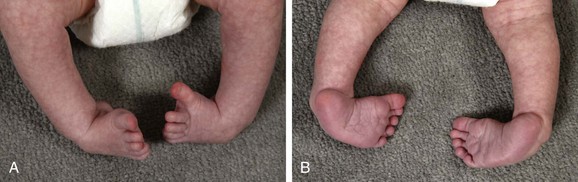
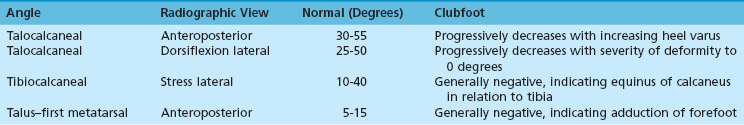
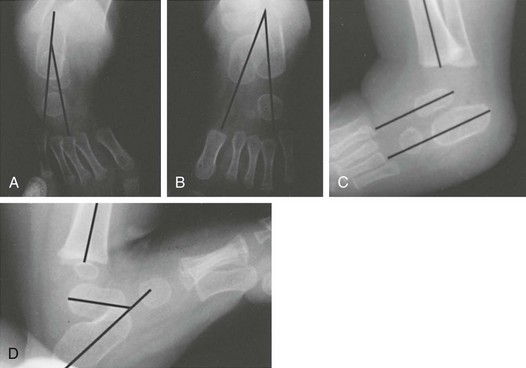
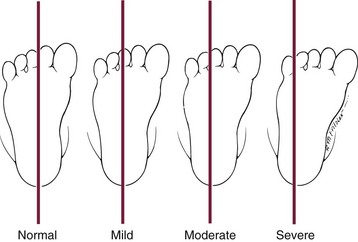
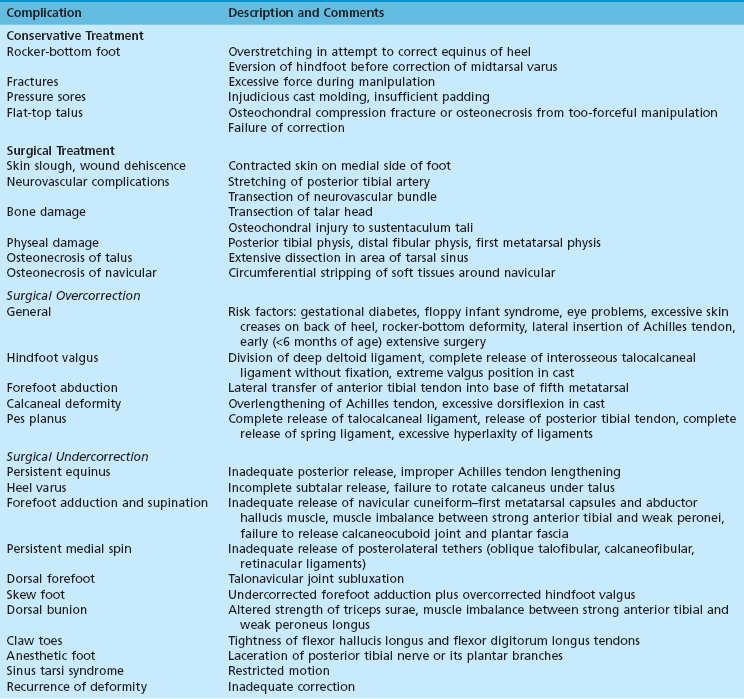
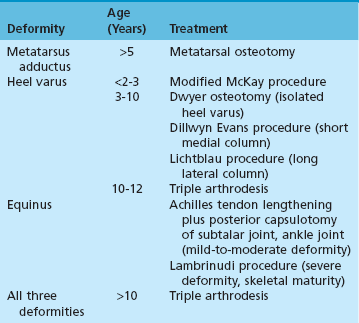
Chapter 33 The skeletal elements of the foot are blastemic by the fifth gestational week; all are present and begin to chondrify between 5 and 6.5 weeks prenatally. The cartilage anlagen of the individual bones ossify slowly and in a regular pattern, beginning with the phalanges and metatarsals at 9 weeks. The calcaneus is the first tarsal bone to ossify and does so between 20 to 24 weeks, followed by the talus at 32 weeks. The remaining tarsal bones ossify after birth, with the navicular being last—not ossifying until the third to fourth postnatal year.16 Between 5 and 7 weeks after conception, the blastemas have differentiated into elements arranged like those of an adult. Individual elements of the limb generally appear in a proximal-to-distal sequence, and the specific time of differentiation has been determined with reasonable accuracy.65 Knowing the time of blastemic insult in a specific skeletal abnormality allows a search for less obvious congenital malformations in organs that differentiate at precisely the same time.63 Clubfoot (talipes equinovarus) occurs in approximately 1 of every 1000 live births. The ratio of idiopathic clubfoot among males to females is 2 : 1 and is consistent across ethnic groups.28 Bilateral deformities occur in 50% of children. Approximately 80% of clubfeet are isolated (idiopathic) birth defects, while the remaining 20% are associated with neuromuscular conditions and genetic syndromes. Although clubfoot may infrequently be inherited in an autosomal dominant manner, the majority of clubfoot cases are sporadic, supporting the notion that clubfoot is a complex trait and not a single-gene disorder. An important role for genetic factors in clubfoot etiology is supported by high concordance rates in identical twins compared with fraternal twins (33% vs. 3%).115 Additional evidence of genetic effects is provided by differences in clubfoot prevalence across ethnic populations, with the lowest prevalence in the Chinese population (0.39 cases per 1000 live births) and the highest in Hawaiians and Maoris (7 per 1000).10,28 A significant role for hindlimb-specific transcription factors in the etiology of clubfoot has recently been demonstrated through genome-wide studies of copy-number variants associated with clubfoot susceptibility. Specifically, there is strong support for the PITX1-TBX4 developmental pathway as one mechanism of pathogenesis, including the presence of PITX1 mutations and deletions in clubfoot families.5,6,74 Chromosome 17q23 duplications that include TBX4 were found in 4 out of 66 familial clubfoot patients and appeared to be associated with possible increased risk of hip dysplasia and poor treatment response.4 Clinically, children with clubfoot have a hypotrophic anterior tibial artery, in addition to the obvious atrophy of the musculature around the calf. Muir et al135 examined 94 parents of children with clubfoot and found an increased prevalence (3%) of an absent dorsalis pedis artery compared with a control group, implying that the anomaly is part of the genetic disposition passed on by the parents, as well as a factor in the development of clubfoot. Dobbs et al39 described absence of the posterior tibial artery in two children with idiopathic clubfoot and noted that absence of this artery found during surgical dissection should serve as a warning of potentially precarious circulation. Research studies of patients and mice with PITX1 mutations also show hypoplastic lateral arteries, suggesting that these vascular abnormalities may have a genetic basis.6 Muscle abnormalities indicate that clubfoot may be heterogeneous in etiology. Several authors have documented abnormal distribution of types I and II muscle fibers in clubfeet.68,89,91,100,162 Feldbrin et al60 found muscle imbalance in 83% of 52 children with clubfoot and suggested that peripheral nerve abnormalities or spinal cord dysfunction might contribute to clubfoot deformity. Ippolito87 noted that genetically induced fibrosis of muscle-tendon units in the leg and foot also may be an important factor in clubfoot deformity. The abnormal foot may be as much as a half to one size smaller in both length and width. Reduced muscle mass has been confirmed by magnetic resonance imaging (MRI) studies88 and also appears to correlate with abnormal vasculature in human patients and genetic models.6 Clubfoot has a distinct clinical appearance that is recognizable at birth, consisting of forefoot cavus and adduction as well as hindfoot equinus and varus (Fig. 33-1). It is often accompanied by internal tibial torsion and the ankle, midtarsal, and subtalar joints all are involved in the pathologic process. Although the severity of every clubfoot may differ a common feature of all clubfeet is that the deformities cannot be fully corrected passively on initial examination. Because available classification schemes for clubfoot do not take into account its etiology, they are of limited use in predicting response to treatment. The authors have found that the most prognostic way in which to classify clubfoot is into one of two groups: isolated and nonisolated. Isolated clubfoot is the most common of the two and occurs in children without any other associated anomalies. Nonisolated clubfoot constitutes a broader group and includes clubfeet associated with neuromuscular or genetic syndromes, as well as clubfeet with congenital nerve deficiencies54 and/or decreased lower leg muscle volumes.127 Turco,175 in the early 1970s, attributed the deformity to medial displacement of the navicular and calcaneus around the talus, and his observations at surgery have helped to delineate more clearly the bony deformities in the clubfoot. According to Turco, the talus is forced into equinus position by the underlying calcaneus and navicular, and the talar head and neck are deviated medially. The calcaneus is inverted under the talus, with the posterior end displaced upward and the anterior end displaced downward and medially. McKay122–124 added an awareness of the three-dimensional aspect of bony deformity of the subtalar complex in clubfoot. According to his description, the relationship of the calcaneus to the talus is characterized by abnormal rotation in the sagittal, coronal, and horizontal planes. As the calcaneus rotates horizontally while pivoting on the interosseous ligament, it slips beneath the head and neck of the talus anterior to the ankle joint, and the calcaneal tuberosity moves toward the fibular malleolus posteriorly. Thus the proximity of the calcaneus to the fibula results primarily from horizontal rotation of the talocalcaneal joint rather than from equinus. The heel appears to be in varus because the calcaneus rotates through the talocalcaneal joint in a coronal plane as well as horizontally. The talonavicular joint is in an extreme position of inversion as the navicular moves around the head of the talus. The cuboid is displaced medially on the calcaneus. Herzenberg et al79 demonstrated with three-dimensional computer modeling that in the clubfoot the talar neck is rotated internally relative to the ankle mortise, but the talar body is externally rotated in the mortise. Johnston et al94 described abnormal talar pronation that they called “in-torsion.” Herzenberg et al79 also showed the calcaneus to be significantly internally rotated with the sloped articular facet of the calcaneocuboid joint, causing additional internal rotation of the midfoot. Simons160 described the calcaneocuboid deformity in clubfoot as a combination of medial angulation of the calcaneocuboid joint with subluxation of the cuboid on the calcaneus. In 100 clubfeet that required surgical treatment, 30 had no calcaneocuboid joint abnormality, 45 had insignificant abnormalities, and only 25 had severe abnormalities that required calcaneocuboid release. Contractures or anomalies of the soft tissues exert further deforming forces and resist correction of bony deformity and realignment of the joints.86,87,90,180 Talocalcaneal joint realignment is opposed by the calcaneofibular ligament, the superior peroneal retinaculum (calcaneofibular retinaculum), peroneal tendon sheaths, and posterior talocalcaneal ligament. Resisting realignment of the talonavicular joint are the posterior tibial tendon, deltoid ligament (tibial navicular), calcaneonavicular ligament (spring ligament), the entire talonavicular capsule, dorsal talonavicular ligament, bifurcated (Y) ligament, inferior extensor retinaculum, and occasionally the cubonavicular oblique ligament. Internal rotation of the calcaneocuboid joint causes contracture of the bifurcated (Y) ligament, long plantar ligament, plantar calcaneocuboid ligament, navicular cuboid ligament, inferior extensor retinaculum (cruciate ligament), dorsal calcaneocuboid ligament, and occasionally the cubonavicular ligament. Radiographs are not necessary in the initial evaluation of isolated clubfoot in the newborn period. It is difficult to evaluate the extent of deformity in the infant and young child because the centers of ossification of the calcaneus, talus, and cuboid are small and oblong. In addition, the navicular, the most displaced component of the clubfoot deformity, does not ossify until the age of 3 or 4 years. Furthermore, Cooper et al31 reported, with an average 30-year follow-up, that residual deformity seen on foot radiographs did not predict success or failure of treatment. The potential danger with focusing on achieving “good” radiographic correction is that this will often lead the treating physician to perform more extensive surgical correction, which may result in feet that look good radiographically but do not function well clinically because of stiffness and the development of arthritis in the foot and ankle.43 Instead, radiographs are reserved for evaluating recurrent or neglected clubfoot or in situations where the foot may not be responding to conservative treatment and more extensive surgical treatment is being considered. In the nonambulatory child, standard radiographs include anteroposterior (AP) and lateral views of both feet. AP and lateral standing radiographs are desirable when possible. Important angles to consider in the evaluation of clubfoot are the talocalcaneal angle on the AP radiograph, the talocalcaneal and tibiocalcaneal angles on the lateral radiograph, and the talometatarsal angle (Fig. 33-2 and Table 33-1). Simons160 devised a radiographic system to evaluate the calcaneocuboid joint deformity in clubfoot. The four grades (0, 1, 2, and 3) are based on the extent to which the midpoint of the cuboid is deviated from the longitudinal axis of the calcaneus or beyond the tangent defined by the edge of the calcaneus (Fig. 33-3). In the 100 clubfeet in his series, grade 1 deformity did not require surgery, grade 2 deformity required extensive soft tissue release, and grade 3 deformity required a bone procedure in addition to extensive soft tissue release. Based on this sample, approximately 25% of all patients who need surgery require calcaneocuboid release. The use of computed tomography (CT)94,163 and MRI69 for further delineation of clubfoot deformity has been described, but these expensive procedures usually add little useful clinical information and are not routinely used. Several authors have reported the use of ultrasonography as a screening tool in infants, to monitor the success of conservative treatment, to guide surgical correction, and to evaluate intraoperative reduction.62,153 Proponents cite as advantages that ultrasonography is quick and simple, is easily tolerated by the child, and can be repeated frequently to monitor response to treatment. The goal with less surgically invasive clubfoot treatment is to provide functional correction with the advantages of creating less scar tissue, and, as a result, more supple feet than those treated with more extensive surgery.43 The two most commonly used methods are the French method and the Ponseti method. The French method, which relies on intensive physiotherapy and splinting, often results in incomplete correction of the hindfoot contractures, necessitating an extensive posterior soft tissue release operation to complete correction.150 The Ponseti method of serial casting, Achilles tendon tenotomy, and foot abduction bracing has become the gold standard for clubfoot treatment in North America as well as in many other parts of the world because it results in excellent long-term correction without the risks associated with more extensive surgical releases, which include stiffness of the foot, pain, arthritis, and the need for additional surgical procedures.43,147 From a global perspective, the Ponseti method has provided the opportunity to correct clubfeet in children in developing nations in which resources for surgical intervention are inadequate or lacking.171 Because of the high success rate with use of the Ponseti method in achieving correction in infants with isolated clubfoot, many have expanded the age range and used the method successfully to treat clubfoot children from the age of 1 to 9 years of age with previously untreated or neglected clubfoot,116 with one report of success in a previously untreated 19-year-old male with unilateral clubfoot (personal communication). Indications for use of the Ponseti method continually expand, with successful correction reported in patients with nonisolated clubfoot, such as those clubfeet associated with distal arthrogryposis, myelomeningocele, and a variety of other underlying neurogenic and syndromic disorders with which the associated clubfeet are severely rigid.1,19,67,75,129 With use of the Ponseti method for these difficult cases, the treating physician must have realistic expectations, depending on the underlying diagnosis. The goal for correction in many of these cases should be to achieve plantigrade and braceable feet. It is not reasonable, for instance, or necessary to obtain 30 degrees of ankle dorsiflexion in a child with arthrogryposis. To achieve the same degree of correction as one strives for with isolated clubfeet would require more extensive surgery and all of the short- and long-term problems that accompany this type of intervention. The Ponseti method has also been used successfully in regaining correction in patients who have relapsed after an extensive soft tissue release surgery.66 The argument, in fact, can be made that the Ponseti method should be the first line of treatment for any clubfoot, regardless of age at presentation, associated diagnoses, or whether the patient has had any previous treatment. If full correction is not obtained in the more difficult cases, then the partial correction achieved still lessens the amount of surgery that needs to be done, essentially turning the surgical procedure into an “a la carte” approach. Perhaps the most difficult part of clubfoot management is recognizing and treating relapse. Most relapses can be corrected with repeat casting alone or casting followed by transfer of the anterior tibial tendon to the third cuneiform. To help prevent relapse, patients are prescribed a foot abduction brace that parents are asked to use for up to 4 years. Not using the brace as prescribed is the most common reason given for relapse.46,111 Although all clubfeet are at risk for relapse, predicting which feet are more likely to relapse is quite difficult at this stage. Being able to classify patients based on risk of relapse is one of the goals of elucidating the genetic etiologies of clubfoot. The development of a genetic-based classification system will allow a more individualized approach to clubfoot management, resulting in those patients deemed at lower risk for relapse being prescribed a shorter duration of foot abduction bracewear. 1. The cavus is corrected first by supinating the forefoot and dorsiflexing the first metatarsal. It is essential to never pronate the forefoot because this worsens the cavus deformity. Supinating the forefoot achieves the first goal of correcting cavus by aligning the forefoot with the hindfoot. After stretching, the cast is applied. 2. The next week, the cast is removed in the clinic with either a cast saw or by soaking the plaster off. Except in severe clubfeet, the cavus usually is corrected with one cast. At this stage, the varus and adduction are addressed by abducting the foot in supination while counterpressure is applied with the thumb on the head of the talus. The calacaneus abducts by rotating and sliding under the talus while simultaneously extending and everting, thus correcting heel varus. After manipulation, a long-leg cast is applied as described above. With immobilization for 1 week in a cast, the tight medial and posterior ligaments begin to relax. 3. The child returns the following week for a repeat cast change. The same manipulation and casting described in step 2 is repeated. This is repeated weekly for a total of 4 to 5 casts to fully stretch the medial ligaments. It is important to never touch the calcaneus during manipulation, for if it is held, the calcaneus is prevented from sliding from varus to valgus. 4. Once the foot is externally rotated approximately 60 degrees and the hindfoot is in neutral to slight valgus, any residual equinus is corrected with a tenotomy of the Achilles tendon. This is done in the clinic with a local anesthetic for patients younger than 1 year and in the operating room for those older than 1 year or those having a repeat tenotomy where the tendon is less easily palpated. The indication for tenotomy is ankle dorsiflexion of less than 10 degrees. While an assistant holds the foot and leg, the surgeon performs a longitudinal stab incision just medial to the tendon and 1 cm above its insertion on the calcaneus. The tendon is cut completely from anterior to posterior. A snap is felt and a sudden increase in ankle dorsiflexion occurs. The final cast is applied with the foot in 70 degrees of external rotation and 10 degrees of dorsiflexion. This cast is left on for 3 weeks to allow the tendon to heal. After cast removal, the child is placed in a foot abduction brace to prevent relapse. The indications for extensive soft tissue release surgeries for clubfoot are decreasing as treating orthopaedic surgeons gain more experience with the broadened indications for use of the Ponseti method. Surgical correction for clubfoot should be reserved for those rare patients whose clubfeet cannot be adequately corrected with more conservative measures and for those clubfoot recurrences that, despite casting, have some residual deformity needing to be addressed. In any case, surgical correction for residual clubfoot should be approached with the philosophy that less is more. The release should be limited to only what is necessary to gain correction on each particular foot. The surgeon must resist the temptation to achieve a perfect radiographic correction but instead focus on trying to provide a plantigrade foot and preserve motion. Achieving a perfect radiographic correction leads to more extensive surgery and feet that are stiffer and at risk of becoming painful and arthritic, and it leads to a patient with a dramatically decreased quality of life.43 The optimal time for extensive soft tissue release surgery is somewhat controversial and ranges from 3 to 12 months of age. Kránicz et al,104 in a 20-year follow-up study of 41 surgically treated clubfeet, found significantly more abnormalities in patients in whom surgery was done after age 1 year. Simons160 stated that the size of the foot is more important than the age of the child and recommended surgery when the foot is 8 cm (about 3 inches) or longer. Carroll23 recommended surgery any time after age 3 months if the child weighs at least 5.5 kg (12 pounds) and is thriving. The current authors prefer to correct any residual clubfoot deformity between 9 to 12 months when the surgery is technically easier to do but also allows correction before walking age. The procedure for a complete extensive soft tissue release operation through a transverse circumferential incision, modified from that described by McKay,123 is described, but the authors’ current approach to residual clubfoot deformity is “a la carte,” in which only the tight structures are released, and a complete release is not performed in many patients. The procedure described by McKay111 takes into consideration the three-dimensional deformity of the subtalar joint and allows correction of the internal rotation deformity of the calcaneus and release of the contractures of the posterolateral and posteromedial foot. General principles for any one-stage extensile clubfoot release include release of the tourniquet at the completion of the procedure (obtaining hemostasis by electrocautery) and careful subcutaneous and skin closure with the foot in plantar flexion, if necessary to prevent tension on the skin. The foot can be placed in a fully corrected position 2 weeks after surgery at the first cast change. Surgery can be performed with the child supine or prone at the surgeon’s discretion. Several authors23,62 have noted that the use of a one-dose caudal anesthetic in addition to general endotracheal anesthesia makes the child more comfortable in the immediate postoperative period. With neurologic, electromyographic, and biopsy studies, Zanette et al186 found a high rate (70%) of myopathic changes in 17 infants with clubfoot surgery; they used light general anesthesia combined with regional anesthesia (caudal block or spinal anesthesia) without complications and recommended regional anesthesia and careful monitoring to prevent possible malignant hyperthermia, cardiorespiratory, or neurologic problems in children undergoing clubfoot surgery. A circumferential transverse (Cincinnati) incision33 provides excellent exposure of the subtalar joint and is useful in patients with a severe internal rotational deformity of the calcaneus. One potential problem with this incision is tension on the suture line when the surgeon attempts to place the foot in dorsiflexion to apply the postoperative cast. To avoid this, the foot can be placed in plantar flexion in the immediate postoperative cast and then in dorsiflexion to the corrected position at the first cast change when the wound has healed at 2 weeks after surgery. This cast change often requires sedation or general anesthesia on an outpatient basis. 1. The patient can be positioned prone or supine. Begin the incision on the medial aspect of the foot in the region of the naviculocuneiform joint (Fig. 33-4A). Carry the incision posteriorly, gently curving beneath the distal end of the medial malleolus and then ascending slightly to pass transversely over the Achilles tendon approximately at the level of the tibiotalar joint (Fig. 33-4B). Continue the incision in a gentle curve over the lateral malleolus, and end it just distal and slightly medial to the sinus tarsi (Fig. 33-4C). Extend the incision distally either medially or laterally, depending on the surgical requirements. 2. Preserve the veins on the lateral side if possible, protecting the sural nerve. Then dissect the subcutaneous tissue up and down the Achilles tendon to lengthen it at least 2.5 cm (1 inch) in the coronal plane. Incise the superior peroneal retinaculum off the calcaneus at the point where it blends with the sheath of the Achilles tendon. 3. Dissecting carefully, separate the calcaneofibular and posterior calcaneotalar ligaments, the thickened superior peroneal retinaculum, and the peroneal tendon sheath. Cut off the calcaneofibular ligament close to the calcaneus (this ligament is short and thick and attached very close to the apophysis). 4. Elevate the peroneal tendon sheaths and the superior peroneal retinaculum from the lateral side of the calcaneus, using sharp dissection but being careful not to cut the peroneal tendons. 5. Incise the lateral talocalcaneal ligament and the lateral capsule of the talocalcaneal joint from their attachment to the calcaneocuboid joint to the point where they enter the sheath of the flexor hallucis longus tendon posteriorly. In the more resistant clubfoot, the origin of the extensor digitorum brevis, cruciate crural ligament (inferior extensor retinaculum), dorsal calcaneocuboid ligament, and occasionally the cubonavicular oblique ligament must be dissected off the calcaneus to allow the anterior portion of the calcaneus to move laterally. 6. On the medial side, dissect free the neurovascular bundle (medial and lateral plantar nerves and associated vascular components) into the arch of the foot, taking particular care to preserve the medial calcaneal branch of the lateral plantar nerve. Protect and retract the neurovascular bundle with a small Penrose drain. Complete dissection of the medial and lateral neurovascular bundle throughout the arch of the foot, being careful not to enter the sheath of the flexor hallucis longus and flexor digitorum longus tendons or the posterior tibial tendon. 7. Enter the compartment of the medial plantar neurovascular bundle, and follow it into the arch of the foot well beyond the cuneiforms, taking down the master knot of Henry. Elevate the abductor hallucis muscle and the sheaths of the posterior tibial tendon and the flexor hallucis longus and flexor digitorum longus tendons. Section the narrow strip of fascia between the medial and lateral branches of the plantar nerve to allow the abductor hallucis to slide distally. 8. Enter the sheath of the posterior tibial tendon just posterior to and above the medial malleolus. Split the sheath and superficial deltoid ligament up the tibia until the muscle can be identified. Then lengthen the tendon by Z-plasty at least 2.5 cm proximal from the medial malleolus to the maximal distance allowed by the incision. 9. Starting from the point at which the flexor digitorum longus and the flexor hallucis longus tendons cross, sharply dissect both sheaths from the sustentaculum tali, moving in a proximal direction until the talocalcaneal joint is entered. 10. Continue the dissection down and around the navicular, holding the distal segment of the lengthened posterior tibial tendon attached to the bone. Open the talonavicular joint by pulling on the remaining posterior tibial tendon attachment, and carefully cut the deltoid ligament (medial tibial navicular ligament), talonavicular capsule, dorsal talonavicular ligament, and plantar calcaneonavicular (spring) ligament close to the navicular. 11. Enter and carefully expose by blunt dissection and retraction the interval between the dorsal aspect of the talonavicular joint and the extensor tendons and neurovascular bundle on the dorsum of the foot. Take special care not to dissect or disturb the blood supply to the dorsal aspect of the talus. 12. Follow through with the dissection, incising the capsule of the talonavicular joint all the way around medially, inferiorly, superiorly, and laterally. Inferior and lateral to the joint is the bifurcated (Y) ligament; incise both ends of this ligament to correct the horizontal rotation of the calcaneus. Complete the release of the talocalcaneal joint ligaments and capsule by incising the remaining medial and posteromedial capsule and superficial deltoid ligament attached to the sustentaculum tali. Do not incise the three talocalcaneal ligaments (interosseous ligament) at this point. 13. Retract the lateral plantar nerve and, using a periosteal elevator, detach the quadratus plantae muscle origin on the medial inferior surface of the calcaneus and expose the long plantar ligament over the plantar calcaneocuboid ligament and the peroneus longus tendon. At this point, the talus should roll back into the ankle joint, exposing at least 1.5 cm of hyaline cartilage on its body. If this does not happen, incise the posterior talofibular ligament. If the talus still does not roll back into the ankle joint, cut only the posterior portion of the deep deltoid ligament. Now the decision must be made as to the necessity of cutting the interosseous talocalcaneal ligament to correct the horizontal rotational abnormality through the talocalcaneal joint. This decision depends on the completeness of the correction and the mobility of the subtalar complex, as determined by the foot’s position. 14. Line up the medial side of the head and neck of the talus with the medial side of the cuneiforms, and medially push the calcaneus posterior to the ankle joint while pushing the foot as a whole in a posterior direction. Then examine the angle made by the intersection of the bimalleolar ankle plane with the horizontal plane of the foot; if the angle is 85 to 90 degrees, there is no need to cut the ligament. In children older than 1 year, however, such an incision generally is necessary because the ligament usually has become broad and thick, preventing derotation of the talocalcaneal joint. 15. After the foot has been satisfactorily corrected, pass a smooth Kirschner wire through the talus from the posterior aspect to the middle of the head. Positioning the pin in a slightly lateral direction in the head of the talus is beneficial in an older child with more pronounced medial deviation of the talar head and neck because it allows lateral displacement of the navicular and cuneiforms on the head of the talus to eliminate forefoot adduction. Pass the pin through the talonavicular joint and cuneiforms and out the forefoot on either the medial or the lateral side of the first metatarsal. 16. While an assistant is inserting the pin, mold the forefoot out of adduction. Cut off the end of the pin close to the body of the talus, and use a drill anteriorly to advance the pin out the forefoot until it is buried in the posterior body of the talus. 17. To correct rotation of the calcaneus beneath the talus, push the calcaneocuboid joint anterior to the ankle joint in a lateral direction while pushing the calcaneus posterior to the ankle joint in a medial and plantar direction. 18. Check for proper positioning of the foot; the longitudinal plane of the foot is 85 to 90 degrees to the bimalleolar ankle plane, and the heel under the tibia is in slight valgus. 19. If the entire talocalcaneal interosseous ligament was divided, insert a pin through the calcaneus, burying it deep in the talus from the plantar surface. Be careful not to penetrate the ankle joint. 20. Suture all tendons snugly with the foot in a maximum of 20 degrees of dorsiflexion. 21. After suturing the tendons, pull the sheaths of the flexor hallucis longus and flexor digitorum longus tendons down over them. 22. Reposition the lengthened posterior tibial tendon in its sheath, and repair the sheath beneath the medial malleolus. 23. With the fibrofatty tissue left attached to the calcaneus anterior to the Achilles tendon, cover the lateral aspect of the ankle joint. Keep the peroneal tendons and sheaths from subluxating around the fibula by suturing the sheath of the peroneal tendons to the fibrofatty flap. 24. Close the subcutaneous tissue and skin with interrupted sutures. 25. Apply a nonadherent dressing and then, very loosely, one or two layers of cast padding. Apply a long-leg bent-knee cast with the foot in plantar flexion and the knee in 90 degrees of flexion. Special attention should be given to two specific problems in clubfoot.37 The first is residual hindfoot equinus in children aged 6 to 12 months who have obtained adequate correction of forefoot adduction and hindfoot varus. This equinus can be corrected adequately by Achilles tendon lengthening and posterior capsulotomy of the ankle and subtalar joints without an extensive one-stage release. The clinical examination and radiographs must be reviewed carefully to be certain that a more extensive release is not required instead of a limited procedure that corrects only hindfoot equinus. The heel varus and internal rotation must have been corrected adequately if Achilles tendon lengthening and posterior capsulotomy alone are to be used. A number of complications can occur after either nonsurgical or surgical correction of clubfoot deformity.2,34,40 Most complications can be avoided by careful attention to technique (Table 33-2). Table 33-2 Complications of Treatment of Congenital Clubfoot Modified from Crawford AH, Gupta AK: Clubfoot controversies: complications and causes for failure. Instr Course Lect 45:339-346, 1996. Dorsal bunions after clubfoot surgery have been attributed to muscle weakness or imbalance. McKay123 reported dorsal bunions in 11 children after posteromedial release for clubfoot and attributed the deformity to weakness of the triceps surae: the bunion develops as the patient tries to push off with the toe flexors to compensate for the triceps weakness. Another suggested factor is imbalance between the anterior tibial muscle and an impaired peroneus longus muscle. Most authors recommend transfer of the flexor hallucis longus to the neck of the first metatarsal, combined with bone correction by plantar closing-wedge osteotomy of the first metatarsal.185 Treatment of residual or resistant clubfoot in older children is one of the most difficult problems in pediatric orthopaedics.7 The deformity can take many forms, and there are no clear-cut guidelines for treatment. Each child must be carefully evaluated to determine what treatment will best correct the particular functional impairment. Thorough physical examination should include careful assessment of the forefoot and hindfoot. Residual forefoot deformity should be determined to be either dynamic (with a flexible forefoot) or rigid. The amount of inversion and eversion of the calcaneus should be determined, as well as dorsiflexion and plantar flexion of the ankle. Any prior surgical procedures that have caused significant scarring of the foot or loss of motion should be noted. AP and lateral radiographs of the standing child should be obtained to assess anatomic measurements; if the clubfoot deformity is unilateral, the opposite foot may be used as a control for measurements. All possible etiologic factors of the persistent deformity, including underlying neuropathy, abnormal growth of the bones, osteonecrosis of the talus, and muscle imbalance, should be investigated. In a group of 159 clubfeet that required repeat surgery for residual deformities, Tarraf and Carroll169 found that the most common persistent deformities were forefoot adduction and supination (95% of feet) and that these deformities resulted from undercorrection at primary surgery. Undercorrection resulted from failure to release the calcaneocuboid joint and plantar fascia and failure to recognize residual forefoot adduction on intraoperative radiographs. As mentioned earlier, the initial approach to these difficult clubfeet should be with use of the Ponseti method.66 At a minimum, the method allows partial correction of the deformities that then simplifies the approach for achieving full correction, often eliminating the need for extensive soft tissue releases while relying on extraarticular bone osteotomies that tend to cause less stiffness long term.31,180 The appropriate procedures and combination of procedures depend on the age of the child, the severity of the deformity, and the pathologic processes involved.84,85 Table 33-3 outlines general guidelines for use in decision making. Table 33-3 Treatment of Resistant Clubfoot From Beaty JH. Congenital anomalies of the lower extremity. In Canale ST, editor: Campbell’s operative orthopaedics, ed 10, St Louis, 2003, Mosby, p 1000. Correction of the forefoot with residual adduction or supination, or both, is similar to that of isolated metatarsus adductus by multiple metatarsal osteotomies or by combined medial cuneiform and lateral cuboid osteotomies85,121,141 when the deformity is in the midfoot. For isolated heel varus with mild supination of the forefoot, a Dwyer osteotomy51,52 with a lateral closing wedge of the calcaneus can be used.84 Opening-wedge osteotomy of the calcaneus occasionally is followed by sloughing of tight skin along the incision over the calcaneus. Consequently, although some height of the calcaneus is lost after a lateral closing-wedge osteotomy, most authors now prefer a lateral closing-wedge osteotomy with Kirschner wire fixation if necessary. The ideal age for this procedure is 3 to 4 years, but there is no upper age limit. If the hindfoot deformity includes heel varus and residual internal rotation of the calcaneus with a long lateral column of the foot, the Lichtblau procedure may be appropriate. This procedure corrects the long lateral column of the foot by a closing-wedge osteotomy of the lateral aspect of the calcaneus or cuboid enucleation. Best results with this procedure are obtained in children aged 3 years or older in whom the calcaneus and lateral column are long relative to the medial column and the talus. This procedure can cause less long-term hindfoot stiffness than the Dillwyn Evans56 calcaneocuboid resection. Potential complications include development of a Z-foot or skew-foot deformity. If all three deformities are symptomatic in a patient older than 10 years, triple arthrodesis may be appropriate. Although triple arthrodesis and talectomy generally are salvage operations for uncorrected clubfoot in older children and adolescents, Galdino et al64 reported excellent or good results in 68% of 19 triple arthrodeses in children aged 10 years or younger (average age at surgery, 8.4 years) with severe hindfoot deformity after failure of soft tissue release. Nonunion occurred in 7% of joints, and fair and poor results primarily were caused by residual rather than recurrent deformity. The authors believe that triple arthrodesis is functionally and cosmetically superior to talectomy. Triple arthrodesis corrects the severely deformed foot by a lateral closing-wedge osteotomy through the subtalar and midtarsal joints. Functional results are generally improved despite postoperative joint stiffness. Talectomy should be reserved for severe, untreated clubfoot, previously treated clubfoot that is uncorrectable by any other surgical procedures, and neuromuscular clubfoot, particularly arthrogryposis. Metatarsus adductus, which consists of adduction of the forefoot in relation to the midfoot and hindfoot, is a fairly common anomaly, often causing in-toeing in children. It can occur as an isolated anomaly or in association with clubfoot. Although earlier studies92,108 indicated that metatarsus adductus was associated with developmental dysplasia of the hip, more recent studies143 have demonstrated no significant association between the two conditions. Clinically, metatarsus adductus can be classified as mild, moderate, or severe, as described by Bleck (Fig. 33-5).18 In the mild form, the forefoot can be clinically abducted to the midline of the foot and beyond (Fig. 33-6A). The moderate form has enough flexibility to allow abduction of the forefoot to the midline but usually not beyond (Fig. 33-6B). In rigid metatarsus adductus, the forefoot cannot be abducted at all. There also may be a transverse crease on the medial border of the foot or an enlargement of the web space between the great and second toes. In general, mild metatarsus adductus resolves without treatment. Moderate or severe metatarsus adductus is best treated initially by serial stretching and casting until the foot is clinically flexible.
Congenital Foot Deformities
Prenatal Development
Embryology
Clubfoot (Talipes Equinovarus)
Incidence
Etiology
Pathologic Anatomy
Radiographic Evaluation
Conservative Treatment
Ponseti Method
Technique
Surgical Treatment
Surgery for Clubfoot
Surgical Technique
Special Problems
Complications
Uncorrected or Residual Clubfoot in Older Children
Metatarsus Adductus
Evaluation and Classification
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Congenital Foot Deformities