Nonosseous injuries of the foot and ankle present the surgeon with a significant management challenge because, while not as well publicized as trauma sustained to the skeletal system, soft tissue injuries that involve tissue loss can present with a complex combination of pathologic features that are unique and difficult to manage. These injuries, especially those that involve significant soft tissue defects, can create considerable morbidity and mortality with long-term functional consequences if not treated appropriately.
It is imperative that the surgeon be familiar with the diagnosis and management of injuries that present with significant soft tissue loss to provide the maximum functional outcome to the patient. Advances in surgical and wound healing techniques, such as internal and external fixation, negative pressure wound therapy (NPWT), advanced bioengineered grafts, and microsurgical technique have greatly increased the overall success rate in the treatment of these types of soft tissue injuries and have helped to greatly reduce morbidity associated with soft tissue trauma (
1,
2).
When involved in the management of soft tissue trauma, it is important for the physician to recognize that soft tissue wounds can be differentiated into a number of various subtypes. These subtypes are abrasions, puncture wounds, lacerations, complex wounds, crush injuries, extravasation injuries, bite wounds, and stings. This chapter deals primarily with the evaluation and management of complex soft tissue wounds that involve degloving-type injuries and those injuries with significant soft tissue loss such as avulsion and mutilation injuries to the lower extremity.
COMPLEX SOFT TISSUE WOUNDS
Complex soft tissue wounds are those wounds that present with significant soft tissue loss. As previously described, these complex wounds are a subtype of overall soft tissue wounds, and it is important to recognize that while it is helpful to distinguish between the various subtypes for the purposes of learning, it is also true that these subtypes of wounds can have concomitant presentation. For example, a patient who has sustained a crush injury to the lower extremity may also demonstrate significant soft tissue loss, thus presenting as both a crush injury subtype as well as a complex soft tissue subtype (
3).
There have been a number of attempts to classify soft tissue trauma to provide for rapid differentiation and possible suggestion toward treatment options and overall prognosis. In 1986, Hidalgo and Shaw classified lower extremity soft tissue trauma into three types based on size and extent of the wound (
4) (
Table 97.1):
Type I—Soft tissue loss less than 3 cm2
Type II—Soft tissue loss greater than 3 cm2 with no osseous involvement
Type III—Soft tissue loss greater than 3 cm2 with osseous involvement
Other classification systems have been proposed, which have modified the Hidalgo and Shaw classification system to include location of the wound (i.e., weight-bearing vs. non-weight-bearing areas) and the type of plastic surgery procedure necessary to provide coverage of the defect (i.e., split-thickness skin graft [STSG], local flap, or free myocutaneous flap), but these classification systems do not correlate well to overall prognosis following treatment.
Utilizing depth of injury as a distinction, one can see that complex soft tissue wounds present as either superficial or deep, and this distinction offers some insight into the degree of injury sustained to the extremity and therefore the treatment modalities necessary to manage such injuries. Superficial complex soft tissue injuries are those injuries that can present with epidermal, dermal, and subcutaneous tissue loss. In these cases, the underlying musculoskeletal structures remain intact. In contrast, deep complex soft tissue injuries are those injuries that involve damage to the deep musculoskeletal structures in addition to the superficial skin and subcutaneous structures. These deep complex injuries are the most difficult to reconstruct due to the increased level of damage and tissue loss and often require advanced surgical and wound care techniques to provide definitive closure (
2). When considering the depth and extent of complex soft tissue trauma, it is important to remember the functional anatomy present at the location of injury. Knowledge of this anatomy will allow for appropriate evaluation of the injury and later serve as a guide in preparation for limb reconstruction (
Fig. 97.1).
Most often, complex soft tissue injuries present as degloving, avulsion, or mutilation injuries. The specific mechanisms of complex soft tissue trauma injuries differ largely based on the nature and degree of force applied to the extremity. Often, these injuries are due to a shearing force that is applied across the skin surface, and the degree of force often determines the extent of the subsequent injury. Lower force injuries can yield superficial complex injuries such as simple degloving injuries, while increases in force generate increased disruption to the underlying soft tissue, osseous structures, and neurovasculature (
2).
Degloving injuries refer to those injuries that involve a circumferential elevation of the skin and fat from the underlying musculoskeletal structures. As the skin and subcutaneous tissues are separated from the underlying muscle, damage can occur to the associated perforating blood vessels supplying the overlying layers. In this manner, the degloved tissue may lose its blood
supply and may become devitalized (
Fig. 97.2). Degloving injuries of the foot can result in either partial or complete skin loss, and depending on the degree of force applied and the depth of involvement, concomitant fractures may be present. In the instances of partial skin loss, the degloved skin is often attached distally and disrupted proximally, with the remaining skin flap being rolled or folded down the extremity like a sock or glove, hence the name (
5).
As previously discussed, in degloving injuries the mechanism of injury involves a tangential force to the skin surface (
6). In lower extremity degloving injuries, the most common mechanisms of injury include occupational accidents, bicycle spokes (
Fig. 97.3), and high-velocity motor vehicle accidents (
7,
8).
Soft tissue avulsion injuries are similar to simple degloving injuries except they generally involve more significant soft tissue loss. As with degloving injuries, avulsion injuries occur due to tangentially applied shearing forces that separate the soft tissues from underlying osseous structures, although
generally speaking the forces involved in creating soft tissue avulsion injuries are greater than those creating soft tissue degloving injuries (
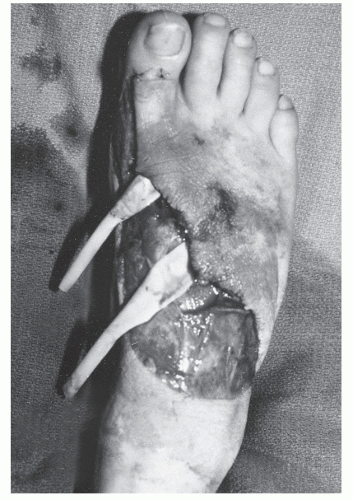
9). Unlike degloving injuries, soft tissue avulsion injuries often demonstrate complete soft tissue loss with no retained soft tissue flap and a subsequent soft tissue defect (
Fig. 97.4). In addition to soft tissue deficits, these injuries can often present with concomitant fractures that must be addressed.
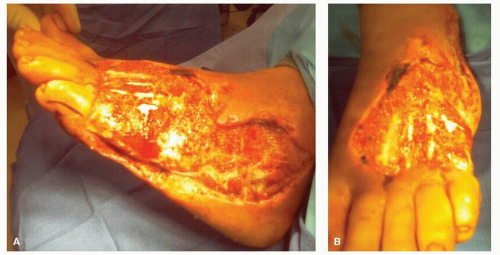
Mutilating injuries to the lower extremity are often described as those injuries that create a “mangled” limb. These injuries are the most severe of complex soft tissue trauma and often lead to amputation due to the significant degree of injury and the reconstructive challenge that they pose (
10,
11). Mutilating soft tissue injuries, particularly those that produce mangled limbs, are often secondary to lawn mower injuries, farm machinery injuries, and high-velocity blast injuries, such as those sustained from land mine blasts or improvised explosive devices (
12,
13). A mangled extremity is one that demonstrates significant injury to skin, bone, nerves, or vasculature (
Fig. 97.5), and the Mangled Extremity Severity Score (MESS) was developed to assess the risk for amputation (
11,
14) (
Table 97.2). A patient’s MESS is calculated as the sum of four parameters: degree of skeletal/soft tissue injury, degree of ischemia, degree of shock, and the patient’s age at the time of injury. A patient with a score greater than 7 demonstrates significant risk of amputation (
14). It is important to understand the severity of and risks associated with mangled extremity injuries; massively crushed muscle and ischemic tissue release myoglobin and other cytotoxic elements, which can lead to renal failure and even death (
11).
EVALUATION
Injuries involving significant soft tissue loss most commonly present to the emergency room, and it is in this setting that the physician is likely to initially become involved in the
management of these patients as a member of a larger health care team. A multidisciplinary team approach allows for expeditious evaluation and treatment of the acute trauma patient in the hospital setting and allows the various surgical and medical specialties the opportunity to provide insight into the appropriate patient management.
It is important to realize that patients suffering from significant soft tissue loss injures may have associated severe lifethreatening injuries, and the initial evaluation of these patients must begin with an assessment of the ABCs (
Airway,
Breathing, and
Circulation) as part of an appropriate primary survey. Management of life-threatening injuries must be addressed first; only after more urgent problems have been addressed can attention be directed toward the management of soft tissue injuries (
15).
As part of the initial evaluation of significant soft tissue injuries, it is prudent to begin by obtaining a thorough event history including, but not limited to, questions regarding the mechanism of action of the injury, the age of the injury, previous attempts at treatments, and any clothing or shoe gear worn during injury. It is also important to obtain a current medical history for the patient including any previous medical conditions, current medications, a social history including tobacco or drug use, any known drug allergies, and the patient’s tetanus immunization status (
16).
After obtaining a thorough history, it is important that one assess the local wound environment at the site of tissue loss to determine the extent and complexity of the injury as well as to evaluate for the presence or absence of contamination by microorganisms or foreign debris. At this point, the wound is carefully examined, with specific attention paid to location and size of the soft tissue defect, the presence of bleeding, and tissue viability. X-rays should be obtained to evaluate for the presence of concomitant osseous injury, and a thorough motor and sensory neurologic exam should be performed to evaluate for neurologic deficits in the affected extremity.
It is often necessary to provide initial local anesthesia to the affected extremity to allow for appropriate evaluation and treatment of the wound (
3). In these cases, local anesthetic can be injected into the periwound tissue or more proximally in the extremity to obtain anesthesia at the wound site. It is important, however, to recognize that direct wound injection may yield less reliable anesthesia due to decreased local anesthesia efficacy in inflamed or infected tissues. Regional nerve blocks directed toward specific sensory nerves may be employed as well to allow for thorough examination of the injured limb.
Injuries that involve soft tissue loss often present with concomitant neurovascular impairment, and it is important that the physician evaluate and address such injuries if they are present (
3). Establishing vascular status is of supreme importance because the ability to reconstruct a limb and provide adequate soft tissue coverage following soft tissue loss injury will largely depend upon establishment of patent vascular supply to the distal segments of that limb. Loss of distal vasculature will ultimately require more proximal intervention for healing and may require possible amputation. This is a significant consequence considering that several studies have demonstrated that patients have increased energy requirements and expenditure as the level of amputation increases proximally (
17,
18).
After appropriately confirming neurovascular status, it is important to assess the level of microorganism and foreign body contamination in the wound. Due to the traumatic circumstances associated with these wounds, they are often contaminated with bits of debris including portions of shoe gear, road debris, or soil contaminants. These contaminants must be removed to reduce the risk of infection and allow the wound to progress through normal healing. Loose foreign bodies can often be removed via lavage in either the treatment or operating room setting; more firmly embedded foreign bodies may require sharp surgical débridement, which can either be accomplished in the treatment or operating room.
As mentioned previously, it is important to establish the patient’s tetanus immunization history. Tetanus is a nervous system disorder that is caused by
Clostridium tetani and is characterized by extreme muscle spasm. Previously, wounds were classified as tetanus-prone or non-tetanus-prone; however, more recent research has demonstrated that tetanus can be associated with a wide variety of injury types, and therefore, all traumatic wounds must be considered tetanus-prone and tetanus prophylaxis indicated as appropriate (
16,
19). Following complex soft tissue injury, patients who have been actively immunized within the past 10 years are administered 0.5 mL tetanus-diphtheria toxoid or adsorbed tetanus toxoid; the latter is given if a suspected hypersensitivity to diphtheria toxoid exists. Patients with a questionable immunization history presenting with significant soft tissue loss wounds are given 0.5 mL diphtheria toxoid and 250 to 500 U of tetanus immunoglobulin intramuscularly (
16).
As part of the initial evaluation of patients with soft tissue trauma, it is also important to evaluate the need for antibiotic
therapy. Clean wounds and clean-contaminated wounds generally are adequately treated with irrigation, débridement, and local wound care. However, in instances with significant tissue loss, especially in patients with underlying systemic factors (such as diabetes or impaired circulation) that increase risk of wound infection, prophylactic antibiotic therapy should be initiated. Certainly, contaminated wounds are associated with increased risk of infection, and patients with these dirty wounds should also be placed on prophylactic antibiotic therapy. Studies have demonstrated that significant soft tissue wounds are commonly contaminated by a mix of both grampositive organisms and gram-negative organisms, and therefore broad-spectrum antibiotics are indicated (
20). Often, these antibiotics include combinations of β-lactam antibiotic with a β-lactamase inhibitor.






 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access