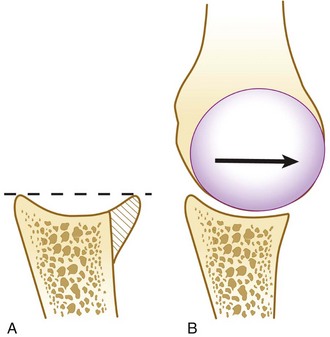
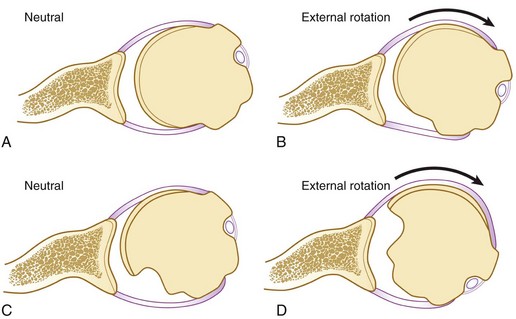
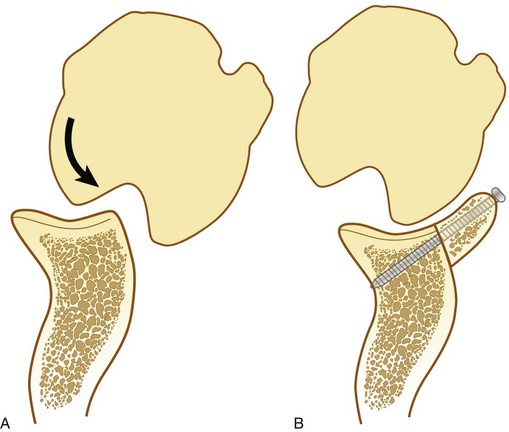
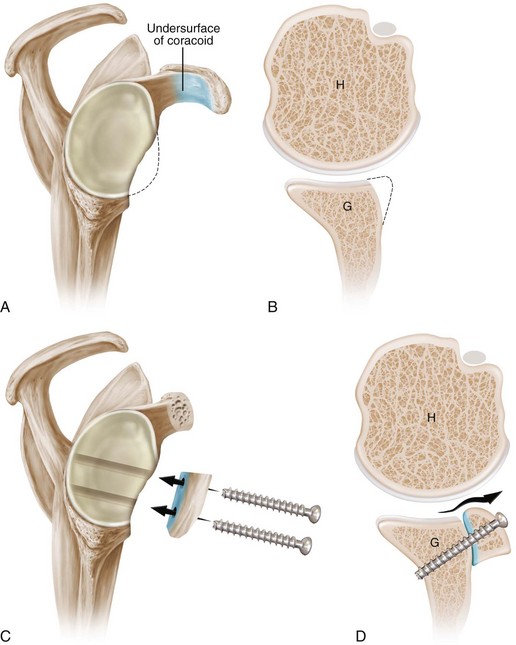
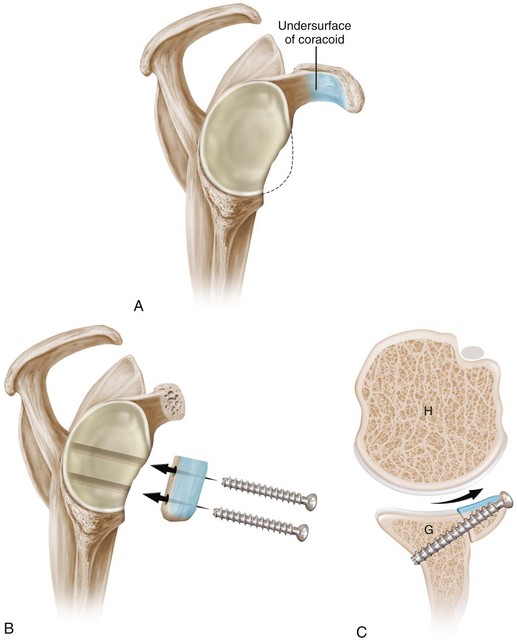
Chapter 18 Recognizing and properly addressing bone defects is crucial to achieving good surgical outcomes in shoulder instability. One of the most important requirements for glenohumeral stability is a long congruent articular arc in which the humerus and glenoid remain in contact throughout motion. Loss of this congruent arc can occur from glenoid bone loss or defects in the posterior humeral head (i.e., Hill-Sachs lesions) (Figs. 18-1 and 18-2). Such lesions are present in up to 95% of patients with recurrent shoulder instability.1 Examining the glenoid alone, Sugaya and colleagues reported that 90% of patients with recurrent instability have glenoid bone abnormalities (including bone loss or abnormal contour).2 Glenoid bone loss (distinct from abnormal contour alone) was seen in 50% of cases; in over half, the defect was greater than 5% of the glenoid width. In the setting of glenoid bone loss of greater than 25% of the inferior glenoid diameter, recurrence after arthroscopic Bankart repair is 67% to 75%.1,3 In such cases, recurrence can be dramatically reduced by the Latarjet procedure, in which the coracoid is transferred to the glenoid (Fig. 18-3). As noted by Patte, the success of the Latarjet procedure can be attributed to the triple effect, which is composed of the following: 1. Lengthening of the articular arc by the bone graft 2. The sling effect of the conjoined tendon 3. Tensioning of the lower subscapularis by means of the conjoined tendon in its new position (draped over the lower subscapularis) Our evaluation for bone loss is based on preoperative and intraoperative assessments. We routinely obtain anterior-posterior, trans-scapular lateral, and axillary radiographs of the glenohumeral joint. Radiographs from all patients are evaluated for the presence of glenoid bone loss or a Hill-Sachs lesion. Whereas plain radiographs can grossly demonstrate bone defects, the severity is often underestimated. We therefore obtain a computed tomography (CT) scan with three-dimensional (3D) reconstructions on all individuals with suspected bone loss. In addition, we have a low threshold for performing CT in patients without plain radiographic evidence of bone loss who otherwise have risk factors for recurrence (e.g., young patients, multiple dislocations). For estimation of glenoid bone loss, bilateral 3D CT scans are obtained. Assuming a normal contralateral shoulder, the percentage of bone loss is easily estimated by comparing the width of the glenoid on the affected side with the width of the glenoid on the normal shoulder in the en face view. In 96% of cases this technique accurately stratifies glenoid bone loss as less than or greater than 25% of glenoid width.4 Our main indications for performing an open Latarjet procedure are the following: 1. Glenoid bone loss of greater than 25% of the inferior glenoid diameter (“inverted pear” glenoid) or 2. Deep Hill-Sachs lesion that engages in a position of 90 degrees of abduction plus 90 degrees of external rotation (position of athletic function) One relative indication for the Latarjet reconstruction is in the patient with severe soft tissue loss involving the anterior labroligamentous complex. Such soft tissue deficiency can occur because of thermal capsular necrosis or because of multiple failed soft tissue procedures for instability. Although some authors have recommended soft tissue allografts, we have preferentially done the Latarjet reconstruction without soft tissue augmentation. Alternatively, we have noted that there are occasional cases with partial loss of the capsule (thermal capsular necrosis; multiple failed surgeries) without any significant bone loss. We have found that such cases may be amenable to arthroscopic repair with a flap of the deep surface of the subscapularis to augment or to substitute for the anterior capsule.5 The major contraindications to the Latarjet procedure are infection and voluntary instability. In 1954 Latarjet described his technique for a coracoid bone graft to prevent anterior dislocation.6 He detached the pectoralis minor from the coracoid, incised the coracoacromial ligament, left a stump of the coracoacromial ligament attached to the coracoid, then completed the osteotomy at the base of the coracoid so that it could be placed as a bone graft against the anterior glenoid neck. The coracoid was passed through a split in the subscapularis and positioned so that its inferior surface was in contact with the anterior glenoid neck, where it was secured with two screws (Fig. 18-4). In doing this, the posterolateral surface of the coracoid was placed adjacent to the glenoid joint surface. We call our surgical technique the congruent-arc technique. This technique was first reported by Burkhart and de Beer7 in 2000 and incorporated two important modifications: 1. The coracoid graft was rotated 90 degrees around its long axis so that the concave inferior surface of the coracoid became the extension to the glenoid concavity, providing a much more anatomic articular arc for the reconstructed glenoid surface8 (Fig. 18-5). Figure 18-5 Schematic of the Burkhart–de Beer modification of the Latarjet reconstruction. A, Sagittal view demonstrates glenoid bone loss. The undersurface of the coracoid is shaded in blue. B, After coracoid osteotomy the graft is rotated 90 degrees so the undersurface of the coracoid is flush with the glenoid and forms a continuation of the concave glenoid articular arc. The graft is secured with two screws. C, Axial view demonstrates how the orientation change (compared with the original French technique [see Fig. 18-4]) provides a contour that more closely matches the native glenoid concavity and also provides greater length extension of the articular arc. G, Glenoid; H, humerus. (From Burkhart SS, Lo IK, Brady PC, Denard PJ. The Cowboy’s Companion: A Trail Guide for the Arthroscopic Shoulder Surgeon. Philadelphia: Lippincott Williams & Wilkins; 2012.)
Coracoid Transfer
The Modified Latarjet Procedure for the Treatment of Recurrent Anterior Inferior Glenohumeral Instability in Patients with Bone Deficiency
Preoperative Considerations
Imaging
Indications and Contraindications
Surgical Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Coracoid Transfer: The Modified Latarjet Procedure for the Treatment of Recurrent Anterior Inferior Glenohumeral Instability in Patients with Bone Deficiency