Abstract
Following severe traumatic brain injury (TBI), failure to adjust language to communication abilities has been described and attributed by many authors to executive function impairment. Interactional dysfunctions may damage family-based, social and vocational equilibrium, and they are of key importance in prognosis of rehabilitation outcome. In conversation, frequently occurring inappropriate formulations connote difficulties in discursive organization and are likely to include numerous digressions, if not confabulations.
Objective
The main objective of this study was to improve assessment of the non-verbal as well as the verbal aspects of the communication disorders observed in TBI subjects. We have developed and are proposing the grid for linguistic analysis (GALI) of free conversational interchange that constitutes an original French-language tool. We wish to demonstrate its validity as a means of measuring interactive skills in a given population.
Method
We assessed 17 severely brain injured patients presenting executive dysfunction, who were compared with 34 matched and healthy individuals. Fifty-one 10-minute sequences of free conversation between study participants and therapists were filmed and analyzed by applying the GALI. Three independent raters coded the conversations. Inter-rater reproducibility was considered statistically satisfactory.
Results
The results successfully distinguished TBI patients from healthy subjects and thereby underscored the discriminatory value of the tool. A significant correlation was found between the patients’ performances in executive tests and in the GALI.
Conclusions
In severe TBI a social handicap results from several associated cognitive disorders. Interactive discourse analysis combining non-verbal with verbal aspects confirms the existence of difficulties in communication that are usually underestimated in classic formal language testing methods. The GALI is likely to meet speech therapists’ need for reliable assessment of their patients’ interactional difficulties and their consequences in social life.
Résumé
Objectifs
Suite à un traumatisme crânien grave, d’importantes perturbations de l’utilisation du langage en contexte sont observées et attribuées par de nombreux auteurs au déficit exécutif. Ces dysfonctionnements interactionnels bouleversent de façon durable l’équilibre social et professionnel et tiennent une part importante dans le pronostic de réinsertion. L’objectif général de cette étude est l’amélioration de l’évaluation des troubles de la communication par l’élaboration d’un outil standardisé, en considérant un aspect systématiquement négligé qui est celui du domaine de la communication non verbale.
Méthode
Notre étude a porté sur la réalisation puis la validation d’une grille d’analyse linguistique d’interaction libre (GALI) auprès d’un corpus de 17 sujets traumatisés crâniens graves comparés à 34 sujets témoins appariés.
Résultats
Les résultats de cette étude ont permis de valider partiellement cette grille et notamment de vérifier ses qualités discriminantes. Cet outil d’évaluation a mis en évidence la présence constante, à des degrés variables, de déficits communicationnels verbaux et non verbaux. Par ailleurs, une corrélation significative a été retrouvée entre les performances des sujets aux tests exécutifs et à la GALI.
Conclusion
Chez les traumatisés crâniens graves, le handicap social est la résultante de désordres cognitifs intriqués. À ce titre, l’analyse du discours conversationnel dans ses composantes verbales et non verbales confirme les difficultés de communication sous estimées ou négligées par les tests de langage classiques qui n’ont pas été conçus dans un objectif d’analyse fonctionnelle de la communication. La GALI a été élaborée afin de répondre à un besoin orthophonique d’évaluation de ces perturbations conversationnelles et de leurs retentissements.
1
English version
1.1
Introduction and objectives
The cognitive, psycho-emotional and behavioral difficulties encountered by persons with severe traumatic brain injury (TBI) impose a heavy family, social and professional burden. One of the key obstacles to their rehabilitation consists in the disruption of their use of language in a specific context. This type of disorder, which is not aphasic in the literal sense of the word, has up until now essentially been studied through discourse analysis in terms of impaired verbal abilities, and it has frequently been linked to executive dysfunction . These different and numerous studies have depicted discourses as largely irrelevant, uninformative, meandering, fragmented, incoherent or repetitive . In conversations, the frequent appearance of inappropriate formulations has been associated with disordered discourse construction along with multiple digressions and occasional confabulations. While the verbal aspects have been described in several studies, with a few rare exceptions the non-verbal aspects have been ignored, even though they are part and parcel of communication; we would be hard-put to deny that “…gestures are an integral part of language as much as are words, phrases and sentences. Gestures and language are one system” . A conversational situation differs from traditional language-based investigations in its degree of complexity and on account of the multiple mechanisms it involves into play, of which improvisation is but one example. It also involves emotional and motivational elements that tend to be neglected in classical evaluations. Per se , conversation requires simultaneous verbal and non-verbal processing of a wide array of linguistic, pragmatic, cognitive and social data, many of which are subject to possibly subtle dysfunction in a TBI patient. So it is that conversation analysis is called upon to highlight practical communication problems that tend to elude investigations focusing on the formal linguistic aspects of language , problems that are summarized by an adage: “The brain-injured person is better at speaking than at communicating”.
The main objective of this study is to propose a French-language tool providing detailed evaluation of the communication disorders suffered by TBI patients presenting dysexecutive syndrome; not only verbal, but also non-verbal aspects, which have been omitted from consideration for too long, and will now be taken into account.
In 1984, Cosnier and Brossard demonstrated that non-verbal communication (NVC) is hardly synonymous with non-language based communication, while language-based communication is by no means limited to a verbal system. Concretely speaking, conversational posture, eye contact (the gaze), intonation and facio-gestural communication are dynamically associated with verbal skills as constitutive elements of the énoncé total , or overall formulation. The structure of the grille d’analyse d’interaction libre (GALI) or grid for analysis of free conversational interchange is based on the levels of conversation defined by Cosnier , namely what is formulated, the formulation itself and the pragmatic interactional level. What is formulated ( l’énoncé ) pertains to the form of a discourse, which means not only the vocal or acoustic ingredients (intonation, intensity, rhythm…), but also the quality of discursive syntax. At the non-verbal level, it refers to the different gestures (coverbal, facial…) directly related to the verbal contents. As for enunciation itself ( l’énonciation ), it corresponds to an individual act of elaborating and producing an énoncé , which – most importantly – is addressed to a conversation partner. At this level, the substance of a discourse (structuring, authenticity, related facial and postural gestures…) undergoes analysis. Concerning other aspects than words, the gaze underscores discourse planning, , while coverbal or language-like gestures unconsciously facilitate the wording of pre-verbal thought and lexical search . Finally, the pragmatic interactional level pertains to discourse in direct connection with a fellow interlocutor: the way speakers take turns speaking, the functions of common or shared speech and of maintaining or “copiloting” non-verbal as well as verbal interchange, and so on.
This work represents a continuation of our 2007 study , which has been reproduced with regard to 17 other TBI patients .
We first present the GALI of which the purpose is quantitative and qualitative analysis of the pragmatic and linguistic functions required for satisfactory conversation. This tool has been elaborated so as to elucidate the types of impaired conversational behavior described in the literature. Our practical objective is to enhance diagnostic evaluation and therapeutic management of speech disorders. Later in the paper, patient results shall be analyzed and further discussed.
1.2
Methodology
1.2.1
Population
We have evaluated 17 patients (P) suffering from severe traumatic brain injury (TBI), who were recruited in the French department of Calvados in the neurological rehabilitation center of the Aunay sur Odon hospital and the UEROS of Mondeville and whose clinical characteristics are summarized in Table 1 .
| Patient | Sex | Age | Lat. | NYS | IG | AD | MMA | Brain lesions |
|---|---|---|---|---|---|---|---|---|
| P1 | M | 20 | R | 11 | 7 | 60 | 6 | Initial scan (D0): bilateral frontal hematoma with diffuse edema and petechiae |
| P2 | M | 17 | R | 11 | 7 | 60 | 7 | Initial scan (D0): intracerebral left parietal hematoma with major mass effect on the cerebral faix and temporal petechial hemorrhages |
| P3 | M | 31 | R | 15 | 6 | 0 | 8 | Initial scan (D0): displaced frontal compound depressed skull fracture extending into the right occipital, acute small-size, bilateral frontal parenchymatous hematoma on fractured skull, right occipito-parietal EDH, cerebral edema with major mass effect |
| P4 | F | 28 | R | 12 | 5 | 42 | 6 | Initial scan (D0): right frontal basal hematoma, deep bilateral parietal petechiae at the level of the left central basal ganglia, minimal subarachnoid hemorrhage and minor SDH of the left cerebellar tentorium |
| P5 | H | 59 | R | 11 | 5 | 0 | 4 | Initial scan (D0): right temporo-parietal contusion with mass effect and onset of displacement of a cerebral hemisphere under the cerebral faix, major right parietal skull fracture with bone splinter from the right longitudinal sinus |
| P6 | M | 22 | L | 11 | 7 | 42 | 4 | Initial scan (D0): bi-fronto-parietal meningeal hemorrhage with right frontal hemorrhagic contusion, acute fronto-parietal SDH and right parietal fracture |
| P7 | M | 16 | R | 9 | 7 | 0 | 3 | Initial scan (D0): left temporo-parietal EDH, left fronto-parietal fracture without bone splinter penetration, and bifrontal cerebral contusion |
| P8 | M | 24 | R | 12 | 7 | 42 | 4 | Initial scan (D0): left frontal hemorrhagic contusion and subarachnoid hemorrhage |
| P9 | F | 22 | L | 14 | 7 | 79 | 8 | Initial scan (D0): right and centrally located oval-shaped petechiae without edema MRI (day 8): insular parenchymatous hemorrhagic insular and right frontal lesions as well as lesions of the corpus callosum splenium and a bilateral temporal edematous reaction |
| P10 | M | 36 | R | 11 | 5 | 63 | 7 | Initial scan (D0): right temporal and left frontal contusions and left parietal petechiae |
| P11 | M | 21 | L | 11 | 5 | 60 | 5 | Initial scan (D0): right SDH, bifrontal contusions, lesions of the corpus callosum of the thalamic region MRI: diffuse hemosideric deposits at the frontal bilateral and deep perimesencephalic levels; petechiae detected at the level of the left cerebellum. Fluid collection aspects in T2 hypersignal at the fronto-parietal level |
| P12 | F | 22 | R | 12 | 7 | 42 | 8 | Initial scan (D0): SDH, right parietal petechiae and moderate cerebral edema MRI (D4): right and bifrontal sylvian shearing lesion; bilateral frontal hygroma |
| P13 | M | 24 | R | 11 | 4 | 70 | 7 | Scan (7 months): no intra or extra-axial hemorrhage, sequelar hypodensity at the right frontal cortico-subcortical junction, no hydrocephalus, no mass effect or cerebral edema, no abnormality of the posterior fossa or the brain stem |
| P14 | F | 29 | R | 11 | 7 | 70 | 15 | Initial scan (D0): superficial bifrontal contusion and left frontal petechiae |
| P15 | M | 42 | R | 11 | 7 | 40 | 36 | Initial scan (D0): right frontal contusion |
| P16 | F | 28 | R | 9 | 7 | 42 | 42 | Initial scan (D0): right frontal contusion |
| P17 | M | 42 | R | 15 | 3 | 35 | 38 | Initial scan (D0): basal ganglia hematoma on the right Control scan (D30): bilateral frontal hydroma predominant on the right, without indication of surgical evacuation |
Inclusion criteria were as follows: the brain injury had to have occurred more than three months previously and the patients underwent examination after the post-traumatic amnesia (PTA) phase evaluated by the « Galveston Orientation Amnesia Test » (GOAT Levin et al., 1979). End of the PTA phase occurred when two successive scores were equal to or greater than 75/100. The subjects had to be French-speaking and of French culture. They also had to present with dysexecutive syndrome, which was assessed through a protocol involving several neuropsychological tests: Tower of London, Stroop, the Wisconsin Card Sorting Test (in the form modified by Nelson), the Trail Making Test, the WAIS-R “cube construction” and “picture arrangement” tests, and the Six Elements test. The subjects’ z scores are presented in Table 2 .
| Patients | Tower of London -5N 5 movements Positive trigger | Tower of London -5I- 5 movements Negative trigger | WAIS cubes | WAIS picture arrangements | Wisconsin Premature withdrawals | Stroop word color | Trail Making Test -B | 6-element tests |
|---|---|---|---|---|---|---|---|---|
| P1 | −0.98 | 0.72 | −0.67 | −1.00 | 0.83 | −1.60 | −1,44 | −1.76 |
| P2 | −0.57 | 0.72 | −0.67 | −1.33 | 0.75 | −0.60 | −1.55 | −1.29 |
| P3 | −0.98 | −1.01 | −2.33 | 0.33 | 0.80 | −2.10 | −1.30 | −6.99 |
| P4 | −0.98 | −1.01 | −1.00 | −0.67 | 0.73 | −2.20 | −1.42 | −2.85 |
| P5 | −0.57 | 0.72 | −1.67 | −1.00 | 0.69 | −1.40 | −3.87 | −3.96 |
| P6 | −2.22 | −0.40 | 0.33 | −3.00 | −1.67 | 0.20 | −5.44 | −3.02 |
| P7 | 1.26 | −0.40 | −1.33 | −1.00 | −0.92 | 0.00 | −11.27 | −1.49 |
| P8 | 0.64 | −0.26 | −1.00 | −1.00 | 0.73 | −1.50 | −3.30 | 0.48 |
| P9 | −0.56 | −1.01 | −2.00 | 0.00 | 0.73 | 0.00 | −0.06 | −0.48 |
| P10 | 1.91 | 0.40 | 0.33 | −1.67 | −3.33 | −2.50 | −2.03 | −3.03 |
| P11 | 0.88 | −0.07 | −1.67 | −2.67 | −1.67 | −0.20 | −3.40 | −2.47 |
| P12 | −0.98 | −0.86 | −0.33 | 0.00 | −2.00 | −1.20 | −0.83 | −1.34 |
| P13 | 1.91 | −1.01 | −3.00 | −1.00 | −2.50 | −2.30 | −12.20 | −2.02 |
| P14 | −0.98 | 0.40 | −2.33 | −1.67 | 0.83 | 0.10 | −0.23 | −3.82 |
| P15 | −1.29 | −1.34 | −1.33 | 0.67 | 0.69 | −2.00 | −0.11 | −3.60 |
| P16 | −1.71 | −1.82 | −1.00 | −1.67 | 0.83 | −1.90 | −3.24 | 0.43 |
| P17 | −1.60 | −1.48 | −1.67 | −1.67 | 0.71 | 0.10 | 0.35 | −1.32 |
Exclusion criteria were as follows: a pronouncedly decreased intellectual ability as measured by the WAIS-R (overall IQ lower than 80), presence of aphasia disorders (BDAE), or of dysarthria (BECD), existence of sensory or motor impairment, gestural apraxia, neurological or psychiatric past history, bilingualism.
Each subject was paired with two controls according to age, sex and sociocultural level.
1.2.2
Material
We developed a corpus of 51 sequences consisting in 10 minutes of free conversation between study participants (17 patients and 34 controls) and a member of the clinical staff designated as the “contact person” (CP). The sequences were filmed and then analyzed with the screening tool we have drawn up, which is known in French as the GALI.
The GALI is an exhaustive French-language tool of which the purpose is to analyze the verbal and non-verbal conversational abilities of a TBI subject presenting dysexecutive syndrome and of his or her interlocutors (cf. Appendix 1, short version ).
The structure of the GALI has been drawn up from the different levels of conversation defined Cosnier : what is formulated (26 items), formulation itself (25 items) and the pragmatic interactional level (69 items). The last part, which is not considered in the present study, pertains to the contact person, who can be an informal or an official caregiver, and to any adjustments he or she may bring about (27 optional items). All in all, the GALI we have applied is composed of 120 items.
Each item is graded on a scale ranging from 0 to 5 (0: « no impairment », 1: « very mild impairment», 2: « mild impairment», 3: « moderate impairment », 4: « severe impairment » and 5: « very severe impairment »).
Each conversational level corresponds to a synthesis scale (SS) summarizing the degrees of difficulty. SS1 corresponds to the synthesis scale involving “what is formulated”, SS2 to the synthesis concerning “formulation itself” and SS3 to the “pragmatic interactional level”. A synthesis scale score corresponds to the maximum grade given to a patient on the level described, provided that at least three items reach that grade for SS1 and SS2, and at least 10 items for SS3. This grading system was adopted in account of the very large number of items that each part comprises, and also in order to highlight the difficulties observed; a single item can correspond to a source of significant everyday disturbance.
An overall score (OS) is calculated by adding up the three synthesis scale scores.
1.2.3
Procedure
The participants – patients and controls alike – were asked to freely converse with the contact person (CP). As they were already acquainted with their conversation partners, they were not exposed to the anxiety-inducing situations provoked by an unknown interlocutor. They had been told about the presence of a camera and had agreed to be filmed without having been informed on the contents of the corpus analysis that would be carried out. The person (patient or control) was filmed facing the camera, and thanks to an interplay of mirrors, the CP was comparably visible. The distance between two speakers was set at 1.10 m. Conversational interchange was open, and it lasted for half an hour; corpus analysis involved the last ten minutes. CPs made a point of bringing personal considerations into the discussion so as to render it as “natural” as possible, thereby avoiding to the greatest possible extent an interviewer/interviewee confrontation.
1.2.4
Coding
Three independent raters coded the entirety of the conversations involving the 17 patients and the 34 controls using the GALI grid. The degree of inter-rater agreement for each item was calculated with Kendall’s W coefficient. For all of the items, W > 0.75; P < .001, which indicates very good inter-rater agreement. The coefficient of agreement for the overall grid score (GS) was W > 0,99; P < .001. Inter-rater reproducibility was consequently deemed satisfactory. Given the degree of agreement between the different raters, only the scores given by the 3rd rater were taken into consideration in our presentation of the results.
1.3
Results
1.3.1
GALI validation
The initial objective of this work was to provide arguments supporting the validity of the GALI as an instrument measuring conversational skills and corresponding as closely as possible to the criteria defined by Fermanian. We also wished to underline the interest of our rating scales in physical medicine and rehabilitation .
1.3.1.1
Predictive validity
A tool has good predictive validity when the result it yields is congruent with independent and direct measurement of the characteristic the test has been designed to assess. In this case, the criteria applied was the clinical diagnosis given by a speech therapy specialist. The GALI has good predictive validity if it accurately differentiates unhealthy from healthy participants. The overall scores of the patients (median: 10) and the controls (median: 1) in the GALI ( Table 3 ) have been statistically compared with a Mann-Whitney test. In the final analysis, the overall score for the patient was significantly more elevated than the overall score for the controls: U = 595, P < .001. The grid indeed discriminates between the two different populations and thereby fulfills the external criteria applied. Item-by-item analysis demonstrates that the patients’ scores were significantly higher than the controls’ scores for all items included in the grid with the exception of eight: 1.7, 1.9, 1.15, 2.9, 3.14, 3.53, 3.66 and 3.69 (cf. Appendix 1 ), for which the difference did not reach significance. It consequently appears that the GALI satisfactorily makes the distinction, as would a clinician, between recovering patients and healthy controls.
| SS1/ What is formulated (raw score) | SS2/ Formulation itself (raw score) | SS3/ Pragmatic interactional (raw score) | Total score (raw score) GS | |
|---|---|---|---|---|
| Patients | ||||
| P1 | 3 | 3 | 4 | 10 |
| P2 | 3 | 3 | 3 | 9 |
| P3 | 3 | 3 | 4 | 10 |
| P4 | 2 | 2 | 3 | 7 |
| P5 | 3 | 3 | 4 | 10 |
| P6 | 3 | 3 | 5 | 11 |
| P7 | 4 | 3 | 4 | 11 |
| P8 | 1 | 1 | 3 | 5 |
| P9 | 1 | 3 | 2 | 6 |
| P10 | 2 | 3 | 4 | 9 |
| P11 | 3 | 3 | 3 | 9 |
| P12 | 3 | 3 | 4 | 10 |
| P13 | 4 | 4 | 5 | 13 |
| P14 | 3 | 3 | 4 | 10 |
| P15 | 4 | 3 | 4 | 11 |
| P16 | 3 | 3 | 4 | 10 |
| P17 | 4 | 4 | 5 | 13 |
| Distribution raw scores | 3 | 3 | 3 | 8 |
| Median raw scores | 3 | 3 | 4 | 10 |
| Min raw scores | 1 | 1 | 2 | 5 |
| Max raw scores | 4 | 4 | 5 | 13 |
| Controls | ||||
| Distribution raw scores | 1 | 1 | 2 | 3 |
| Median raw scores | 0 | 0 | 1 | 1 |
| Standard deviation raw scores | 0.50 | 0.46 | 0.60 | 1.04 |
| Min raw scores | 0 | 0 | 0 | 0 |
| Max raw scores | 1 | 1 | 2 | 3 |
1.3.1.2
Construct validity
Construct validity is aimed at establishing the degree to which the grid provides adequate measurement of the theoretical construct to be evaluated. In this instance, the GALI has been conceived so as to measure conversational difficulties according to three distinct levels: what is formulated, formulation itself and the pragmatic interactional level. In order to specifically indicate the construct measured by the GALI and to confirm the validity of its breakdown into three distinct areas, a principal components analysis (PCA) was conducted on the different items. Its results show that the 16 components have a value equal to or greater than 1, which means that the GALI effectively takes into account the actual variety of dimensions, and that the overall variance of the items cannot be clustered in a limited number of components. That much said, given the small sample size, the dimensions should be interpreted with caution. For this reason, our analysis in this paper will involve only the first component, which in fact explains 47.09% of the overall variance, while the other components account for relatively negligible proportions.
Examination of the component matrix indicates that the items most strongly contributing to the construction of axis 1 ( Table 4 ) are the following: 3.43, 3.28, 3.31, 3.34, 3.19, 3.48, 3.21, 3.67, 3.46, 3.42, 3.35, 2.1, 1.1, 3.60, 2.2, 2.3, 3.26 et 1.16. The axis can be interpreted as a translation of affective-cognitive and discursive convergence. The PCA is not identical to the initially projected breakdown into three distinct levels.
| Items | FL | Items | CS | Items | FL |
|---|---|---|---|---|---|
| 3.31 | 0.892 | 1.4 | 0.596 | 2.15 | 0.394 |
| 1.16 | 0.779 | 1.5 | 0.588 | 3.4 | 0.368 |
| 3.34 | 0.771 | 1.1 | 0.570 | 3.59 | 0.331 |
| 3.21 | 0.746 | 3.37 | 0.543 | 1.8 | |
| 3.25 | 0.720 | 3.42 | 0.542 | 1.9 | |
| 3.35 | 0.716 | 2.10 | 0.526 | 2.2 | |
| 3.43 | 0.711 | 3.46 | 0.526 | 2.3 | |
| 1.2 | 0.694 | 3.64 | 0.522 | 2.4 | |
| 3.28 | 0.668 | 3.26 | 0.514 | 2.9 | |
| 3.36 | 0.657 | 3.48 | 0.487 | 3.6 | |
| 3.29 | 0.655 | 2.1 | 0.481 | 3.7 | |
| 2.14 | 0.652 | 3.38 | 0.469 | 3.17 | |
| 3.67 | 0.645 | 3.3 | 0.433 | 3.24 | |
| 3.19 | 0.620 | 1.10 | 0.421 | 3.61 | |
| 3.60 | 0.610 | 3.8 | 0.408 | ||
| 1.3 | 0.608 | 1.15 | 0.404 |
1.3.1.3
Convergent validity
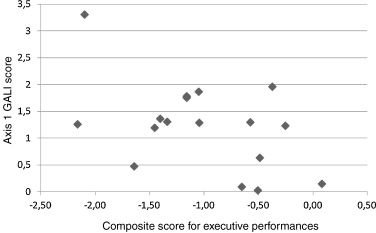
Convergent validity consists in specifying what a tool measures by achieving correlations with tools of which the validity had previously been established. A connection between pronounced conversational difficulties and dysexecutive syndromes has frequently been reported , and that is why a correlation between GALI scores and executive performances is to be expected. A standardized composite score for executive performances has been calculated for each patient by averaging the standard scores for the different tests they have taken ( Table 2 ). Correlation between this composite score and the score for patients on axis 1 of the PCA, the construct underlying the GALI that explains the most common variance, is significant,, r = –0.614, P < .01 ( Fig. 1 ). The lower the average score for the executive functions, the higher the GALI performances (i.e. the more the patient is impaired as regards conversational abilities). Correlation analysis renders it possible to establish a link between axis 1 of the PCA and the executive functions of the patients.
1.3.2
Raw scores
Raw scores for the patients on SS1, SS2, SS3 and the global raw score (GS) with the medians, maximums and minimums compared to the scores for the controls are specified in Table 3 .
1.3.3
Qualitative analysis of the conversational abilities of the 17 TBI subjects
7 patients (P3, P5, P6, P12, P14, P15 and P17) were considered as logorrheic, whereas four patients (P2, P7, P13 and P16), on the contrary, presented with impaired verbal triggering.
Table 5 reports only the GALI items mentioned hereinafter.
| ITM | MIN | MAX | MED | P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 | P12 | P13 | P14 | P15 | P16 | P17 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.2 | 0 | 4 | 3 | 3 | 3 | 0 | 0 | 0 | 3 | 4 | 0 | 0 | 2 | 2 | 0 | 4 | 3 | 3 | 3 | 3 |
| 1.3 | 0 | 4 | 2 | 3 | 2 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 1 | 2 | 0 | 4 | 2 | 2 | 2 | 3 |
| 1.4 | 0 | 4 | 2 | 3 | 3 | 0 | 0 | 0 | 3 | 4 | 0 | 0 | 1 | 3 | 0 | 4 | 3 | 2 | 2 | 2 |
| 1.5 | 0 | 4 | 2 | 3 | 3 | 0 | 0 | 0 | 3 | 4 | 0 | 0 | 1 | 2 | 0 | 3 | 2 | 2 | 2 | 2 |
| 1.8 | 0 | 4 | 2 | 3 | 2 | 1 | 2 | 3 | 1 | 3 | 1 | 0 | 3 | 4 | 1 | 3 | 2 | 0 | 3 | 4 |
| 1.10 | 0 | 4 | 2 | 3 | 2 | 0 | 2 | 0 | 0 | 4 | 0 | 0 | 2 | 1 | 3 | 4 | 0 | 3 | 3 | 0 |
| 1.15 | 0 | 4 | 0 | 0 | 0 | 2 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 4 | 0 | 0 | 0 | 0 |
| 1.16 | 0 | 3 | 2 | 2 | 0 | 2 | 0 | 0 | 3 | 3 | 0 | 0 | 2 | 0 | 0 | 3 | 3 | 3 | 2 | 2 |
| 2.2 | 1 | 3 | 2 | 2 | 1 | 3 | 2 | 3 | 2 | 2 | 2 | 2 | 2 | 3 | 2 | 2 | 2 | 2 | 3 | 2 |
| 2.3 | 1 | 3 | 2 | 1 | 1 | 3 | 2 | 3 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 3 | 2 | 3 | 3 |
| 2.4 | 0 | 3 | 0 | 0 | 0 | 3 | 0 | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 1 | 0 | 2 |
| 2.9 | 0 | 3 | 0 | 3 | 0 | 2 | 0 | 0 | 0 | 1 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2.10 | 0 | 5 | 2 | 0 | 2 | 0 | 0 | 3 | 4 | 2 | 2 | 2 | 0 | 0 | 3 | 4 | 3 | 3 | 0 | 5 |
| 2.14 | 0 | 4 | 2 | 3 | 1 | 1 | 0 | 3 | 3 | 2 | 0 | 1 | 0 | 3 | 2 | 4 | 2 | 3 | 0 | 2 |
| 2.15 | 0 | 4 | 2 | 2 | 3 | 0 | 2 | 0 | 3 | 4 | 0 | 3 | 2 | 0 | 0 | 4 | 1 | 3 | 3 | 0 |
| 3.3 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 1 | 1 | 0 | 0 | 3 | 3 | 3 | 4 | 0 |
| 3.4 | 0 | 4 | 1 | 4 | 1 | 0 | 3 | 0 | 0 | 3 | 1 | 1 | 2 | 0 | 0 | 4 | 2 | 3 | 4 | 0 |
| 3.6 | 0 | 5 | 0 | 2 | 0 | 5 | 0 | 4 | 3 | 0 | 0 | 1 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 3 |
| 3.7 | 0 | 3 | 2 | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 1 | 2 | 1 | 3 | 2 | 2 | 2 | 2 | 3 | 2 |
| 3.8 | 0 | 5 | 4 | 5 | 2 | 5 | 5 | 4 | 4 | 5 | 0 | 4 | 4 | 0 | 4 | 4 | 5 | 3 | 5 | 5 |
| 3.17 | 0 | 5 | 3 | 4 | 2 | 4 | 3 | 4 | 4 | 0 | 0 | 3 | 3 | 1 | 5 | 2 | 3 | 3 | 4 | 4 |
| 3.19 | 0 | 5 | 4 | 3 | 2 | 5 | 4 | 4 | 5 | 3 | 0 | 2 | 3 | 0 | 5 | 5 | 4 | 4 | 4 | 4 |
| 3.23 | 0 | 4 | 3 | 3 | 2 | 0 | 3 | 4 | 4 | 3 | 0 | 0 | 0 | 2 | 4 | 3 | 3 | 1 | 4 | 4 |
| 3.24 | 0 | 5 | 3 | 1 | 1 | 5 | 3 | 4 | 4 | 0 | 0 | 2 | 2 | 2 | 5 | 3 | 3 | 3 | 4 | 4 |
| 3.25 | 0 | 4 | 1 | 2 | 0 | 0 | 0 | 1 | 4 | 1 | 1 | 0 | 3 | 0 | 0 | 3 | 1 | 2 | 0 | 2 |
| 3.28 | 0 | 4 | 3 | 2 | 1 | 3 | 0 | 4 | 3 | 1 | 2 | 0 | 4 | 0 | 3 | 4 | 3 | 3 | 3 | 3 |
| 3.29 | 0 | 4 | 0 | 2 | 0 | 0 | 0 | 0 | 4 | 3 | 1 | 0 | 3 | 0 | 0 | 4 | 2 | 1 | 0 | 0 |
| 3.31 | 0 | 4 | 2 | 3 | 0 | 2 | 0 | 2 | 3 | 3 | 0 | 0 | 1 | 0 | 2 | 4 | 3 | 2 | 2 | 3 |
| 3.34 | 0 | 4 | 2 | 3 | 2 | 2 | 2 | 1 | 4 | 3 | 1 | 0 | 2 | 2 | 1 | 4 | 3 | 3 | 3 | 3 |
| 3.36 | 0 | 4 | 1 | 3 | 1 | 0 | 0 | 1 | 2 | 1 | 0 | 0 | 3 | 3 | 1 | 4 | 0 | 3 | 0 | 3 |
| 3.37 | 0 | 5 | 3 | 4 | 3 | 3 | 3 | 1 | 4 | 4 | 0 | 4 | 2 | 1 | 3 | 4 | 3 | 3 | 3 | 5 |
| 3.38 | 0 | 5 | 3 | 2 | 1 | 4 | 0 | 4 | 3 | 0 | 3 | 0 | 3 | 0 | 4 | 5 | 2 | 3 | 3 | 0 |
| 3.43 | 0 | 4 | 3 | 3 | 1 | 4 | 1 | 4 | 3 | 3 | 2 | 0 | 3 | 1 | 3 | 4 | 3 | 3 | 3 | 3 |
| 3.59 | 0 | 3 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 3 | 0 | 0 | 2 | 0 | 3 | 0 | 3 | 0 | 3 |
| 3.61 | 0 | 3 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 3 | 1 | 0 | 0 | 0 | 3 |
| 3.64 | 0 | 5 | 3 | 4 | 1 | 0 | 0 | 3 | 1 | 0 | 0 | 3 | 1 | 3 | 0 | 5 | 5 | 5 | 4 | 5 |
| 3.67 | 0 | 5 | 2 | 2 | 0 | 2 | 0 | 3 | 3 | 0 | 2 | 2 | 2 | 2 | 1 | 5 | 3 | 3 | 3 | 3 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






