7 Common Procedures This chapter covers procedures that are commonly needed in the daily care of children but are not well described in surgical atlases, including techniques for the application of traction in children, administration of regional blocks, and aspiration of major joints. Skin traction is used for conditions that require moderate traction for reduction or comfort. It is limited by the shear resistance of skin, which is about 2 to 4 pounds per limb in younger children and 5 to 7 pounds per limb in older children. If these parameters are exceeded, blisters may form. Skin is also more sensitive when it has been traumatized or when there is swelling from an adjacent fracture. Skeletal traction is an option if skin traction is not suitable. Some indications for skin traction include the following: 1. Treatment of developmental dysplasia of the hip up to about age 2 to 3 years 2. Restoring abduction in stiff, adducted hips with Perthes disease 3. Femur fractures under age 6 a. As definitive treatment if a cast is contraindicated and there is no spasticity b. As temporary treatment until definitive stabilization is performed 4. To promote resolution of transient synovitis 1. Apply tincture of benzoin (if desired) followed by a single layer of soft roll. Do not apply the traction strips directly to skin. Application of more than a single layer of soft roll would allow traction to slip off when weight is applied. 2. Place an adhesive strip in a sugar-tong or “U” shape on the limb as shown in Fig. 7.1. Be sure to pad the malleoli well. If the traction weight is to approach the limit stated above, distribute the shear over the maximum area by bringing the wrap up to the thigh. 3. Roll Ace wrap around leg to hold traction strip in place. Do not roll too tightly. 4. Place spreader in loop of adhesive strip. Make sure the malleoli are free. Fig. 7.1 Application of skin traction to lower limb. 1. Collect equipment including Steinmann pin set, hand drill, sterile gloves and towels, Lidocaine, and syringe with needle and scalpel. 2. Inject local anesthetic into the entrance and exit areas, ensuring that the periosteum is thoroughly numb. Femoral nerve block is also an option (see below). 3. Make a small skin incision at the entry site. Use a hemostat to spread the soft tissue down to bone. Note: For a femoral pin, enter medially 1 cm above the physis, which is at the adductor tubercle (Fig. 7.2A). For a tibial pin, enter laterally 1 cm distal to and posterior to the base of the tibial tubercle (Fig. 7.2B). 4. Have an assistant stabilize the limb with longitudinal traction and counter pressure. Select a pin and insert it into the entry hole. Feel the anterior and posterior edges of the bone by gently “walking” the pin along the cortex. Determine the midpoint, and press the tip of the pin in. Adjust the angle of the pin to ensure its exit at the proper position. Maintain pressure. 5. Drill through the bone until the pin tents the skin on the far side. 6. Make a small incision to allow the pin to exit the skin. Advance the pin and place traction bow. Cut any sharp ends off the pin and protect. Fig. 7.2 Insertion sites on children for (A) femoral pin, (B) tibial pin. 1. Modified Bryant’s a. Use for developmental dysplasia of the hip and, rarely, hip fractures for infants (Fig. 7.3). If a higher angle of flexion is desired, a horizontal bar may be used over the top of the crib. 2. Split Russell’s a. Use in children with hip synovitis or awaiting treatment of fracture of midshaft of femur (Fig. 7.4). This may be applied as skin or skeletal traction. The hip and knee are flexed 20 to 30 degrees. The term split is used because in the original Russell’s traction, the same weight was used to provide the vertical as well as the longitudinal traction. 3. Ninety–ninety traction (skeletal traction): Use for treatment of femur fractures in children (Fig. 7.5). It is appropriate for fractures of the proximal, midshaft, or distal femur. Greater supervision is required to obtain an accurate radiograph, however. Fig. 7.3 Modified Bryant’s traction. Fig. 7.4 Split Russell’s traction. Fig. 7.5 “Ninety-ninety” traction. 1. Indications: Use for reduction and immobilization of upper cervical spine fractures and dislocations, such as odontoid fractures, rotatory subluxation, and facet subluxations. Also used for treatment of thoracolumbar spine deformities in preparation for surgery. 2. Technique: Choose halo size so that there is at least 1.5-cm space between the ring and the cranium circumferentially. Titanium is preferred for magnetic resonance imaging (MRI) compatibility. Stabilize the head while obtaining circumferential access by moving to the end of the backboard. Local anesthetic can be injected into desired areas. Systemic analgesia may be given as needed. Anterior pin sites should be 1 cm above the eyebrow and lateral to its midportion to avoid supraorbital and supratrochlear nerves. Posterior pin sites should be diametrically opposite to these. In children under age 12, six to eight pins should be used for increased stability. Torque should be increased incrementally from 2 in-pound at age 2 to 8 in-pound at maturity. 3. If used for traction, weight is increased gradually from around 5 pounds initially. Monitor neurologic status at least once per shift, more frequently if weight is increased. This should include check of cranial nerves and upper and lower extremities. 4. Gardner-Wells tongs: These tongs can be used for temporary traction. This assembly consists of two pins, one above each external auditory meatus, inserted until the indicator tab pops out. 1. Indications: Upper extremity fractures requiring closed reduction but not amenable to single-nerve block 2. Contraindications a. Fracture above distal humerus b. Vascular injury, compartment syndrome c. Allergy to local anesthetics 3. Premedication a. Chloral hydrate, 50 to 100 mg/kg either orally or rectally or b. Other sedative of choice c. Have available Valium for administration 1 to 2 mg intravenously every 2 minutes as needed for convulsions (incidence less than 0.5%) 4. Technique a. Intravenous access in each upper extremity b. Single- or double-cuff tourniquet on upper arm of injured side c. Exsanguinate by gravity for 1 to 2 minutes, and then inflate cuff; if double cuff, use most proximal first. d. Inflation pressure: 200 to 250 mm Hg e. Inject lidocaine, 0.5%: 0.6 to 1.0 ml/kg (3–5 mg/kg) f. Reduce fracture, apply splint or cast, and confirm with radiograph. g. If tourniquet pain occurs, change from proximal to distal cuff. h. Release: Tourniquet must be up for at least 30 minutes to allow tissue binding of lidocaine. i. Deflate tourniquet for few seconds, and then reinflate and repeat over 2 minutes to allow gradual release of anesthetic. Barnes CL, Blasier RD, Dodge BM. Intravenous regional anesthesia: a safe and cost-effective outpatient anesthetic for upper extremity fracture treatment in children. J Pediatr Orthop. 1991;11(6):717–720 1. Indications a. To provide anesthesia for reduction of fractures of the distal humerus or below the hand, wrist, forearm, elbow, distal arm b. For wound debridement, closure, or incision 2. Contraindications a. Allergy to local anesthetics b. Inability to abduct shoulder c. Bleeding diathesis d. Vascular injury or compartment syndrome 3. Premedication to decrease anxiety a. Intravenous line in case it is needed b. Children 1) Chloral hydrate 50 to 100 mg/kg administered orally or rectally or 2) Intravenous titration with benzodiazepine/narcotic 4. Technique of block administration (Fig. 7.6): a. Draw up anesthetic agent: Lidocaine or Mepivacaine 5 mg/kg in children, 7 mg/kg in adults (usual adult dose is 40 cc of 1% solution) b. Intravenous line and sedation as desired c.
 Skin and Skeletal Traction
Skin and Skeletal Traction
Indications for Skin Traction
Skin Traction Application
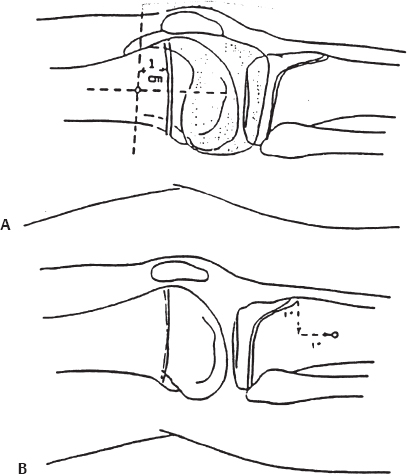
Skeletal Traction Pin Placement
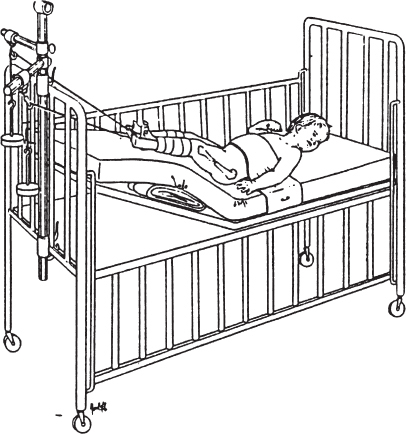
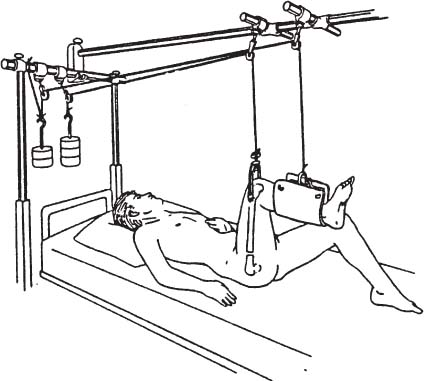
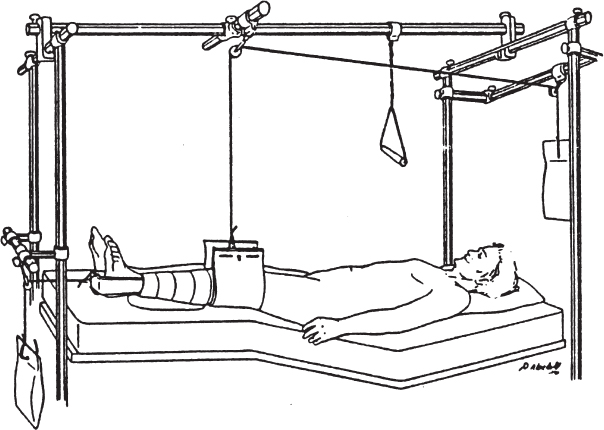
Traction Assembly
Pediatric Halo and Halo–Vest Application
 Regional Blocks
Regional Blocks
Intravenous Regional Anesthesia (Bier Block)
Bibliography
Axillary Block
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree