Fig. 5.1
Osteoarthritis of the sacroiliac joint demonstrating spurring, sclerosis, joint widening, and vacuum sign
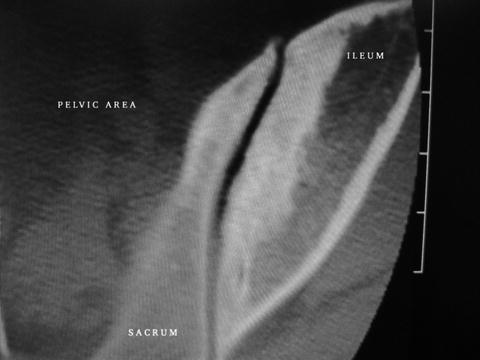
Fig. 5.2
Advanced osteoarthritis of the sacroiliac joint involving entire joint with resultant increase in bone density on both the iliac and sacral sides
Inflammatory Arthritis
This type of arthritis in the SIJ may arise from both a seropositive and seronegative inflammatory disease process. The conditions that have resulted in a successful fusion at our institution were rheumatoid arthritis (RA), the non-joint fusing form of HLA-B27-positive ankylosing spondylitis in a young female, Reiter’s syndrome, and idiopathic sacroiliitis. These inflammatory types of arthritis in the SIJ can cause severe pain, both in the acute and chronic phases, and the delay in diagnosis can be excessive. The affected SIJs can be stable or demonstrating a microtype of instability secondary to the ligament–bone attachments being affected by the inflammatory process (enthesopathy). It is important to be in consultation with a rheumatologist when working with these patients (Fig. 5.3).
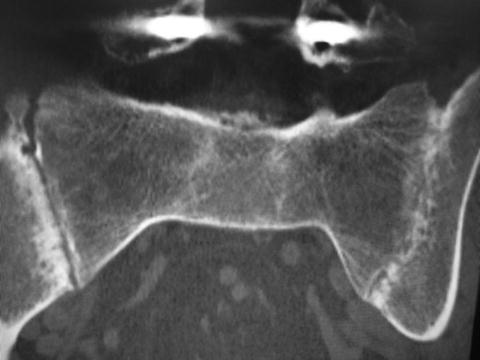
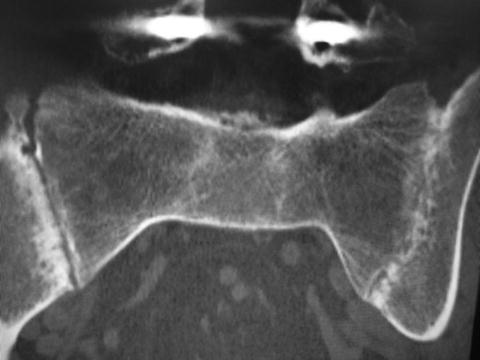
Fig. 5.3
Bilateral inflammatory joint changes showing, as you look at the image, a fusion on the right (asymptomatic) and an incomplete fusion on the left (symptomatic). Note the narrowing, sclerosis, and subchondral bone erosions on the unfused side. Also note the screws from the lumbosacral fusion that failed to resolve this patient’s low back pain
Case Example of RA Affecting the SIJ
The first patient to have a SIJ fusion at BBSI presented to us in 1991. She was 74 years old and unable to stand or put weight on her right leg secondary to severe pain and the feeling of instability. Her bone scan was significantly enhanced over the right SIJ, and her CT showed typical signs of joint erosions, surrounding osteoporosis, and an obvious separation of the joint margins. She had been suffering with this condition for several years, had seen countless doctors, and was confined to a wheel chair. Due to the current surgical standard being simply placing two screws across the joint into her osteoporotic sacrum, and her suggesting death as her next option, we devised a posterior midline approach to fuse and instrument her SIJ. This procedure allowed for better screw to bone fixation. There was no readily available instrumentation for this at that time so a bone plate (used for long bones) crossing the joint posteriorly fixated with large cancellous screws in the S1 pedicle and the ilium along with autogenous iliac bone graft were used. Due to the fixation being quite rigid, she was allowed to weight bear as tolerated in the first postoperative week and continued to ambulate with a walker, without significant pain, for nine years until her death from other causes. The result from this patient was the beginning of our understanding that the SIJ can cause severe disabling pain and that a fusion is a viable option in some patients (Fig. 5.4).


Fig. 5.4
Nine-year follow-up of elderly patient with severe rheumatoid arthritis and osteoporosis after fusion of her sacroiliac joint using a plate and cancellous screws
Our experience with fusing patients with inflammatory arthritis has been mixed. It contains some of our very best and also some of our worse results. Currently, our feeling is that if it involves one joint and the patient does not have other systemic problems arising from their inflammatory arthritis diagnosis, they seem to respond the best to the surgery. If their condition is bilateral and they suffer with pain from multiple other sites related to the inflammatory process, caution should be taken when considering surgery. This situation is illustrated in the case shown in Fig. 5.5. Although some cases of inflammatory arthritis have done very well with fusion procedures others have not. Much more research and experience are needed in patients with this diagnosis to fully understand which subgroups would be the most appropriate for fusion surgery. A rheumatologist might be able to manage their condition as a better option to surgery (Fig. 5.5).


Fig. 5.5
Middle-aged female with severe bilateral sacroiliitis after a bilateral posterior midline fusion using custom instrumentation (Medtronic). Note that the cages are not approved for this purpose by the FDA and they are used as custom devices without label. Although initially successful, her pain returned after several months with no loosening of hardware on CT noted. Screws and rods were removed without improvement of pain
Postpartum SIJ Dysfunction
The obstetrics and gynecology literature has recognized for decades the abuse that the SIJs endure as a result of carrying the baby during the final weeks of pregnancy and as a result of a vaginal labor and delivery [7–11]. In most cases, the endogenous factors that allow for the laxity and occasional injury to the ligaments surrounding the SIJ during labor and delivery reverse themselves, and the pain that was associated with this event subsides. In a small number of cases, the pain does not resolve, and the patient continues on with chronic pain. Typically, this pain is endured and possibly alters activities or lifestyle. Occasionally, it becomes progressively severe and begins to cause increasing levels of disability. These types of patients frequently populate chronic pain clinics and get repeated injections into the SIJ for short-term relief. It has only been recently that such a patient is being referred for possible surgery. It is usually the primary care doctor, the patient’s physical therapist, or a collaboration of both that sends this type of patient for a possible surgical solution. These patients are usually very frustrated and often depressed when they present to the surgeon for consultation. As a group, they also have the fewest findings on any imaging test. CT and the bone scan may be essentially normal. It will be the history that offers the clues to the etiology and the injection (Chap. 6) that ultimately solidifies the diagnosis.
Case Example
A patient, having a greater than 10-year follow-up at our institution, suffered from postpartum SIJ dysfunction. She also had a secondary diagnosis of HLA-B27-positive non-fusing ankylosing spondylitis. After the birth of her first child during her mid-20s, her pain slowly and steadily increased to a point of being very disabling. By the time we evaluated her in her late 40s, she had reached a point of constant pain and progressive inability to bear weight on her right leg and was having progressively more dyspareunia, receiving only short-term relief with injections, and becoming increasingly frustrated with her condition. After failing years of appropriate conservative treatments, she underwent a posterior SIJ fusion. At an 11-year follow-up, she was still having significant pain relief and increased functional ability. Her dyspareunia improved significantly as well. She remains very satisfied with her outcome and would do it again for the same result. This patient has gone on to council other patients with chronic SIJ dysfunction (Figs. 5.6 and 5.7).

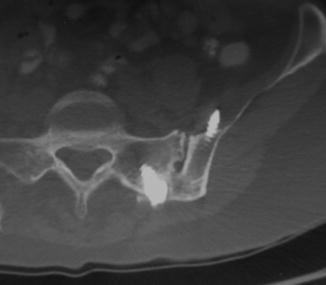

Fig. 5.6
Greater than 10-year follow-up AP X-ray of a right posterior midline sacroiliac joint fusion
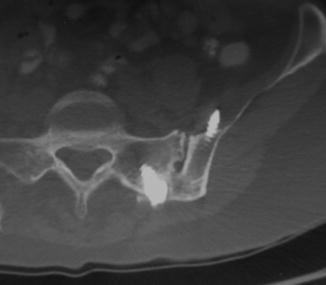
Fig. 5.7
Axial CT scan showing a solid sacroiliac joint fusion at greater than 10 years after a posterior midline sacroiliac joint fusion. Note the tip of the iliac screw in the iliacus muscle. This did not cause a problem and may have strengthened the stabilization with the cortical fixation of the medial iliac wall
Sacral Osteoporosis
This can be a very challenging condition, which can present to the clinician in various ways. We have encountered painful, dysfunctional SIJs adjacent to healed sacral insufficiency fractures due to osteoporosis, in RA, lupus, and Reiter’s syndrome with their associated osteoporotic states, and after sacroplasties, which inadvertently injured the SIJ. Osteoporosis becomes very important for the surgeon to understand when considering the quality of the bone-instrumentation interface available in a patient needing a SIJ fusion. The sacrum, which consists of primarily cancellous bone, may have very little fixation potential for laterally based fusion systems. In these patients, it is important to consider other fixation points such as the S1 pedicle, placing the iliac screw between the cortical layers of the ilium allowing for more cortical bone surface area capture or considering posterior lateral into or obliquely crossing the longitudinal axis of the joint fixation where there might be more of a stronger subchondral cortical bone available in the osteoporotic patient (Fig. 5.8).


Fig. 5.8




Placing a cage into the sacroiliac joint as part of a posterior midline sacroiliac joint fusion. The sacroplasty, done elsewhere, entered the sacroiliac joint causing joint damage and resultant chronic pain. The fusion procedure relieved this iatrogenically caused pain
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







