Comprehensive Management of Maxillofacial Injuries
Moises Salama
Richard D. Klein
Brian M. Derby
The treatment of facial trauma can be quite challenging. The goals of treatment are threefold. First, the establishment of the preinjury appearance or aesthetics is of paramount importance. Second, the function of the facial skeleton and soft tissues must be restored. The final goal is minimization of the disability period. The philosophy of treatment has shifted from that of the 1970s, where broad exposure and fixation of all buttresses were practiced to the current practice of minimizing approaches and potentially morbid exposures. Additionally, the advent of microvascular tissue transfer has made treatment of previously untreatable injuries possible. Further, the use of plate and screw rigid fixation has supplanted the use of cumbersome external fixation devices and the instability of interfragment wire fixation.1
GENERAL CONSIDERATIONS
Mechanisms of Injury
The most common cause of facial injuries is motor vehicle crashes. Other causes include fights, motorcycle and bicycle crashes, industrial mishaps, and athletic injuries. The use of seat belts and air bags has reduced the incidence of facial fractures associated with motor vehicle crashes. In a comprehensive review of 73,000 patients from 1983 to 1994, Lee et al. in 2000 published that the male to female ratio is 2:1, average age is 33, and the overall mortality is 5.9%. This mortality increases to 17% with a concomitant brain injury. The pattern of soft tissue injury was usually T-shaped involving the forehead, periorbital region, nose, lips, and chin. Lim et al. looked at concomitant injuries with facial fractures. He observed that in motor vehicle accidents, more than 50% of victims sustained injuries to the head, face, and cervical spine. Contributing factors included the use of alcohol and drugs and emotional problems. Eleven percent of patients had injuries other than the facial skeleton, 8% had injured extremities, 4% had ocular injuries, and 1% had spinal cord injuries.1
Associated Injuries
As with all trauma patients, victims of facial injuries need to be ruled out for concomitant injuries. A thorough physical examination and diagnostic workup is essential. This includes examining the airway, looking for significant blood loss, and diagnosing a brain or spinal cord injury.
The Airway
With extensive trauma to the mandible or midface asphyxia is a potential problem. The mouth and nasal passage should be cleared of foreign bodies, broken teeth or dentures, or blood clots, which may cause obstruction. Unstable mandibular fractures have the potential to push the tongue posteriorly and obstruct the airway. These patients may insist on sitting up and this is feasible if other injuries will notbe exacerbated. Anterior traction on the jaw and tongue and placement of an oropharyngeal airway is an alternative
if the patient cannot sit up or be placed prone. Patients with massive hemorrhage or fractures of the nose, maxilla, and mandible with resultant soft tissue edema are especially at risk. Endotracheal intubation or an emergency airway such as a cricothyroidotomy may be indicated, especially in patients with a head injury and blunted reflexes.
if the patient cannot sit up or be placed prone. Patients with massive hemorrhage or fractures of the nose, maxilla, and mandible with resultant soft tissue edema are especially at risk. Endotracheal intubation or an emergency airway such as a cricothyroidotomy may be indicated, especially in patients with a head injury and blunted reflexes.
For surgical fixation of maxillary or mandible fractures, nasotracheal intubation is frequently used. However, orotracheal intubation can be used even in cases where maxillomandibular fixation (MMF) is necessary if the tube can be placed through a gap in the teeth or behind the last molar. Another technique used by some is to pass the tube through the floor of the mouth with an incision in the submental area. In patients with panfacial fractures where an endotracheal tube would interfere with the repair or those with head or chest injuries who cannot protect their airway, a tracheostomy is indicated. This also applies to patients with significant airway swelling who may or may not need intermaxillary fixation.
Hemorrhage
Displaced fractures and lacerations of the face can result in significant blood loss. Life-threatening hemorrhage can be seen in up to 5% of Le Fort type maxillary fractures. Seventy percent of these bleeds are from the internal maxillary artery and its branches. When the source is superficial, local pressure, packing, or ligation can be used for control. Temporary reduction of fractures can slow bleeding from fracture lines. For anterior nasal bleeds, nasal packing may be temporizing. If bleeding stops, nasal packing can be removed within 2 to 3 days. Deeper bleeding usually comes from the internal maxillary artery. This area can be difficult to access and control. The placement of Foley catheters, one in each nostril, with 30 to 50 mL balloons can temporize the bleeding along with nasal packing anterior to the balloons. The balloons are pulled snug against the posterior nasopharynx for maximal effect. This maneuver done for several hours with intermittently releasing the pressure usually stops the hemorrhage. Reported complications of this intervention include necrosis of the palate or columella (if the Foleys are secured against the columella).
Another method previously used to control bleeding is the use of external compression dressings or Barton bandages which encircle the head. These are rarely used now. For patients who continue to bleed despite more conservative measures, radiographic embolization is the next step. Complications from this procedure include facial nerve palsy, tongue necrosis, and stroke. Internal maxillary artery bleeds can be readily embolized with this technique. Bleeding that may not be embolized can be due to fractures in the anterior cranial fossa with transection through the carotid artery or veins such as the dural venous sinuses. These injuries can be defined by angiography and palliated with bilateral ligation of the external carotid arteries and superficial temporal arteries. Blood flow to the midportion of the face is diminished with this maneuver.
Brain Injury
When patients with facial fractures have concomitant head injuries, the focus of treatment should be to minimize secondary ischemia from brain edema, mass lesions, and hypothermia. Patients with head injury are stratified based on the Glasgow Coma Scale (GCS). This grading system has prognostic significance and patients with a GCS score of 3 have a very limited chance of survival. Prognosis also worsens with increasing age, decreasing mean arterial pressure, intracranial hypertension, and abnormal posturing. It should be noted though that even in patients in a coma, surgical treatment of facial injuries is not contraindicated. Patients can be monitored intraoperatively with intracranial pressure monitoring.
Cervical Spine Injury
Patients with multiple trauma, especially those with head and facial injuries, should be considered to have a spinal cord injury until proved otherwise. It is thought that approximately 10% of victims with facial injury have a concomitant cervical injury. The converse figure is 18%. Mandible fractures specifically are associated with upper cervical spine injuries. Studies indicate that these upper level injuries (C1-2) as well as lower C-spine injuries (C6-7) are the most commonly overlooked. This has been reported to occur in as many as 10% of cases. Therefore, it is imperative that these multitrauma patients be approached with a high level of suspicion.
Timing of Surgical Interventions
In the management of a multitrauma patient, the life-threatening injuries are treated first to optimize survival. Once these injuries are stabilized and the patient can tolerate surgical intervention, facial injuries and fractures should be treated as soon as possible. This optimizes aesthetic outcome, function, and makes fracture fixation easier. Other patients may not be able to tolerate surgery or may need definitive treatment for a graver injury. These patients should have their facial lacerations closed, their fractures grossly reduced, and may even be placed in temporary MMF. Many surgeons will subsequently wait until the edema subsides before attempting to operate on the facial skeleton. In any case, we do not recommend waiting any longer than 2 weeks postinjury before skeletal fixation to avoid having to deal with malunions, soft tissue contraction, and scar tissue.
Diagnostic Evaluation of the Facial Trauma Patient
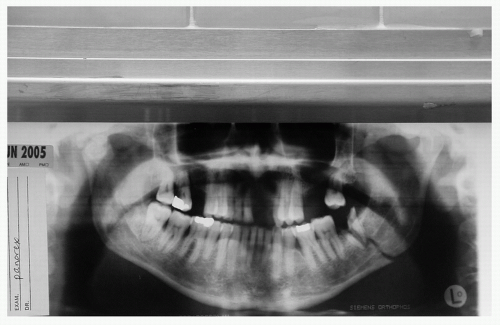
The diagnosis of facial injuries relies on a thorough physical examination and a supplemental radiologic assessment. Although many radiologic views of the face and head have been described, all of the information needed can be obtained from a dedicated craniomaxillofacial computed
tomography (CT) scan with coronal, axial, and sagittal views. The only conventional radiographs which are still justifiable are the panorex mandible radiograph (see Fig. 1) and dental views.
tomography (CT) scan with coronal, axial, and sagittal views. The only conventional radiographs which are still justifiable are the panorex mandible radiograph (see Fig. 1) and dental views.
The diagnosis of facial injuries is more difficult in children and the elderly.1 Even with apparently minor external injuries such as abrasions or contusions, significant fractures may be present. This is why a good history and physical examination is of paramount importance. Treatment of facial lacerations should not be deferred and may even be done in the emergency department. Lacerations and wounds should be copiously irrigated, debrided, and closed with a layered closure to optimize aesthetic result.
Signs and symptoms of facial injuries include pain, tenderness, crepitus, paralysis of a specific motor nerve, hypoor hyperesthesia, altered visual acuity, diplopia, dental malocclusion, facial deformity or asymmetry, lacerations, contusions, bleeding, edema, echymosis, and difficulty breathing. The examination should begin with inspection for facial asymmetry and deformity. Palpation should follow in a specific order. The bony prominences that should be palpated include the frontal bone, superior, lateral inferior and medial orbital rims, nose, zygomatic arches, malar eminence, maxilla, borders of the mandible, and alveolar ridges both maxillary and mandible (tooth-bearing segments).
Examination and palpation of the periorbital region should be carried out to check for tenderness, contour defects, and crepitus. One may find dystopia of the globes (unequal level), enophthalmos, proptosis, or diplopia, which may all indicate orbital, zygomatic, or maxillary fractures. Consultation with an ophthalmologist is indicated with injuries in this region to rule out globe injuries such as ruptures or retinal detachment. The eye examination should include visual acuity, extraocular movements, pupillary function, fundoscopic examination, and measurement of intraocular pressure. Extraocular movements may be assessed in the unconscious or sedated patient with a forced duction test. This involves grasping the conjunctiva of the globe with fine-toothed Adson forceps rocking the globe up and down as well as side to side to rule out muscle entrapment from an orbital fracture. Other signs that should be assessed include eyelid excursion, double vision, enophthalmos, hyphema, and corneal abrasions. Enophthalmos can be assessed by asking the patient to tilt his/her head back and comparing the corneal planes by looking in a cephalad direction. Any loss of vision or acuity should be documented preoperatively. Pupillary reactivity is also important to assess and is thought to be the most reliable sign of optic nerve injury.
The nasal examination should include an intranasal examination to look for soft tissue lacerations or septal hematomas. Externally, nasal trauma documentation should include the presence of nasal dorsum deformity and/or tip deviation, nasal bone collapse or instability, and presence of any lacerations.
In the awake patient, the muscles of facial expression (cranial nerve [CN] VII) and tongue function (CN XII) can be easily assessed. In the unconscious patient, initial CN motor function evaluation is not possible. Therefore, serial physical examination over a period of days is required to document CN function once the patient has become awake and cooperative.
In the examination of masticatory function, the maxillary and mandibular dental arches are inspected and palpated to look for irregularities of bone, lacerations, loose teeth, hematomas, swelling, crepitus, or tenderness. Dental occlusion and the intercuspal relationship of the teeth are checked and may be the only evidence of a fracture. Trismus may also be seen with zygomatic, maxillary, or mandibular fractures. A careful dental examination is performed to document the condition and quality of the patient’s dentition including the presence of decayed, fractured, or avulsed teeth. In condylar or subcondylar fractures, placing one finger in the ear canal and another over the condylar head may allow one to feel condylar movement or crepitus with jaw motion. In addition, one may see blood or fluid draining from the ear canal, which may indicate a laceration, a middle cranial fossa fracture with resultant cerebrospinal fluid (CSF) leak, or a condylar dislocation. Bleeding from the nasal passages may indicate nasal injuries, Le Fort fractures, orbital or nasoethmoid fractures, or anterior cranial fossa fractures. The mobility of the maxillary jaw should also be checked, for this also implies a Le Fort fracture. Finally, CSF rhinorrhea may be seen in anterior and middle basilar skull fractures, or cribriform plate fractures.
On neurosensory examination, one may find hypoesthesia or anesthesia in the distribution of one of the branches of the trigeminal nerve (CN V). This may indicate a fracture somewhere in the bony path of the nerve or injury from a soft tissue laceration. These nerves may be lacerated or just contused, implying neuropraxia. Neuropraxic nerves generally recover. These nerve branches travel through
foramina, which are weak parts of the bone and can fracture thereby crushing the nerve. Cutaneous branches are small and generally do not warrant repair. Larger branches such as the supraorbital, infraorbital, inferior alveolar, or mental nerves can be primarily repaired.
foramina, which are weak parts of the bone and can fracture thereby crushing the nerve. Cutaneous branches are small and generally do not warrant repair. Larger branches such as the supraorbital, infraorbital, inferior alveolar, or mental nerves can be primarily repaired.
Imaging
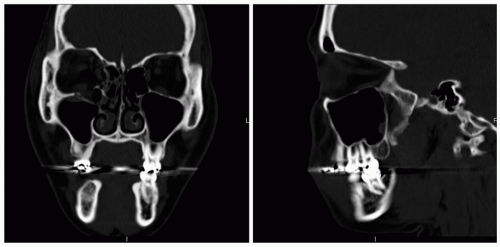
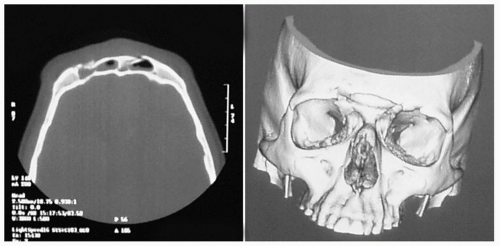
With the image resolution and quality available currently, the CT scan has supplanted plain radiographs in the diagnosis of maxillofacial trauma. The craniofacial CT must include axial, coronal, and sagittal sections with bone and soft tissue windows. This examination must be undertaken before any surgical intervention is commenced. Bone windows allow accurate visualization of fractures (see Fig. 2). Three-dimensional reconstructions can also be obtained to compare volume and symmetry between the two sides of the face. Further, special views such as the orbital apex view allow magnification into this area.
FACIAL SOFT TISSUE INJURIES
Etiopathogenesis
As previously mentioned, motor vehicle accidents are the most common source of facial soft tissue injury, with sports-related injuries, falls, altercations, and industrial accidents also contributing as common causes. These injuries include lacerations, abrasions, contusions, and avulsions. Treatment approach and potential complications are often dictated by type of injury encountered; therefore, accurate description of injury is imperative. Associated complications are also important to consider. Roughly 25% of facial lacerations resulting from motor vehicle accidents are accompanied by underlying facial bone fractures.2 A sound knowledge of facial anatomy will assist in evaluation of soft tissue injuries potentially involving salivary ducts, CN V and VII, facial mimetic muscles, and significant vessels.
Anatomy
The management of facial soft tissue injuries requires a thorough knowledge of facial anatomy. From superficial to deep, facial layers include skin, subcutaneous tissue, superficial musculoaponeurotic system (SMAS), fine areolar tissue, and mucosa. Understanding this blueprint assists in identifying structures involved in injury, and ensures that wounds are closed properly. Layered closure is important for attainment of the ultimate treatment objective, functional and cosmetic restoration.
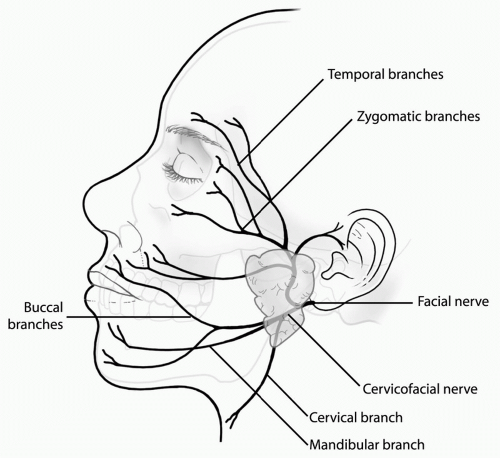
The facial nerve exits the skull at the stylomastoid foramen, enters the parotid gland, travels in the lateral aspect of the face deep to the facial mimetic muscles, and innervates them on the deep surface. Exceptions to this deep innervation include the buccinator, levator labii superioris, orbicularis oris, and the depressor angularis oris (see Fig. 3).
The parotid gland is located in the soft tissue of the lateral aspect of the face from the zygomatic arch superiorly to the mandibular angle inferiorly, and from the ear posteriorly to the midportion of the cheek anteriorly. The parotid duct travels along a transverse line from the tragus to the midportion of the upper lip and empties into the oral cavity, through the Stensen duct, opposite the second maxillary molar. The duct is often accompanied by the buccal branch of the facial nerve. Not uncommonly, both structures are simultaneously injured with lacerations to the lateral aspect of the face.
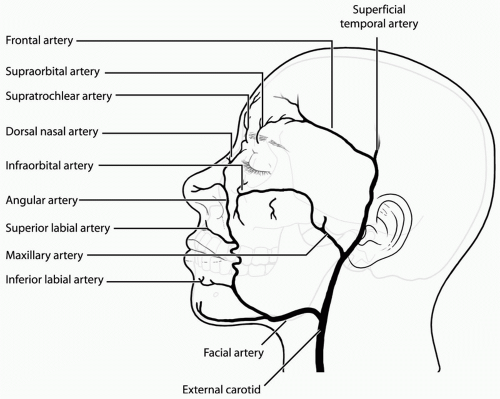
Blood supply is derived from branches of the external carotid artery—facial, internal maxillary, and superficial temporal (see Fig. 4). In the basilar skull region, tributaries of the internal jugular vein and intracranial circulation have valveless communication.
Lymphatics drain posteriorly and laterally. Avulsed tissue may have obstructed lymphatic drainage, frequently resulting in lymphedema. Trapdoor deformities, which are bulging soft tissue deformities that disrupt natural facial contours can result.
Diagnosis
Before the assessment of facial injury, the initial treatment of facial trauma patients focuses on management of life-threatening conditions. Following this initial evaluation, assessment of facial soft tissue injury can occur. A full facial examination is performed as previously described. This inspection should be performed in a systematic manner to avoid missing injuries. One can begin from the vertex of the head and proceed caudally from the top of scalp to the bottom of the neck.
The purpose of soft tissue wound inspection is to identify underlying damage and the presence of foreign material. The ends of transected structures, when isolated, can be made available for future repair. Foreign material serves to reduce the bacterial inoculum necessary to cause infection from 105 bacteria per gram of tissue to 102 per gram of tissue.
Bleeding, although initially best controlled with compression, is ultimately controlled with careful ligation. Recommendations for hemostasis caution against the use of cautery secondary to risk of damage to surrounding nerves, fat, and muscle. In the event that bleeding is slow to resolve, further investigation with arteriography may be required.
Insufficient hemostasis may result in hematoma. Like that found in any other region of the body, facial hematoma represents a nonvascularized region, inaccessible to antibiotics and white blood cells. Typically hematomas will resolve over time. The process may be expedited with application of warm, moist heat starting on day 3 after injury. Occasionally, a facial hematoma may be localized and considered fit for evacuation. This process is pursued under general anesthesia, with a suction tip advanced into the area of hematoma through a camouflaged incision. Patients must be warned of the risks of hyperpigmentation when hematomas are exposed to the sun.
General or local anesthesia is typically required during the inspection process, especially with pediatric patients.
One should also be sure to incorporate the use of extensive and accurate photographic documentation in their review. Photographs not only supplement and enhance medical documentation, but also enable the patient to appreciate the extent of injury and effectiveness of treatment.2
One should also be sure to incorporate the use of extensive and accurate photographic documentation in their review. Photographs not only supplement and enhance medical documentation, but also enable the patient to appreciate the extent of injury and effectiveness of treatment.2
Contamination is dependent on time elapsed since injury. A direct relationship exists between the time elapsed from injury to cleansing and the risk of contamination.2 Within the first few hours, inoculated organisms become encased in a protein-fibrin substrate that ultimately serves as a shield against antibiotics and dislodgment by normal irrigation fluids. More aggressive cleansing will require the use of surgical debridement, high-pressure irrigation, and scrubbing.
The surface of the skin, if contaminated by “traumatic tattoos,” should be freed of all foreign particles. Primary surface dermabrasion may risk extension of the depth of cutaneous injury and result in more prominent, hypertrophic scarring.2 Wound edges that are jagged and devitalized should be sharply excised. Typically, 1 to 2 mm of skin edge excision is all that is required to turn a traumatic wound into a surgically excised wound with improved cosmetic result upon closure. Very conservative excision is recommended in critical areas such as the eyelids, eyebrows, nostril rim, and the vermillion border, especially near the Cupid bow.2
Consideration of tetanus immunization status is also necessary, as all facial wounds are potentially contaminated. With obvious contamination, and no prior history of immunization, simultaneous injection of 250 IU of tetanus immune globulin and 0.5 mL of tetanus vaccine is recommended. The immunization is completed with two additional boosters at monthly intervals.
SPECIFIC FACIAL SOFT TISSUE INJURIES AND THEIR TREATMENT
Laceration Injury
Pertinent points to remember in repair of lacerated facial wounds are marginal edge excision and layered closure. Conversion of a crushed, devitalized, irregularly torn surface to a straight surgical incision enhances cosmesis upon closure while also reducing risk of infection. The basic sequence of facial closure entails repair of deeper structures—bone, glands, ducts, nerves—followed by approximation of muscle, fat, dermis, and epidermis. Fine grade absorbable sutures are used and should be strong enough to maintain dermal alignment after the skin sutures are removed on day 3 to 5. Early suture removal (within 5 to 7 postoperative days) prevents suture marks and further scarring. The physician should routinely inform a patient and his/her family about the possible need for future revision and/or reconstruction.
Bite Injury
Animal and human bites are not uncommon injuries. Significant points to remember with this injury are (a) the high likelihood of wound contamination secondary to extensive oral flora, and (b) the use of systemic antibiotic therapy is standard. Copious irrigation and sharp excision of contaminated wound edges is followed by prophylactic penicillin for potential Pasteurella multocida infection from cat bites, and broad-spectrum antibiotics for human bites (gram-positive, gram-negative, aerobic/anaerobic bacteria). The face is the only area where primary closure of bite wounds is considered, but debridement and irrigation must be thorough.
Facial Nerve Injury and Facial Muscle Injury
Wound inspection, combined with physical examination, may demonstrate laceration of the facial nerve. The extensive arborization and communication of the terminal branches of the facial nerve distal to a line drawn vertically from the lateral canthus may result in reduced functional deficit with injury to this region. Regardless, when able to be identified, transected nerve ends should be isolated and approximated with microsurgical techniques within 72 hours of injury.
Muscle realignment and approximation allows for some degree of nerve regeneration by neurotization of the muscle.2 Additionally, balance and activity of facial movement is better restored when muscle edges are approximated.
Trigeminal Nerve Injury
Sensory nerves of the face arborize extensively, calling the practicality of repair into question. Exceptions are made when nerve laceration occurs in close proximity to skull foramina (supraorbital, infraorbital, mental). Most commonly, one undertakes sensory nerve repair to prevent the development of painful neuromas.2
Parotid Gland Injury
Evidence of parotid duct injury can be confirmed by retrograde irrigation of the Stensen duct while looking for extravasation of fluid into the wound. Should a bony fracture be a component of the injury, duct repair should follow bony repair. The parotid duct falls along the middle third of a line drawn from the tragus to the midpoint of the upper lip. The buccal branch of the facial nerve is in close proximity to the parotid duct in this region.
The sequence of parotid duct repair includes dilation of the intraoral orifice with a lacrimal dilator, insertion of small silicone tubing into the duct ends as a stent, and suturing of duct ends over the silicone tubing with fine 8.0 nonabsorbable suture.3 Microsurgical technique
should be used. Parotid duct ligation is not recommended for two reasons. First, considerable gland swelling with secondary atrophy can occur and second, chronic infection requiring parotidectomy may develop.2 In contrast, damage to the submandibular gland or duct can be treated by duct ligation. Gland excision is another option for submandibular gland injury.
should be used. Parotid duct ligation is not recommended for two reasons. First, considerable gland swelling with secondary atrophy can occur and second, chronic infection requiring parotidectomy may develop.2 In contrast, damage to the submandibular gland or duct can be treated by duct ligation. Gland excision is another option for submandibular gland injury.
Eyelid Injury
Before eyelid repair, the importance of globe inspection and examination is paramount. This takes precedence over soft tissue restoration. Once assured, one proceeds with sequential conjunctival, tarsal, septal, levator, and orbicularis oculi repair with fine absorbable suture internally. Levator disruption may result in ptosis if not repaired. In closing external layers, sutures should be tied away from the globe to avoid corneal or conjunctival surface irritation.
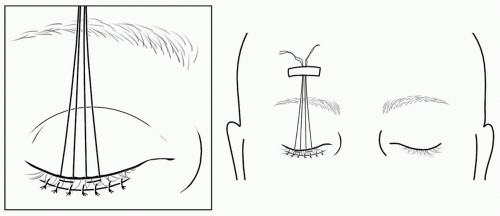
Lid defects can be closed with lid mobilization and lateral canthotomy. This release allows for medial mobilization of the remaining lower lid.2 Skin closure is performed with fine sutures. Proper alignment of the gray line, internal lid margin, and cilia is crucial to an esthetic and functional repair. In closing eyelid defects, one must be aware of the potential for development of ectropion. This occurs when the lid contracts from scarring and there is resultant scleral show. Techniques to prevent this complication include careful and meticulous closure of all anatomic layers after inferior orbital rim exposure as well as the application of Frost suture at the eyelid margin for 24 to 48 hours following the surgical intervention to maintain proper lid length (see Fig. 5). Participation in the care of these patients by plastic surgeon will help in obtaining optimal outcomes.
Lacrimal System Injury
Injury to the region of the medial canthus may result in damage to the lacrimal canaliculi or sac. This is assessed by cannulation of the puncta with a lacrimal probe. A laceration is proved by visualizing the probe in the wound. If an injury is present, the puncta are cannulated with Crawford tubes that are passed into the nose and are left in place for 4 weeks. If cannulation is not possible, lacerations are repaired and the patient may require a dacryocystorhinostomy if epiphora becomes problematic.4
Nasal Lacerations
Given its prominence, the nose is commonly involved with other soft tissue injuries of the face. Skin, cartilage, and mucous membrane defects must be managed separately in attempt to maintain nasal contour. In keeping with the concept of contour preservation, debridement should be kept to a minimum. Full-thickness lacerations are best repaired from the inside out. The nasal mucosa should be repaired with chromic sutures. The cartilage should be repaired with monofilament sutures. Lastly, the skin should also be repaired with monofilament sutures with good eversion of the skin edges.4 Significant soft tissue avulsion can be reconstructed with local or regional flaps to restore the mucosa, framework, and external skin. The use of cartilage grafts is often necessary. Any septal hematoma should be evacuated to prevent potential septal perforation.
Lip Lacerations
The facial soft tissue repairs discussed to this point have highlighted a consistent theme of attention to layered closure and proper edge alignment. Perhaps nowhere on the face is attention to this detail more important than the vermilion border of the lip. Skin, orbicularis oris, and mucosa must be precisely aligned and repaired, especially the pars orbicularis (thick band of orbicularis muscle) underneath the vermilion of the lip. The vermilion should be marked with methylene blue before the administration of local anesthesia, which can distort the landmarks. Although proper vermilion positioning is essential, one should keep in mind that approximation of the orbicularis muscle sets up alignment of the vermilion. As stated previously, debridement in this region should be minimized, especially in the area of the Cupid bow. Uncorrectable deformity can result.
Eyebrow Injury
Similar to lip lacerations, eyebrow injuries should be treated with minimal debridement. The eyebrow varies in thickness along its length. Resection almost assures a step-off deformity. Such deformities are only reparable by hair unit transplantation. Anatomic proximity should trigger inspection for supraorbital nerve injury and repair when feasible.
Auricle Injury
Like the nose, auricular protrusion leads to its frequent involvement in trauma. Further, the injured auricle is prone to hematoma formation. Hematomas must be evacuated and bolsters applied to prevent them. Drains can also be placed for 24 hours to reduce hematoma formation. Undrained hematomas can result in fibrosis and a “cauliflower ear” deformity. Avulsed tissue should be wrapped in sterile saline-soaked gauze, and placed in a plastic bag in a container on ice. Before replantation, wound edges are debrided as is cartilage stripped of perichondrium. After replantation of avulsed tissue, leech therapy should be initiated for 3 to 5 days until venous connections begin to develop. This will aid with necrosis from venous congestion. If the ear canal is involved, lacerations are repaired and the canal is stented to prevent stenosis.4 Secondary reconstruction may be necessary.
Significant Soft Tissue Defects
The scenario of avulsion injury or tissue loss that prevents primary closure may occur. These large wounds can be repaired with local undermining, local flaps, or skin grafting. Areas that may have compromised vascularity may be closed by delayed primary closure. This allows the wound to demarcate before definitive closure.
INJURIES TO THE FACIAL SKELETON
Frontal Sinus Fractures
Epidemiology
Frontal sinus fractures are relatively infrequent sequelae of facial trauma, occurring in approximately 5% to 15% of facial fractures.5 Typically, 60% of frontal sinus injuries involve both anterior and posterior table injury. Anterior table fractures occur alone in 33% of cases, with the remaining frontal sinus fractures involving the posterior table alone.1 Given the proximity of the posterior table to intracranial structures of the anterior cranial fossa, intracranial injury occurs in 33% to 70% of patients.6
Anatomy
The independently developing paired frontal sinuses are typically not pneumatized until the age of 2 years. Each approximates the size of a pea around the age of 4 years, and at about the age of 8 years become radiographically identifiable. Significant pneumatization does not occur until the age of 15 years, with maximal expansion not achieved until the age of 19. The paired structures are bound anteriorly by the anterior table, posteriorly by a posterior table, superiorly by the floor of the anterior cranial fossa, inferiorly by the orbital roof, and medially by the intersinus septum.
Identification of the involvement of the frontonasal duct (FND) in injury is essential. This structure is the most anterior and superior portion of the anterior ethmoidal complex. Its chief role is drainage of the frontal sinus into the middle meatus. Borders include the uncinate process anteriorly, the anterior ethmoidal air cells posteriorly, the medial portion of the middle turbinate medially, and the lamina papyracea or suprainfundibular plate laterally.
Arterial supply to the sinus involves contributions from the supraorbital, supratrochlear, and anterior ethmoidal arteries. Venous drainage can be divided into superficial and deep systems. Superficial drainage follows the angular vein, with deep drainage to the subdural venous system through foramina of Breschet. Lymphatic drainage follows meningeal and nasal cavity lymphatics. The complexity of the drainage system points to the risk of meningitis or brain abscess after a frontal sinus fracture, even in the absence of a posterior wall fracture
Diagnosis
Any laceration, hematoma, or ecchymoses of the forehead and glabellar region should heighten suspicion of an associated fracture. Subconjunctival ecchymosis and CSF rhinorrhea may also be present. If CSF leak is suspected, a halo test or laboratory analysis of fluid sampled from the nose for β-2 transferrin can be used to identify CSF. Additionally, the entire region should be palpated for bony irregularities (i.e., depressions, “step-offs,” crepitus), with specific attention given to the superior orbital rims. Anesthesia in the distribution of the supraorbital nerve may be present. Associated swelling may obscure depression in the first few days after injury. Although good clinical examination skills can assist in the diagnosis, physical examination is not enough in determining the extent of injury to the frontal sinus and supplementation of the examination with imaging studies is essential.
Radiographic Analysis
Thin-section axial and coronal CT scans are the main imaging studies used for frontal sinus trauma assessment.5 Complete evaluation involves determination of posterior and anterior wall involvement, fracture displacement, and associated intracranial or FND injury (see Fig. 6). The presence of air-fluid levels in the frontal sinus may imply absence of duct function.1 Pathognomonic CT findings for FND involvement include associated fracture of the anterior ethmoid complex and a fracture of the floor of the frontal
sinus.6 Small fractures are not always readily identifiable radiographically, especially when nondisplaced.
sinus.6 Small fractures are not always readily identifiable radiographically, especially when nondisplaced.
Treatment
Surgical and nonsurgical management options exist. Independent assessment of the anterior and posterior tables and the FND will dictate the need for surgical intervention. Surgical intervention should take place within the first week if possible. Early treatment reduces incidence of long-term complications.5
Indications for surgical intervention include the following: depression of the anterior table, FND involvement on radiographic examination, FND obstruction identified by persistent air-fluid level or mucocele formation, displaced fractures of the posterior table that have presumably lacerated the dura, and CSF leak without resolution after 4 to 7 days. Nondisplaced, simple linear fractures are often managed nonoperatively.
Anterior Wall Fracture
Surgical intervention for anterior wall fracture is determined by the degree of bony displacement and comminution as well as the location of the fracture (e.g., fractures of the supraorbital rim). Nondisplaced anterior wall fractures are managed conservatively, with antibiotics administered for 7 days and follow-up CT scanning over a period of 12 months. Concern for late infection and formation of mucoceles dictates the need for long-term follow-up.
Typically, disruption of aesthetics, secondary to anterior table depression, necessitates surgical repair to restore forehead contour. Adequate exposure of the surgical field is essential for ensuring appropriate bony contouring. A coronal incision will allow for ample exposure down to the nasoglabellar region anteriorly and frontozygomatic junctions laterally.5 Intraoperatively the fractured fragments of the anterior wall are removed, and the sinus cavity is explored for additional damage. In the absence of additional damage (i.e., FND), the bony fragments are carefully reassembled, replaced, and held in place with either titanium screws and plates or resorbable screws and plates. The goal is to restore a proper aesthetic contour of the frontal bone and fronto-orbital bar. Split cranial bone graft may be necessary to restore the anterior wall if there is significant comminution and contamination of the fractured bone.
Posterior Wall Fracture
Isolated posterior wall fractures rarely occur. They are typically accompanied by anterior wall fractures. Should fracture of the posterior wall be nondisplaced, presence of FND damage and/or CSF leakage dictate the need for surgical intervention. Nondisplaced fractures without CSF leak are treated nonoperatively with close observation only. CSF rhinorrhea, if present, can be initially treated expectantly with elevation of the head of the bed to 30 degrees and the patient placed on mandated bed rest. For cases of leakage that extend beyond 4 days, spinal drainage may be considered to expedite resolution.
Significantly displaced posterior wall fractures, comminuted fractures, or nondisplaced fractures associated with persistent CSF rhinorrhea require a surgery. Treatment consists of cranializing the frontal sinus. The procedure involves removal of the entire posterior wall of the frontal sinus followed by repair of dural tears by a neurosurgeon.5 The entire sinus mucosa is stripped and removed by mechanical abrasion using a fine bur. Subsequently, a galeal frontalis flap is placed to separate the intracranial cavity from the FNDs. The anterior table is then repaired and replaced and the frontal lobe expands and fills any remaining dead space.
Frontonasal Duct Fracture
The importance of identifying FND fracture in frontal sinus injury cannot be overemphasized as it is an absolute indication for surgical treatment. Further, because some extent of FND injury accompanies approximately 55% of all frontal sinus fractures, one must be cognizant of both radiographic and intraoperative tactics for FND injury identification. Radiographic findings were discussed previously. If the
fractured segments are not easily observed intraoperatively, methylene blue or fluorescein dyes can be used to assess the drainage of the sinus through the duct into the nasal cavity. Significant FND injury, either isolated or in combination with anterior and/or posterior wall fracture, can be addressed in a variety of ways. A few authors recommend repairing the FND directly followed by stenting the duct open. Stenosis of the duct with potential mucocele formation is a possible long-term risk of this strategy. We recommend obliterating the frontal sinus. Obliteration involves exposing and opening the entire frontal sinus through a coronal approach. This is followed by complete removal of the entire sinus mucosa, closure of the FND with a galeal flap, and bone graft. The remaining dead space in the sinus can then be filled with either bone, fat, muscle, or some advocate leaving air in the sinus. Alloplastic material is not recommended as the rate of infection is significantly increased. If the posterior wall is significantly disrupted then cranialization is favored over obliteration. Long-term follow-up with serial CT scans is essential to rule out mucocele formation.
fractured segments are not easily observed intraoperatively, methylene blue or fluorescein dyes can be used to assess the drainage of the sinus through the duct into the nasal cavity. Significant FND injury, either isolated or in combination with anterior and/or posterior wall fracture, can be addressed in a variety of ways. A few authors recommend repairing the FND directly followed by stenting the duct open. Stenosis of the duct with potential mucocele formation is a possible long-term risk of this strategy. We recommend obliterating the frontal sinus. Obliteration involves exposing and opening the entire frontal sinus through a coronal approach. This is followed by complete removal of the entire sinus mucosa, closure of the FND with a galeal flap, and bone graft. The remaining dead space in the sinus can then be filled with either bone, fat, muscle, or some advocate leaving air in the sinus. Alloplastic material is not recommended as the rate of infection is significantly increased. If the posterior wall is significantly disrupted then cranialization is favored over obliteration. Long-term follow-up with serial CT scans is essential to rule out mucocele formation.
Orbital Fractures
Anatomy
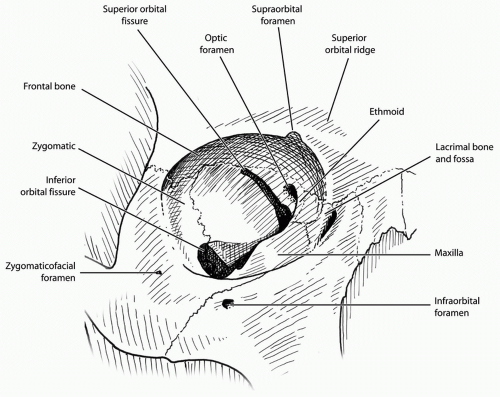
The orbit is made up of the maxilla, zygoma, ethmoid, frontal bone, lacrimal bone, greater and lesser wings of the sphenoid, and palatine bone. The orbital cavity resembles a cone but is thought of as having medial, lateral, superior, and inferior walls for ease of description (see Fig. 7). The superior wall is quite thin but isolated fractures in this area are rare due to the protection from the frontal bone and sinus, and thick supraorbital rim. Children are more predisposed to roof fracture because their cranium is proportionallybigger and the frontal sinus is not pneumatized. The frontal, zygomatic, and greater wing of the sphenoid bones make up the lateral wall. Its strength makes isolated fractures in this wall rare. It is commonly involved in zygomatic fractures. Here the zygoma articulates with the greater wing of the sphenoid.
The inferior wall is relatively weak and susceptible to fracture. Contributing to its weakness is the infraorbital canal, the thin maxillary roof, and the curvature of the floor. The anterior floor is concave and especially weak.
Similarly, the thin lacrimal bone and lamina papyracea of the ethmoid, which make up the medial wall, render it weak. In this area, the lacrimal sac, which is protected anteriorly by the frontal process of the maxilla, can be injured. The medial canthal tendon can also be avulsed or disrupted.
Similarly, the thin lacrimal bone and lamina papyracea of the ethmoid, which make up the medial wall, render it weak. In this area, the lacrimal sac, which is protected anteriorly by the frontal process of the maxilla, can be injured. The medial canthal tendon can also be avulsed or disrupted.
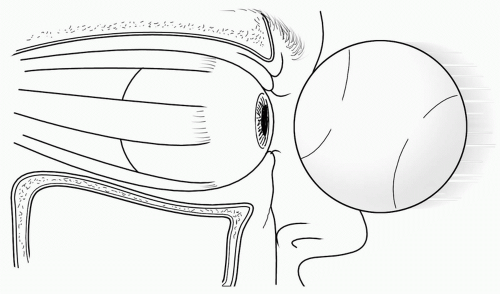
Biomechanics of Injury
Fractures of the floor and medial wall result from one of two mechanisms. One is the direct transmission of force to the orbital rim and the other is through transmission of force from the globe and other orbital contents. There has been much controversy as to which mechanism explains orbital blowout fractures but both likely play a role (see Fig. 8).
Clinical Evaluation
The most common clinical symptoms of blowout fractures are diplopia and enophthalmos. Diplopia is caused by restricted ocular motion. This is most common on upward gaze in blowout fractures. It can manifest on central vision, which is most problematic, or on peripheral gaze. Mechanical causes of diplopia include motion restriction due to entrapment of the intraorbital contents by the fracture, or from changes in the mechanical advantage of the inferior rectus muscle if the vector of pull or excursion changes. Entrapment of the orbital contents such as the inferior oblique or rectus muscles, Lockwood ligament, periorbital fat, or the Tenon capsule can be tested intraoperatively with the forced duction test. This test is performed by gently grasping the sclera with two Adson forceps and rocking the globe from side to side and up and down, being careful not to injure the cornea. Any entrapment becomes evident when the globe fails to move in any one direction. The medial rectus can become contused but rarely incarcerates. Nonmechanical causes of diplopia include extraocular muscle injury, nerve injury to these muscles, edema, or hematomas. The forced duction test is not always accurate in the acute setting, according to Hollier and Thornton.7 Emery et al. observed that in blowout fractures diplopia resolved within 15 days in 55% of patients and persisted in 27%.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree