Convertible Total Elbow Replacements
Graham J.W. King
Shawn O’Driscoll
Ken Yamaguchi
INTRODUCTION
A convertible total elbow replacement provides the surgeon the option to switch from an unlinked to a linked articulation or vice versa without having to revise either the ulnar or humeral prosthetic stems (1,2). A large proportion of patients who suffer from arthritis can be adequately treated with an unlinked elbow arthroplasty. Some patients with arthritis and many with other indications require a linked device owing to a lack of adequate bone stock or deficiency of the collateral ligaments. A convertible total elbow replacement permits the surgeon to make a decision to link the prosthesis should an unlinked implant not be stable or not be articulating congruously intraoperatively. Furthermore, it is possible to later link an unstable unlinked arthroplasty through a minimally invasive procedure without having to remove and revise well-fixed components.
INDICATIONS/CONTRAINDICATIONS
The indications for a convertible total elbow arthroplasty are similar to those for all elbow arthroplasty designs. The most common indications are rheumatoid arthritis or other types of inflammatory arthritis, primary or posttraumatic osteoarthritis, osteonecrosis, hemophilic arthropathy, comminuted distal humeral fractures, and periarticular tumors. Active infection is an absolute contraindication such as for any other joint arthroplasty. A history of remote infection, an inadequate soft tissue envelope, a nonfunctional hand, and the unwillingness of a patient to be compliant with postoperative long-term restrictions are considered relative contraindications.
PREOPERATIVE PLANNING
The collateral ligament function and extent of bone loss should be evaluated with a careful physical examination and radiographs to assist in deciding between a linked and an unlinked arthroplasty. Templates are available to evaluate the size and shape of the elbow relative to the implants.
DESIGN OVERVIEW
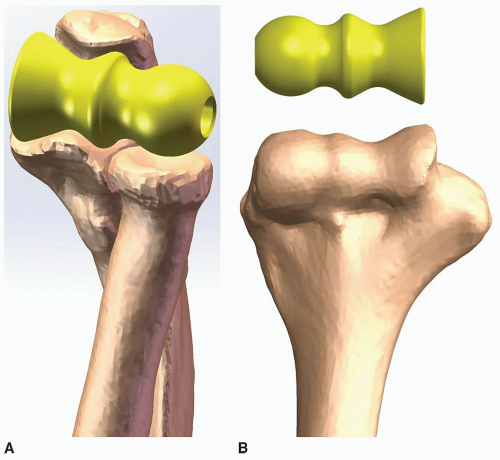
The Latitude EV total elbow arthroplasty (Tornier, Inc.) provides a wide variety of implant sizes and options for primary and revision total elbow arthroplasty (Fig. 35-1). In addition to short, long, and extra-long stem humeral and ulnar components, an optional bipolar radial head arthroplasty is available. The capitellar portion of the humeral component is anatomic, also allowing retention of the native radial head. An anatomic distal humeral hemiarthroplasty option is available in many countries worldwide, but not currently in the United States. The humeral component is modular; the stem and articulation are coupled using a cannulated bolt that incorporates a locking ring to prevent loosening. The cannulated bolt allows sutures to be placed through the implant to facilitate repair of
the collateral ligaments. The cobalt-chrome stems are treated with titanium plasma spray, and the humeral stem incorporates an anterior flange to help prevent implant loosening. An optional linkage cap converts the implant to a linked device when indicated. The saddle shape and thick polyethylene of the ulnohumeral articulation optimizes contact throughout motion in an effort to reduce bushing wear. Several features of the implant allow for a significant proportion of unlinked arthroplasties. These include mechanisms to either retain or replace the radial-capitellar articulation, a built-up coronoid process, and anatomic flexion axis restoration. A comprehensive instrumentation system is available to facilitate efficient and accurate implant positioning.
the collateral ligaments. The cobalt-chrome stems are treated with titanium plasma spray, and the humeral stem incorporates an anterior flange to help prevent implant loosening. An optional linkage cap converts the implant to a linked device when indicated. The saddle shape and thick polyethylene of the ulnohumeral articulation optimizes contact throughout motion in an effort to reduce bushing wear. Several features of the implant allow for a significant proportion of unlinked arthroplasties. These include mechanisms to either retain or replace the radial-capitellar articulation, a built-up coronoid process, and anatomic flexion axis restoration. A comprehensive instrumentation system is available to facilitate efficient and accurate implant positioning.
SURGICAL TECHNIQUE: LATITUDE EV SYSTEM
Position
A general or regional anesthetic can be employed. The patient is typically placed in a supine position with the arm across the chest; however, the lateral decubitus position can be used if preferred. Prophylactic antibiotics are administered, and a sterile tourniquet is employed.
Incision
A longitudinal incision is made just medial to the tip of the olecranon, and full-thickness flaps are elevated on the level of the deep fascia as required. The ulnar nerve is identified, mobilized, and anteriorly transposed into a subcutaneous pouch. The medial intermuscular septum is excised.
Exposure
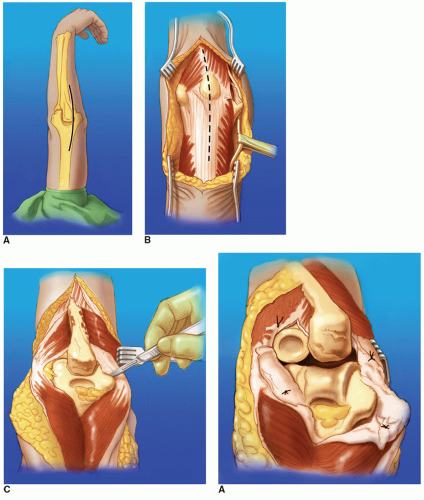
Multiple deep surgical approaches can be employed at the surgeon’s discretion. The triceps can be elevated from the olecranon from medial to lateral (Bryan-Morrey) or from lateral or medial (extended Kocher) (3). Alternatively, a triceps-splitting approach can be employed, elevating the triceps medially and laterally (4) (Fig. 35-2). It is critical with these techniques to maintain continuity of the triceps with a forearm fascia.
Note: When detaching the triceps off the olecranon, care should be taken to ensure a full-thickness tendon for reattachment. A triceps tongue approach can also be used. In the setting of periarticular bone loss from erosive arthritis, previous surgery, or comminuted distal humeral fractures, the triceps can be left attached to the olecranon, lowering the risk of triceps insufficiency in the postoperative period (5,6). The “triceps on” approach compromises visualization of the ulna relative to alternative triceps detaching approaches. The lateral and medial collateral ligaments are sectioned from the humeral epicondyles and tagged for later repair. The posterior capsule and fat pad are excised. Hyperflexion of the elbow allows the olecranon to move away from the humerus, allowing adequate exposure for performing the arthroplasty. Elevation of the anterior capsule off the distal humerus facilitates exposure and placement of the bone graft behind the anterior flange of the humeral component.
Implant Selection
Sizing of the implant is a crucial step. The width of the articulation defines the size of the prosthesis to employ to ensure the capitellum aligns with the radial head. The sizes of the ulnar, humeral, and radial components are not interchangeable. Four different prosthesis sizes are available for the total elbow arthroplasty and six for the anatomic distal humeral hemiarthroplasty.
Note: It is often easiest to size the prosthesis by placing the humeral spool in the greater sigmoid notch of the ulna and evaluating the alignment of the radial head with the capitellar portion of the sizing spool. Alternatively, the spool can be aligned with the distal humerus (Fig. 35-3).
When in between sizes, a smaller implant should be selected unless the radial head is being retained. Sizing in this case is dependent on alignment to the native radial head and may involve selection of the larger implant.
Humeral Preparation
A rough cut is made removing the intracondylar portion between the medial and lateral trochlear ridges with a transverse cut made at the proximal portion of the olecranon fossa. A high-speed burr is used to open the medullary canal of the humerus, widening this for lateral placement of broaches as well as cement restrictors (Fig. 35-4).
The humeral canal is prepared beginning with the starter broach and moving up to the size broach of the stem chosen. An alignment pin placed through the broach is used to control the rotation, while an alignment line on the broach is used to control the depth of insertion relative to the
flexion-extension axis, which runs from the anterior-inferior aspect of the medial epicondyle to the center of the radius curvature of the capitellum. Since the broaches allow for a cement mantle, it is possible to use a humeral broach one size smaller than the implant size in the setting where the fit in the humerus is too tight. Flexible reamers are available to facilitate preparation if the medullary canal is small or if long stem implants are to be employed.
flexion-extension axis, which runs from the anterior-inferior aspect of the medial epicondyle to the center of the radius curvature of the capitellum. Since the broaches allow for a cement mantle, it is possible to use a humeral broach one size smaller than the implant size in the setting where the fit in the humerus is too tight. Flexible reamers are available to facilitate preparation if the medullary canal is small or if long stem implants are to be employed.
The trochlea and capitellum cutting guide is attached to the broach and secured in place using stabilizing pins (Fig. 35-5




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree