Fig. 54.1
Limited constrained condylar knee prosthesis, LCCK (Zimmer®, Warsawa, IL USA)

Fig. 54.2
Posterior stabilized high flex total knee prosthesis (Zimmer®, Warzawa, IL USA)
CCK TKR design guides knee motion in the frontal, sagittal, and axial plane, which is achieved by a large central peg of the liner engaging with the femoral box.
The major drawback of a CCK is that the increase in constraint results in increased forces, directly transferred to the component-cement-bone interface. For that reason stems are highly recommended in order to increase fixation stability. However, this has to be discussed in the context of whether CCK TKR is required in primary or revision surgery.
Severe varus deformity in primary TKR may require an extended capsular and ligamentous release on the medial side to achieve adequate ligament balancing. This may be difficult in cases with additional lateral laxity. Extended soft tissue release will increase flexion and/or extension gap and a thicker liner may be needed. A significant joint line elevation and a secondary patella baja will likely result.
Joint line elevation occurs frequently during revision surgery. One of the reasons may be the attempt to compensate significant distal bone loss or inadequate sizes of distal spacer on the femoral side with the use of a thicker PE liner [12].
Joint line elevation of 5 mm may result in midflexion instability [13, 18]. Porteus et al. showed that a joint line elevation of 5 mm leads to inferior clinical outcome according to the Bristol score [24]. Others have reported significant inferior clinical outcome with joint line elevation more than 8 mm [23]. However, small changes in joint line position, such as 2 mm, do not appear to affect clinical outcome [3].
Joint line elevation also leads to increased patellofemoral contact pressure due to lowering of the patella in relation to the femoral condyles. It remains questionable whether joint line elevation or the secondary patella baja is most decisive for clinical outcome. Patella position has a direct impact on clinical outcome after TKR [8, 20]. Anterior knee pain, extensor lag, and locking due to notch impingement at the femoral component are the major concerns.
Ligament balancing in knees with severe valgus deformity remains a challenge in primary TKR. Soft tissues and the lateral collateral ligament are generally tight. In contrast, the medial collateral ligament is rather loose. Hence, valgus deformity in both primary and revision surgery may require a more constrained TKR (Fig. 54.3). Especially in revision surgery, the treatment may be more complex (Figs. 54.4 and 54.5). Post-traumatic valgus osteoarthritis, which often occurs after fracture of the lateral tibial plateau, results in an overly tight lateral and loose medial collateral ligament. Here, correct implant placement and good range of motion can be achieved with the use of more constrained TKR (Fig. 54.6).


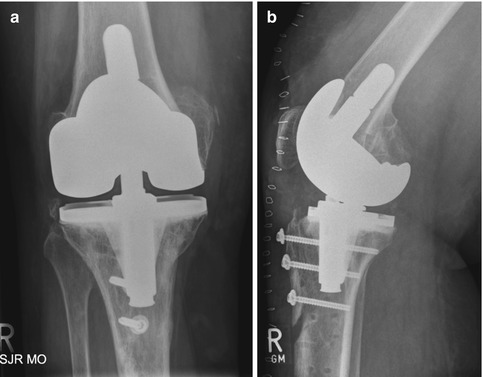
Fig. 54.3
Surgical view. The total stabilized LCCK in place. The tibial tuberosity was osteotomized in order to receive sufficient access to the joint

Fig. 54.4
The tibial tuberosity was fixed with three cortical screws and slightly elevated to address the patella baja

Fig. 54.5
Radiographs after TKR. The femoral and tibial component was implanted using a hybrid fixation technique
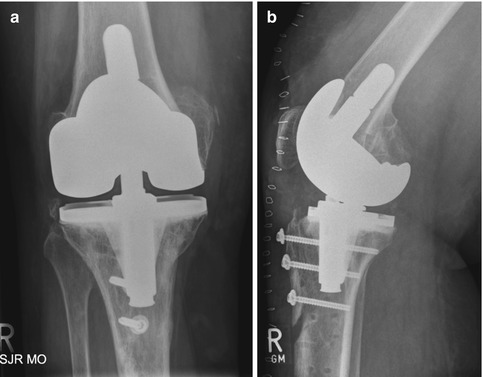
Fig. 54.6
(a, b) AP and lateral views of the CCK TKR without tibial stem and only 30 mm stem on the femoral side
It has been shown that varus malalignment of up to 10° is not associated with significant ligament imbalance [4]. Once the deformity exceeds 10°, significant shortening and tightness of the medial collateral ligament can be expected. Laxity on the convex side in valgus knees is an independent factor for using constrained condylar TKR, as shown in a multivariate analysis [10]. Mediolateral stress X-rays prior to surgery will help indentify the more difficult knee (Fig. 54.2). The alternative to CCK TKR may be the proximalization of the medial femoral epicondyle, including the insertion site of the medial collateral ligament, using a sliding osteotomy of the medial epicondyle. This will tighten the medial collateral ligament [5]. The sliding osteotomy might be an option, especially for younger patients, to avoid the usage of higher constraint implants. Sliding osteotomy of the lateral femoral epicondyle by distalizing the insertion site of the lateral collateral ligament may be an alternative. The technique is often performed using a lateral parapatellar approach to preserve the soft tissue on the medial side [27]. Navigation serves as a helpful tool and offers exact correction of the femoral insertion site of the lateral or medial collateral ligament in both extension and flexion. However, no data are available yet showing superior outcome and survival rates after sliding osteotomy of the epicondyle in conjunction with unconstrained TKR compared to a more constrained prosthesis.
An iatrogenic injury of the medial collateral ligament during TKR is very rare. In such cases, it is recommended to change to a more constrained design rather than suturing the damaged ligament [16].
It can be speculated that higher constrained CCK TKR results in more abnormal knee kinematics, which may have an impact on clinical outcome, but gait analysis and electromyography do not seem to differ between patients after constrained TKR and bilateral UKR [9]. However, both groups did show significant difference in comparison to healthy subjects.
Comparison of knee function after CCK and posterior stabilized TKR has shown a 15° decreased range of motion for the CCK group, but there was no significant difference in clinical outcome in terms of the Knee Society’s outcome score [28]. Limited range of motion is known to have direct impact on function and patient satisfaction [19, 22].
Another major concern in more constrained prostheses is the increased risk of aseptic loosening. Good clinical outcome and low revision rate have been reported in primary TKR with CCK. No mechanical failure or infection was reported in 54 cases after a 10-year follow-up [15]. Another study showed no failure in primary CCK TKR, but a few mechanical failures in revision cases after a mean follow-up of 5 years [14]. Furthermore, there was no difference in range of motion, aseptic loosening, or revision rate between posterior stabilized, CCK, or hinged prosthesis after a mean follow-up of 5 years [11]. A 10-year survival rate of 96 % after CCK TKR has been reported with good or excellent results in 86 % [15].
There is an ongoing discussion about the need of stems in CCK TKR. Due to the increased strain between the implant-cement-bone interface, metaphyseal support is recommended. The indication for stems depends on the bone stock at the proximal tibia and distal femur. The critical question is, how much of the bone support is preserved?
Generally, unstable knees with sufficient bone stock do not require stems. Good results have been reported without increased aseptic loosening when no stems were used, such as reported after primary TKR [1]. Other studies compared the outcome after TKR with or without intramedullary stems. No difference in aseptic loosening was found [21] (Fig. 54.6a, b).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








