Fig. 7.1
AP intraoperative image of sacroiliac joint showing two “confusing” joint lines
There is a basic fact about the orientation of the joint that has been relatively constant and if well understood can help the surgeon. When viewing the dorsal aspect of the patient, the general overall orientation of the joint is approximately a 20–30° angulation from posteromedial to anterolateral. If, however, the joint is analyzed in sections, again from the dorsal aspect, there exists an angular difference between them. The cephalad portion basically maintains the 20–30° oblique angle from posteromedial to anterolateral, whereas the caudal portion is almost in a line perpendicular to the floor and may even angle slightly anteromedial (Fig. 7.2).
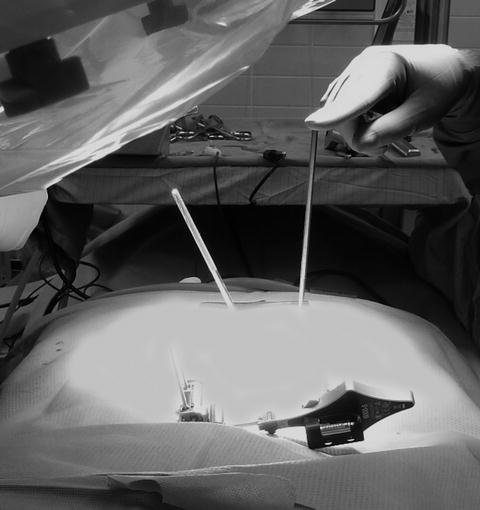
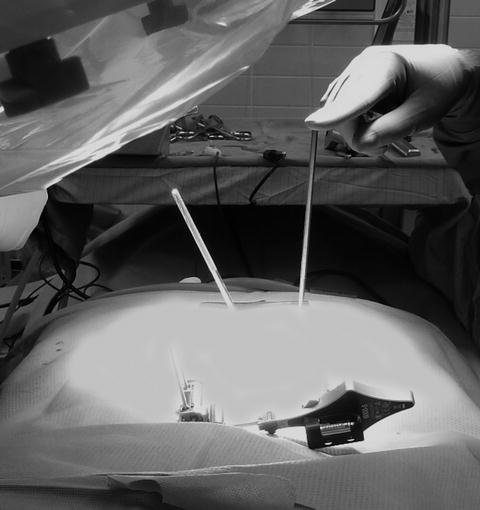
Fig. 7.2
Intraoperative photo showing two K-wires. The vertical wire is in the longitudinal axis of the caudal portion of the sacroiliac joint and the angled wire is in the cephalad portion of the joint
This is why those injecting into the joint do so at the caudal end where, when visualized posterior to anterior in the coronal plane under fluoroscopy with some slight oblique medial or lateral angulation, this joint becomes one joint line allowing for accurate joint injection (Fig. 7.3).
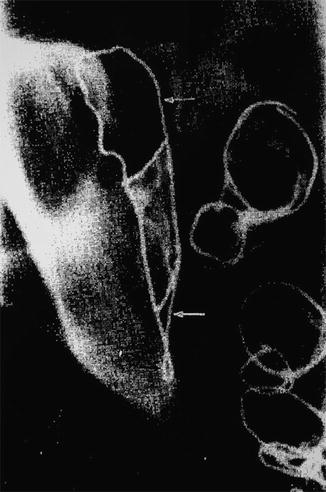
Fig. 7.3
Image showing the outline of the sacroiliac joint (arrows) from posterior demonstrating its “propeller-like” configuration
This knowledge is useful when using image to place a cage from posterior into the longitudinal axis of the joint in its caudal portion. It is in this section of the joint that the ilium is closest to the sacrum and has less posterior ligament mass. It is in this caudal section that the best fusions can occur when approached posteriorly. Interestingly, the subchondral bone of the true SIJ is also where some of the thickest and strongest cortical bone exists for screw or cage fixation. Instrumentation placed in this section has a better chance of firmly connecting the ilium to the sacrum.
Considerations When Imaging in the Anterior–Posterior Plane
Imaging the patient in the lateral plane is very straightforward, has been discussed in the literature for decades, and will be covered in detail in the Chap. 8 discussions on the minimally invasive lateral approach. What is less familiar for the surgeon is understanding the anatomical details in the patient being imaged using the anterior–posterior (AP) plane in the various angles ranging from 30° cephalad (outlet view) to 30° caudad (inlet view). In relation to the SIJ orientation in the prone position, each of these angles views the joint in very different ways. When using AP image to perform posterior lateral screw or cage insertion, these various angles must be clearly understood for successful instrumentation. Starting with the straight AP image view (Figs. 7.4 and 7.5), note the location of the S1 pedicle, the S1 foramen, and the posterior superior iliac spine (PSIS), as these are the landmarks that will be most obvious as they change position when angling the image in this plane. The value of the straight AP image is to assure that the spine and pelvis are symmetrically oriented in the coronal plane with the spinous processes in the centerline and the sacrum and iliac wings appearing equal bilaterally. This view also shows the most prominent portion of the PSIS the best in an area just lateral and cephalad to the S1 pedicle and foramen.
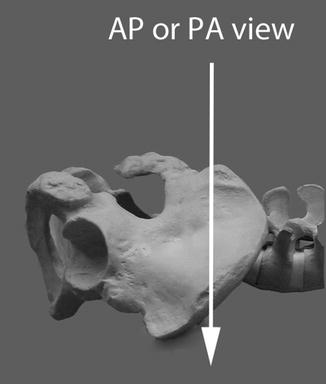
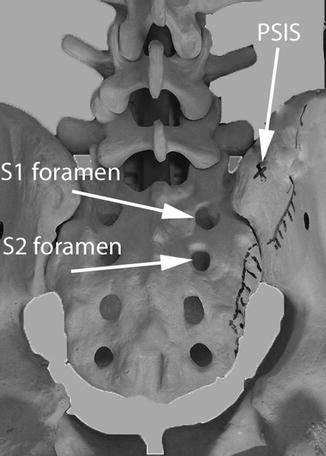
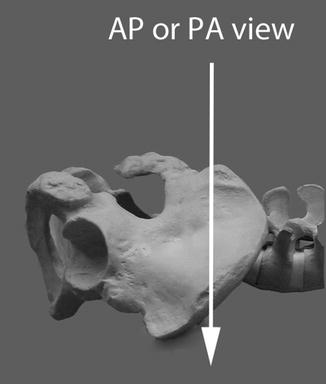
Fig. 7.4
Shows AP or PA plane for imaging for pelvis
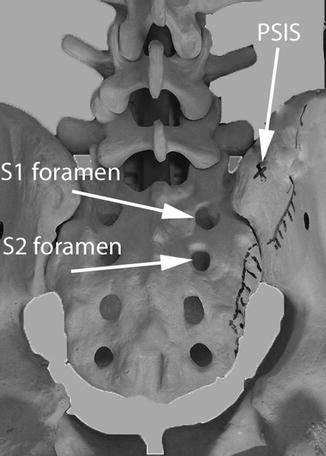
Fig. 7.5
Shows skeletal anatomy with AP image. Note that the PSIS is cephalad to the S1 foramen and possibly at the level of the L5–S1 disk space
When the AP view is moved to the 30° cephalad position, what is being imaged is the “outlet” view (Figs. 7.6 and 7.7). Note again the location of the S1 pedicle, the S1 foramen, and the PSIS. These change in location dramatically with this angular change in the image. This image is very valuable when instrumenting as it gives the best view of the S1 pedicle and the S1 and S2 foramina.
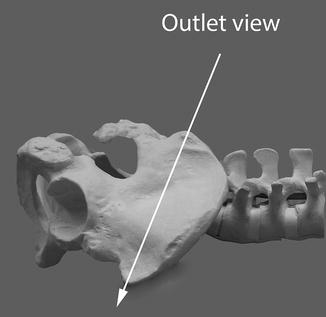
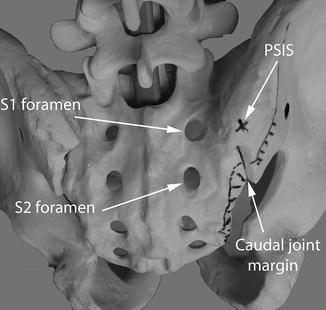
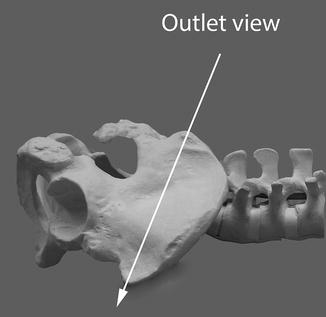
Fig. 7.6
Shows 30° (approximate) cephalad plane of AP imaging for pelvis, the “outlet” view
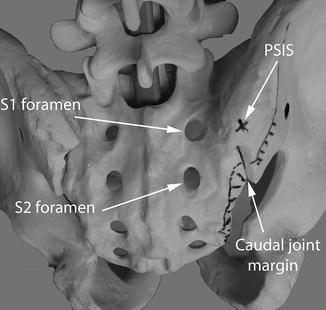
Fig. 7.7
Demonstrates the “outlet” pelvic view which shows the PSIS as being directly lateral to the S1 foramen and the lowest part of the joint margin directly lateral to the S2 foramen (this can vary according to individual)
The third AP angle we will consider is the 30° caudal, or “inlet” view. This represents a 60° angular change in viewing of the AP anatomy compared to the 30° cephalad view. The primary value of this view is to visualize the anterior arch of the sacrum, which consists of the anterior elements of the sacral alae and both the S1 and S2 exiting foramina. Just caudal to the S2 foramen, the sacrum usually angles in a caudal direction and severs its joint connection with the ilium. This caudal portion of the sacrum acts more like an apophasis serving no weight-bearing structural function but is an attachment for multiple ligaments and muscles forming the pelvic sling. This 30° caudal inlet angular view of the sacrum is the primary one used for assuring that no instrumentation goes anterior to the sacrum into the pelvis. It should always be checked as one of the final images after any of the instrumented approaches (Figs. 7.8 and 7.9).
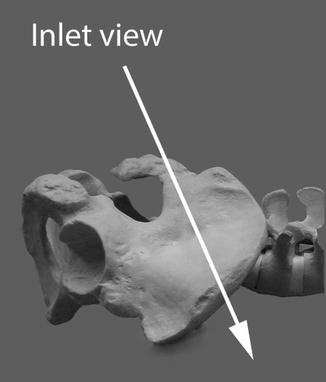
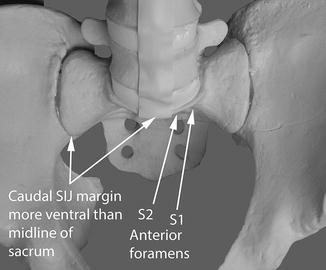
Fig. 7.8
Shows 30° (approximate) caudal plane of AP imaging for pelvis, “inlet” view
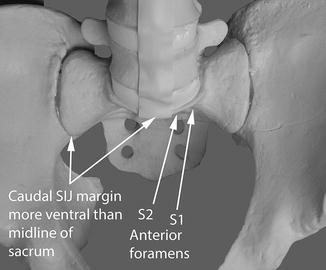
Fig. 7.9
Demonstrates the “inlet” pelvic view, which shows the anterior margin of the sacrum. This view helps to avoid anterior penetration of the sacrum into the pelvis when placing instrumentation
When imaging using the various angles in the AP plane, the surgeon must be fully knowledgeable of the anatomical landmarks present and how they change in relation to one another as the angle of the image changes. From anyone of these three AP angles, there is also the ability to angle obliquely either medial or lateral to further define a location. There frequently is a “learning curve” to understanding what is actually being seen and what the surgeon is expecting to see during these surgeries. If at any time the surgeon becomes confused by the image, it is imperative to return to a known image angle or to move the image “live,” for the shortest period of time possible, until the anatomy in the image is fully understood. If there is still confusion, the question of aborting the current plan comes into play.
Location and Importance of the Cluneal Nerves, Sciatic Nerve, and Superior Gluteal Artery
The subject of cluneal nerves has been discussed in Chap. 3 on anatomy, but a few facts concerning these nerves deserve further dialogue. The cluneal nerves enter the posterior gluteal space approximately 8–12 cm cephalad and lateral to the PSIS along the rim of the ilium to fan out over the buttock (see Figs. 3.10 and 3.14). These nerves access the superficial deep fascial layer, which extends from the midline of the spine laterally over the gluteal musculature. When these sensory nerves are cut, they form neuromas on their transected ends, which can become a source of chronic pain for various different reasons. Hutchinson published how to reflect the cluneal nerves safely out of harms way when using the posterior midline fascial splitting approach to harvest iliac bone graft [1]. He presented dramatic results in significantly decreasing or eliminating the chronic pain occurring from cluneal nerve injury with this method. The potential for injury to the cluneal nerves should be on the surgeon’s mind as he/she considers where to make the incision for exposure to the SIJ. The literature illustrates several techniques where the incision is along the entire arch of the ilium or long straight incisions placed posterolaterally that certainly cross into cluneal nerve territory. Three incision types do, in general, avoid the cluneal nerves. The first type is the posterior midline incision and fascial splitting approach discussed by Hutchinson. The second type are those incisions used for posterior lateral minimally invasive approaches, which essentially are located at, lateral, or inferior to the PSIS and extending for 2 in. or less. The third type is the lateral minimally invasive approach (Fig. 7.10).


Fig. 7.10
Various posterior and lateral incisions to approach the sacroiliac joint with arrows pointing to those which are less likely to injure the cluneal nerves
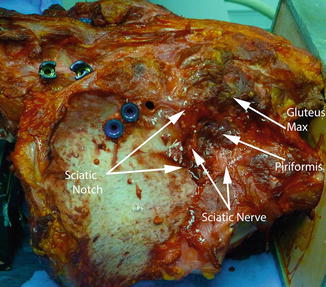
The superior gluteal artery is a branch off of the internal iliac artery that quickly exits the pelvis through the sciatic notch (see Figs. 3.12 and 3.14). It angles cephalad, anterior, and lateral as it branches out between the gluteal muscle layers to provide blood supply to those muscles. Injury to this artery has been implicated as a potentially disastrous complication in the harvesting of the iliac bone graft [2]. Considering that its path literally crosses over the ilium where the SIJ can be superimposed, it is at potential risk with any direct lateral instrumentation effort. If transected, it can retract back inside the pelvis, and if a significant hematoma should occur, be advised that this may need extreme measures to treat. It is possible that interventional radiology might be needed to clot off the bleeder or that an open procedure might be required. At this point, one should also be reminded that the distance from the sciatic notch (see Figs. 3.6 and 7.11), where both the superior gluteal artery and the sciatic nerve exit, is only a few centimeters from the insertion point of the most posterior caudal fixation device using the minimally invasive straight lateral approach. Great caution is advised probing this area while using image in attempting to secure the point of placement for the subsequent drilling and insertion of instrumentation as pushing the probe into the sciatic notch is very possible and can result in neurologic or vascular trauma.