Complications of Internal Fixation
John V. Vanore
William G. Montross
Fixation of elective osteotomies, arthrodesis, and traumatic fractures are part of daily practice for foot and ankle surgeons. An osteosynthesis is the composite structure of bone and biomaterials transforming an unstable osseous situation into a stable structural framework with reduction of any osseous or articular malalignments (1,2 and 3). It is the responsibility of the surgeon to design an appropriate osteosynthesis, execute the operative plan and monitor for successful bone healing. Complications may and do occur as a result of the insertion and continued presence of these fixation implants (4,5). Some occur due to poor host situations whether due directly to bone quality or pathology that may impair healing (6). Complications may occur due to postoperative overloading of the reconstruction or patient malcompliance. Surgeons must be aware of potential complications and be prepared to treat often difficult clinical situations.
INITIAL PRESENTATION
The patient presenting with a complication from an internal fixation implant will have a history of prior injury or surgery requiring fixation for stabilization of bone. Complications may be asymptomatic for a period of time although generally symptoms of localized pain, deformity, inflammation, or infection, with or without an open wound, may present. The patient may have had a relatively unremarkable postoperative course and is generally followed with serial radiographs to ascertain bone union and maintenance of osseous reduction. Complications occur for a variety of reasons including delayed or nonunion, implant loosening or fracture, chronic pain, soft tissue inflammation, ulceration, or gross infection including osteomyelitis (5,7).
The surgeon’s role is to carefully evaluate the patient and determine what complications have occurred and why they have occurred and provide a treatment plan for the resolution of the complication (Fig. 98.1). Evaluation of the patient must start with a careful history particularly relevant to the past treatment of the affected part including injury, date of surgery, postoperative course, and any known complications. Medical comorbidities such as diabetes, vitamin deficiencies and a variety of patient social habits that may impair healing and lead to fixation complications must be kept in mind (Table 98.1).
Physical examination should identify any gross deformity or instability, prominence of subcutaneous implants, local swelling or inflammation, and areas of tenderness. As this is a musculoskeletal problem, initial evaluation of current radiographs is necessary for evaluation of the current state of bone healing and any deviation in normal osseous anatomy and bone quality. Review of prior radiographs including preoperative films may be very helpful. The diagnostic workup may include blood work with CBC, sedimentation rate, as well as bone scan or MRI for evaluation of nonunion or osteomyelitis, although presence of fixation implants may interfere with imaging studies. Wound culture, in the presence of any ulceration or open wound with identification of any sinus tract formation, may be helpful. Patients presenting with a complication of internal fixation must be evaluated regarding any comorbidities including diabetic control, renal or hepatic impairment, osteopenia, anemia, and nutritional status.
MAKING A DIAGNOSIS
Patients should be evaluated and an accurate diagnosis determined. Definitive diagnosis may require additional surgery including bone culture and bone biopsy, but the surgeon must arrive at an accurate diagnosis to then propose a proper treatment plan (Table 98.2).
The surgeon must clearly assess the clinical situation as well as the likely etiologic factors. Complications are often a very daunting problem as well as the patient’s commitment to the proposed corrective measures, which may include prolonged disability, additional surgery, and administration of costly or potentially toxic drugs. If smoking is the problem, it needs to be addressed or the same complication may occur during the correction.
THE OSTEOSYNTHESIS
Complications associated with an osteosynthesis may occur as a result of a poorly designed fixation construct or inability of the surgeon to execute the planned osteosynthesis. The surgeon must take into account physiologic loading of the bones involved and generally try and limit weight-bearing and potential disruptive forces until bone healing has at least progressed to clinical union (2,50).
When designing an osteosynthesis, there are multiple variations that may be proposed for any clinical situation. The surgeon must take into account bone quality, body habitus, and ability of the patient to limit weight-bearing on the affected part, if necessary. An ideal osteosynthesis is one that provides a stable construct and is able to maintain that position and stability through the bone healing process. Perren’s concept of bone healing (2) under varying conditions of stability is a useful tool to predict and interpret the radiographic appearance of the healing process, so it is instrumental in the surgeon’s assessment of the patient’s progress (Fig. 98.2).
Perren’s Unified Concept of Bone Healing states that bone healing will vary depending upon the degree of stability of the bone interface (2). Under perfectly stable conditions, there will
be no resorption, no bone callus, and no displacement during healing. The radiographic appearance of radiolucency at the fracture or osteotomy and proliferative bone callus is indicative of the degree of mechanical instability. Typically, the clinical parameters of swelling, joint stiffness and localized pain is often proportional to the radiographic findings of instability and secondary union.
be no resorption, no bone callus, and no displacement during healing. The radiographic appearance of radiolucency at the fracture or osteotomy and proliferative bone callus is indicative of the degree of mechanical instability. Typically, the clinical parameters of swelling, joint stiffness and localized pain is often proportional to the radiographic findings of instability and secondary union.
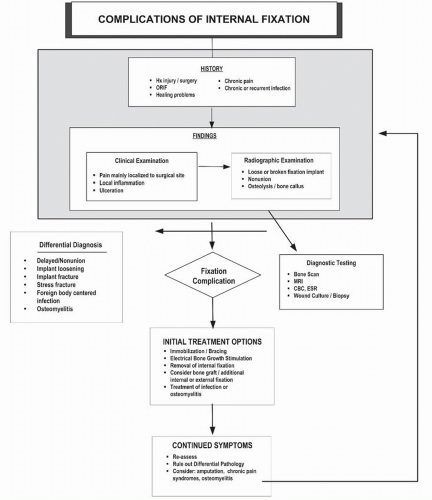 Figure 98.1 Clinical algorithm for the evaluation and treatment of complications associated with the use of fixation implants. |
TABLE 98.1 Disease States and Conditions Associated with Impaired Bone Healing | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








