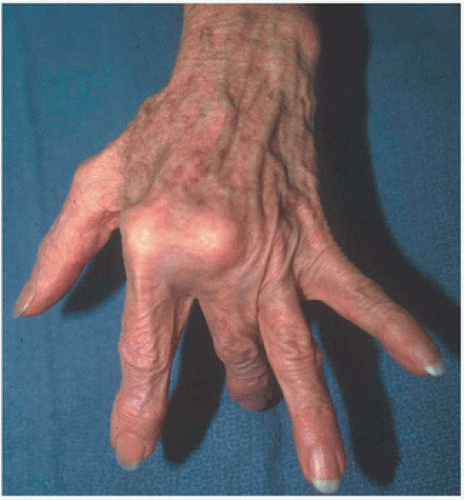
an SB injury may be associated with collateral ligament injuries. The patient will usually present with swelling and tenderness over the SB and limited or deviated extension of the MCP joint. The most telltale finding is a painful snapping sensation with concomitant ulnar subluxation of the extensor tendon during active MCP flexion (Fig. 13-3). Rayan and Murray described a provocative test for SB injury: resisted finger extension and attempted deviation toward the injured SB elicit apprehension and pain.
an SB injury may be associated with collateral ligament injuries. The patient will usually present with swelling and tenderness over the SB and limited or deviated extension of the MCP joint. The most telltale finding is a painful snapping sensation with concomitant ulnar subluxation of the extensor tendon during active MCP flexion (Fig. 13-3). Rayan and Murray described a provocative test for SB injury: resisted finger extension and attempted deviation toward the injured SB elicit apprehension and pain.
Two classification systems have been described, but in our opinion, neither fully characterizes the clinical situation. Ishizuki differentiates ruptures of the SB secondary to superficial tears and deep tears. Rayan and Murray have described a more treatment-oriented classification system of three
varieties emphasizing whether the SB is torn or there is subluxation of the tendon. What is most important is the assessment of the passive motion in the joint and the stability of the contralateral ligaments.
varieties emphasizing whether the SB is torn or there is subluxation of the tendon. What is most important is the assessment of the passive motion in the joint and the stability of the contralateral ligaments.
For acute injuries, immobilization with a cast or Orthoplast splint with the MCP joints in extension and the wrist in neutral is often satisfactory. Rayan and Murray have reported that conservative treatment is most successful when begun within 3 weeks of the injury, whereas Inoue recommended repair or reconstruction when the patient is seen more than 2 weeks after the injury. Occasionally, conservative treatment of acute injuries is unsuccessful, but most patients with SB injuries will present with a chronic condition.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree