Fig. 1
Anterior view of a patient with HSMN with bilateral cavus feet. Note the ability to see the heel from this view with the elevated arches. The posterior view clearly demonstrates the varus of the hindfoot
Intrinsic wasting → overpull of extrinsic musculature → claw toe deformity (Fig. 2).


Fig. 2
Multiple claw toes and significantly claw hallux are seen in more advanced stages of HSMN. Claw hallux and claw toes in young patients should always increase the suspicion of a neurologic disorder
Variable sensory deficits → can lead to recurrent ulceration, infection, and arthropathy.
Forefoot-driven hindfoot varus: deformity corrects with Coleman block test. Concomitant intrinsic hindfoot varus: deformity does not correct.
Treatment
UMN disorders:
Nonoperative Care
Physical therapy, stretching, maintenance of joint range of motion. Other modalities include splinting, serial casting, oral muscle relaxants, phenol and lidocaine nerve blocks, and botulinum type A toxin.
Phenol block have proven history with longer-lasting effect and are less expensive than botulinum toxin. However, botulinum toxin is easy to deliver since it needs only an injection into the muscle belly rather than precise injection around nerve.
Surgical Treatment
Address equinus deformity with open Z-lengthening or percutaneous lengthening.
Varus deformity addressed with split anterior tibialis tendon transfer (SPLATT) to lateral cuneiform or cuboid or total anterior tibialis tendon transfer to lateral cuneiform. Release of toe flexors often required.
Hereditary motor-sensory neuropathies (HMSN)
Flexible Deformity (hindfoot can be passively manipulated):
Nonsurgical management:
Not currently recommended given progressive pattern of disease
Surgical management:
Forefoot driven: closing wedge dorsiflexion osteotomy of first metatarsal (Fig. 3), release of plantar fascia, transfer of peroneus longus into peroneus brevis at level of distal fibula.
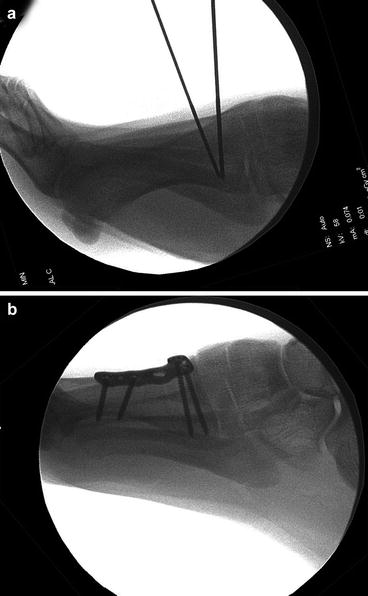
Fig. 3
Dorsiflexion osteotomy to correct the plantarflexed first ray is performed by marking the osteotomy with two K-wires (a). Following resection of the wedge, the osteotomy is closed and fixated with resultant elevation of the first ray (b)
Hindfoot driven: in addition to abovementioned procedures, include lateral calcaneal slide and/or closing wedge osteotomy (Fig. 4).
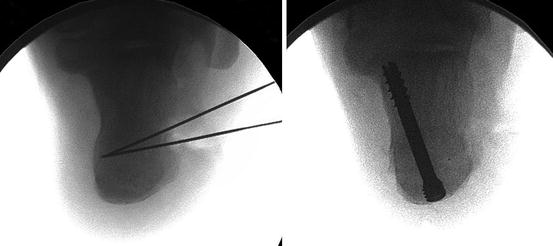
Fig. 4
Lateral closing wedge osteotomy of the calcaneus in a patient who had concomitant intrinsic hindfoot varus (failure to correct with Coleman block). This is performed in addition correction of the plantarflexed first ray and is not a substitute for a dorsiflexion osteotomy of the first metatarsal
Clawed hallux can be surgically treated with Jones procedure (arthrodesis of interphalangeal joint and transfer of EHL to the first metatarsal).
Consider posterior tibial tendon transfer to dorsum (lateral cuneiform) or lengthening of the tendon to restore balance.
Fixed Deformity (hindfoot cannot be passively manipulated):
Nonsurgical management:
Attempted with locked-ankle, short-leg ankle-foot orthosis with a lateral T-strap.
Rocker sole can improve gait and decrease energy expenditure.
Surgical management:
Triple arthrodesis usually required for hindfoot correction. Posterior tibialis tendon transfer through the interosseous membrane can correct equinus contracture and dorsiflexion weakness.
Must address imbalance of tendon forces even in the setting of an arthrodesis to prevent recurrence.
Dorsiflexion osteotomy of first metatarsal, release of plantar fascia.
Forefoot correction is performed according to the guidelines outlined previously.
Bibliography
1.
Botte MJ, Bruffey JD, Copp SN, Colwell CW. Surgical reconstruction of acquired spastic foot and ankle deformity. Foot Ankle Clin. 2000;5:381–416.
2.
Piazza S, Ricci G, Caldarazzo Ienco E, et al. Pes cavus and hereditary neuropathies: when a relationship should be suspected. J Orthop Traumatol. 2010;11:195–201.
3.
Roy DR, Al-Sayyad MJ. Complications of surgery of the foot and ankle in hereditary neurologic disorders. Clin Orthop Relat Res. 2001:181–7.
4.
Schenone A, Nobbio L, Monti Bragadin M, Ursino G, Grandis M. Inherited neuropathies. Curr Treat Opt Neurol. 2011;391(13):160–79.
5.
van der Ven A, Chapman CB, Bowker JH. Charcot neuroarthropathy of the foot and ankle. J Am Acad Orthop Surg. 2009;17:562–71.
2 Rheumatoid Foot
Take-Home Message
Rheumatoid arthritis is a chronic autoimmune disease that results in polyarthropathy that commonly involves the forefoot.
Typical deformity includes dorsal and valgus toe deviation, claw toe deformity, and pes planovalgus.
Conservative treatment involves proper shoe and orthotic wear and immune-modulating drugs under the direction of a rheumatologist.
Surgical treatment of the forefoot includes first MTP arthrodesis, lesser MT head resections, osteoclasis of interphalangeal joints, and extensor brevis tenotomy, while midfoot or triple arthrodesis is needed for pes planovalgus deformity in the rheumatoid foot.
Definition
Chronic, symmetrical polyarthropathy that most commonly presents in the third and fourth decades and is more prevalent in women
Etiology
Autoimmune disease with a genetic predisposition
Cell-mediated immune response against soft tissues, cartilage, and bone
Pathophysiology
ESR, CRP will be elevated, and RF titers positive (most commonly IgM).
Chronic synovitis leads to ligament and capsular laxity and cartilage and bony erosion.
Forefoot involvement very common:
Complaints of forefoot swelling, poorly defined pain, and eventually deformity.
Incompetence of joint capsules and lateral ligaments causes toes to subluxate or dislocate dorsally and deviate into valgus (Fig. 5).

Fig. 5
Clinical photograph of a patient with RA with swelling of the digits and characteristic valgus deviation of all digits with claw toes
Contracture of the intrinsic musculature exacerbates claw toe deformity.
Plantar fat pad migrates distally and atrophies, causing metatarsalgia and forming keratoses.
As lesser toes deviate, hallux valgus occurs, and transfer metatarsalgia worsens (Fig. 6).

Fig. 6
In severe cases, the joint laxity that occurs results in significant hallux valgus with overlap of the second toe over the first
Midfoot and hindfoot less commonly and less severely involved:
Midfoot/hindfoot arthrosis often results in pes planovalgus deformity that can be midfoot driven (tarsometatarsal joints are subluxated with a congruent hindfoot) or hindfoot driven (transverse tarsal and subtalar joint is subluxated with normal midfoot).
Tibiotalar joint is also commonly involved and may be caused by chronic subtalar joint malalignment.
Radiography
Can have significant midfoot and hindfoot arthrosis (talonavicular joint is characteristic)
Typically has diffuse osteopenia, symmetrical joint space narrowing, and lack of osteophyte formation (which easily differentiates RA from osteoarthritis) (Fig. 7)

Fig. 7
Typical radiographic appearance of a patient with RA. Note the multiple joint involvement with symmetric joint space narrowing, osteopenia without osteophyte formation with associated pes planus deformity. The typical dislocation of the lesser MTP joints can be noted as well
Treatment
Vasculitis and soft tissue fragility is common, requiring diligent care of the soft tissues regardless of treatment.
Conservative
Rest, NSAIDs, immune-modulating drugs under the direction of rheumatologists, toe taping, orthoses, careful use of corticosteroid injections to help symptoms related to synovitis, and patient education
Surgical
Should discuss use of immune-mediating pharmacologic therapies with rheumatologist prior to surgery → while most medications can be continued (prednisone, methotrexate, plaquenil), the newer biologic agents (such as TNF inhibitors) should be discontinued.
“Rheumatoid forefoot reconstruction” for deformity correction:
First MTP arthrodesis, lesser metatarsal head resection with pinning of lesser MTP joints, closed osteoclasis of interphalangeal joints versus PIP arthroplasty (silicone arthroplasty not recommended) through the use of three dorsal incisions. Extensor brevis tenotomy and Z-lengthening of extensor longus tendons may be necessary (Fig. 8).

Fig. 8
Preoperative AP radiograph (a) of a patient with RA with clinical hallux valgus with subluxation of the lesser MTP joints. Post-op AP radiograph (b) demonstrating excellent alignment following first MTP arthrodesis with metatarsal head resection of joints 2–5 and osteoclysis of the PIP joints. Interposition of the extensors into the potential space created may decrease risk of late subluxation
Pes planovalgus: Midfoot driven, realignment midfoot arthrodesis. Hindfoot-driven and fixed deformity, triple arthrodesis
Tibiotalar arthrosis: Ankle arthrodesis is treatment of choice, ankle arthroplasty emerging as more reliable technique (though it is associated with increased risk of wound complications).
Complications
Wound complications common following surgical treatment.
Current literature controversial whether patients on immunosuppressive therapies have significantly increased infection rates.
Late recurrence of deformity has been reported and some consideration for joint sparing lesser toe surgery has been considered. However, no long-term data to support joint sparing treatment to date.
Bibliography
1.
Aronow MS, Hakim-Zargar M. Management of hindfoot disease in rheumatoid arthritis. Foot Ankle Clin. 2007;12:455–74, vi.
2.
Goodman SM, Paget S. Perioperative drug safety in patients with rheumatoid arthritis. Rheum Dis Clin North Am. 2012;38:747–59.
3.
Jeng C, Campbell J. Current concepts review: the rheumatoid forefoot. Foot Ankle Int. 2008;29:959–68.
4.
Loveday DT, Jackson GE, Geary NP. The rheumatoid foot and ankle: current evidence. Foot Ankle Surg. 2012;18:94–102.
5.
Sammarco VJ. Ankle arthrodesis in rheumatoid arthritis: techniques, results, and complications. Foot Ankle Clin. 2007;12:475–95, vii.
3 Nerve Entrapment Syndromes
Take-Home Message
Nerve entrapment related to space-occupying mass is more likely to improve with surgical treatment than nerve entrapment without a related mass.
The first branch of lateral plantar nerve compression between the fascia of abductor hallucis and quadratus plantae is the most common cause of nerve-related heel pain, common in running athlete.
Superficial peroneal nerve entrapment related to chronic ankle instability and peroneal muscle herniation through fascial defect.
Nerve entrapment syndromes most commonly cause neuropraxia type of nerve injury with nerve contusion and focal demyelination of axon sheath.
Definition
Nerve Entrapment
Localized pressure causing nerve dysfunction.
Tarsal tunnel syndrome → tibial nerve:
Boundaries – flexor retinaculum (medial); talus, calcaneus, sustentaculum tali (lateral); abductor hallucis (inferior)
Additional contents – tendons of tibialis posterior, flexor hallucis longus, flexor digitorum longus, posterior tibial artery, venae comitantes, numerous septa
First branch of lateral plantar nerve (Baxter’s nerve)
Anterior tarsal tunnel syndrome → deep peroneal nerve
Boundaries – inferior extensor retinaculum (anterior), tibia and talus (posterior)
Additional contents – dorsalis pedis artery
Superficial peroneal nerve.
See Table 1 for symptoms and physical exam findings.
Table 1
Nerve entrapment symptoms and physical exam findings
Symptoms
Physical exam findings
Tarsal tunnel syndrome
Burning sensation of plantar foot, medial ankle
Positive Tinel and nerve compression tests
Plantar foot numbness variable
Pain with dorsiflexion-eversion
Worse with prolonged standing, walking, running
Diminished two-point discrimination
Wasting of intrinsic musculature
Hindfoot valgus, pes planus
First branch of lateral plantar nerve
Chronic heel pain, pain at plantar medial foot, may radiate laterally
Maximal point of tenderness at site of compression by fascia of abductor hallucis and quadratus plantae
Symptoms similar to plantar fasciitis
Symptoms without weight bearing
Wasting of abductor digiti quinti
No numbness – nerve has no sensory innervation
Anterior tarsal tunnel syndrome
Burning pain in dorsal first webspace
Positive Tinel sign
Vague dorsal foot pain
Diminished two-point discrimination
Worse at night with foot in plantarflexion
Forced ankle plantarflexion reproduces symptoms
Worse with shallow, laced shoes
Weak great toe extension
Superficial peroneal nerve
Pain and paresthesias radiating to dorsum of foot
Positive Tinel sign
Numbness is variable
Diminished two-point discrimination
Symptoms increase with activity
Palpable fascial defect and peroneal herniation
May feel a bulge at lateral leg – area of muscle herniation
Forced plantarflexion and inversion reproduces symptoms
Signs of ankle instability
Etiology
External compression from adjacent structures – tenosynovitis, engorged or varicose veins.
Space-occupying mass – synovial or ganglion cyst, pigmented villonodular synovitis, nerve sheath tumors, lipomas (Fig. 9).
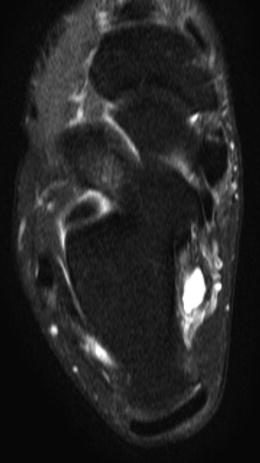
Fig. 9
Axial T2 fat-saturated image of a patient with tarsal tunnel syndrome that was noted to have a ganglion within the tarsal tunnel that required excision in addition to decompression of the nerve
Systemic disease can cause compression indirectly due to inflammatory edema – diabetes mellitus, rheumatoid arthritis.
See Table 2 for nerve-specific etiologies.
Table 2
Nerve entrapment etiology
Etiology
Tarsal tunnel syndrome
Increased nerve tension from hindfoot valgus and pes planus
Fracture of sustentaculum tali, medial tubercle of posterior process of talus
Accessory muscle
First branch of lateral plantar nerve
Compression between fascia of abductor hallucis and quadratus plantae
Lateral plantar nerve injury can occur from insertion of intramedullary nail for tibiotalocalcaneal fusion
Anterior tarsal tunnel syndrome
Anterior osteophytes of tibiotalar or talonavicular joints
Tightly laced shoes
Superficial peroneal nerve
Chronic ankle instability
Herniation of peroneal musculature through fascial defect
Iatrogenic injury
Pathophysiology
Pressure on nerve causes ischemia and neuroma formation.
Neuroma contains bundled disorganized nerve endings within collagenous mass.
Can result in loss of sensory and motor function.
Pain and paresthesia replace normal sensation.
Radiography
Weight-bearing radiographs of the foot and ankle
Detect bony abnormality causing or contributing to nerve entrapment.
Evaluate alignment of foot and ankle.
Rule out other source of symptoms.
MRI – if concern for space-occupying mass
EMG and NCV – can help confirm diagnosis but variable sensitivity
Classification
Seddon Classification
Neuropraxia – nerve contusion, focal demyelination of axon sheath, no Wallerian degeneration, good prognosis
Most common resulting injury following nerve entrapment:
Axonotmesis – axon and myelin sheath disruption, Wallerian degeneration, endoneurium intact
Neurotmesis – complete disruption of nerve including endoneurium, Wallerian degeneration
Treatment
Nonoperative: first line unless a space-occupying mass is present
Activity modification
Medications
Nonnarcotic analgesics
Centrally acting anticonvulsants
Tricyclic antidepressants, selective serotonin reuptake inhibitors
Topically applied compounds – include local anesthetic, anti-inflammatory medication, capsaicin
Physical and occupational therapy
Injection of local anesthetic with or without corticosteroid medication
Useful for diagnosis
Operative: indicated after 3–6 months of unsuccessful conservative treatment
Complete nerve decompression (Fig. 10)

Fig. 10
Intraoperative photograph demonstrating an appropriate incision with decompression of the tibial nerve and the requisite branches. Note release of the abductor hallucis in the distal aspect of the incision, ensuring that both the medial and lateral plantar branches are adequately released
Removal of space-occupying mass if present:
Greater rate of surgical success if nerve compression secondary to space-occupying lesion
See Table 3 for nerve-specific treatment information.
Table 3
Nerve entrapment treatment options
Nonoperative
Operative
Tarsal tunnel syndrome
Medial heel and sole wedge if hindfoot valgus and pes planus
Identify nerve proximally
Release deep investing fascia proximally, flexor retinaculum, deep and superficial fascia of the abductor hallucis
Short period of immobilization with cast or boot
Assure that all branches – medial calcaneal, lateral plantar, medial plantar – are decompressed
Release all septa
First branch of lateral plantar nerve
Heel pad
Release superficial and deep abductor hallucis fascia
Arch support if pes planus
Remove heel spur if present
Release part of plantar fascia if appears pathologic
Anterior tarsal tunnel syndrome
Night splint
Incise inferior extensor retinaculum
Shoe tongue padding
Decompress both medial and lateral branch of nerve (divide 1 cm proximal to ankle joint)
Excise bone spur if present
Superficial peroneal nerve
Lateral shoe wedge
Identify nerve distally and trace proximally to level that it pierces crural fascia (10–12 cm proximal to tip of lateral malleolus)
Ankle brace
Partial fasciotomy
Physical therapy for peroneal strengthening and proprioception
Test for residual tethering with intraoperative plantarflexion
Correct concurrent ankle instability
Complications
Recurrence of nerve entrapment – most commonly due to incomplete decompression
Revision surgery – decreased success rate
Bibliography
1.




Ahmad M, Tsang K, Mackenney PJ, Adedapo AO. Tarsal tunnel syndrome: a literature review. Foot Ankle Surg. 2012;18(3):149–52.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






