1 Anatomy and Normal Development in Children Knowledge of normal growth and development is important for evaluation and diagnosis. This chapter contains relevant anatomy and developmental norms. It also contains a description of normal gait and guidelines for interpreting a gait study. When evaluating a patient at risk of developmental delay, it is helpful to have norms to determine whether a delay is present. The section below presents the chronological appearance of certain key motor, social, and language skills. The Denver II Developmental Screening Test displays these in graphic form. Although the orthopedic surgeon will not perform the test formally, it provides an excellent summary of developmental milestones. Table 1.1 provides the norms for milestones. Information on the Denver II Developmental Screening Test is available from the following: Denver Developmental Materials Inc PO Box 371075 Denver, CO 80237 E-mail: generalinfo@denverii.com The Denver II Developmental Screening Test can be used with children from birth to age 6 years. It is used to decide which children should be referred for diagnostic evaluation. It is not an IQ test. It has four sections: personal–social, fine motor, language, and gross motor. The Denver II scoring chart provides an excellent summary of motor development. Table 1.1 Norms for Motor Milestones
 Neurodevelopmental Norms
Neurodevelopmental Norms
Skill | Mean Age (mo) | St. Dev. |
|---|---|---|
Roll from back to stomach | 3.6 | 1.4 |
Roll from stomach to back | 4.8 | 1.4 |
Sit tailor-style | 5.3 | 1.0 |
Sit unsupported | 6.3 | 1.2 |
Crawl (many never crawl) | 7.8 | 1.7 |
Pull to stand | 8.1 | 1.6 |
Cruise | 8.8 | 1.7 |
Walk | 11.7 | 2 |
Run | 15 | 3 |
Source: Palmer F, Capute A. Keys to developmental assessment. In McMillan J, ed. Oski’s Pediatrics, 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2006:789
Psychomotor Skills in Children During Years 1 Through 5
• Neonatal period (first month)
Supine: Generally flexed and tone a little low
• 2 Months
Prone: Head sustained in plane of body in ventral suspension
Social: Smiles on social contact
• 4 Months
Supine: Reaches and grasps objects and brings them to mouth
Sitting: No head lag on pull to sitting position
• 4 to 6 Months
Prone: Rolls over to supine
Semantics: Turns to his or her own name
• 7 Months
Sitting: Sits briefly with support of pelvis
Adaptive: Transfers objects from hand to hand
• 10 Months
Standing: Pulls to standing position
Motor: Creeps or crawls
• 12 to 18 Months
Syntax: Speech generally consists of single-word utterances (comment)
• 12 Months
Motor: Walks with one hand held, “cruises” or walks holding on to furniture
Language: Two “words” besides mama and dada
• 15 Months
Motor: Walks alone, crawls up stairs
• 18 Months
Motor: Runs stiffly
Social: Feeds self
• 24 Months
Motor: Opens doors
Syntax: Uses two- and three-word combinations (telegraphic speech)
• 30 Months
Motor: Jumps
• 36 Months
Motor: Goes up stairs alternating feet, stands momentarily on one foot
Motor: Hops on one foot, throws ball overhand
• 60 Months
Motor: Skips
Bibliography
Richter SB, Howard BJ, Sturner R. Normal infant and childhood development. In McMillan J, ed. Oski’s Pediatrics. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2006:593–601
Referral Criteria
Referral should be made if the infant is displaying any of the following:
1. Not rolling by 6 months
2. Not sitting independently by 8 months
3. Handedness develops too early (by 12 months): May indicate abnormality of opposite side
4. Not walking by 18 months
5. No words by 14 months
 Neurologic Anatomy
Neurologic Anatomy
Sensation
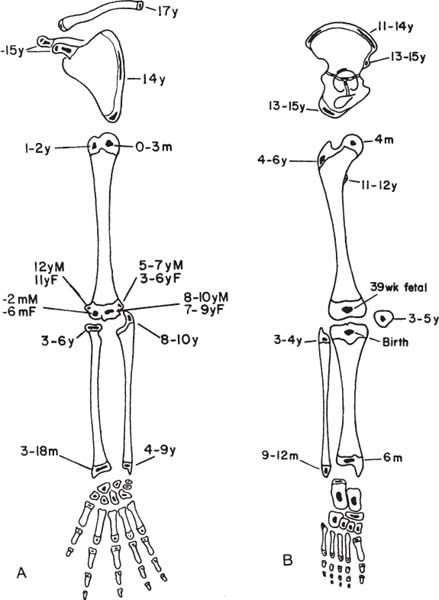
Knowledge of dermatomes will help in the evaluation of neurologic conditions. There is, however, some variation and overlap between levels. Injury to a single nerve root may not produce complete loss of sensation within a dermatome. Sensation should be recorded as increased, decreased, absent, or dysesthetic. The sensation of proprioception and vibration is carried in the dorsal column of the spinal cord: light touch in the ventral spinothalamic tract and pain and temperature in the lateral spinothalamic tract. During neurologic root recovery, pain sensation returns before light touch (Fig. 1.1).
Upper Extremity Motor Examination
Injury to the roots or the cord of the cervical spine follows certain patterns. Even though most muscles have innervation from multiple segments, each root has specific muscles and sensory regions for which it is critical. The diagram below is helpful for diagnosing cervical root lesions and spinal cord injury. Motor testing can be performed in one coordinated sequence, from proximal to distal: deltoid (C5), biceps (C5), wrist extension (C6), finger extension (C7), finger flexion (C8), finger abduction and adduction (T1) (Fig. 1.2).
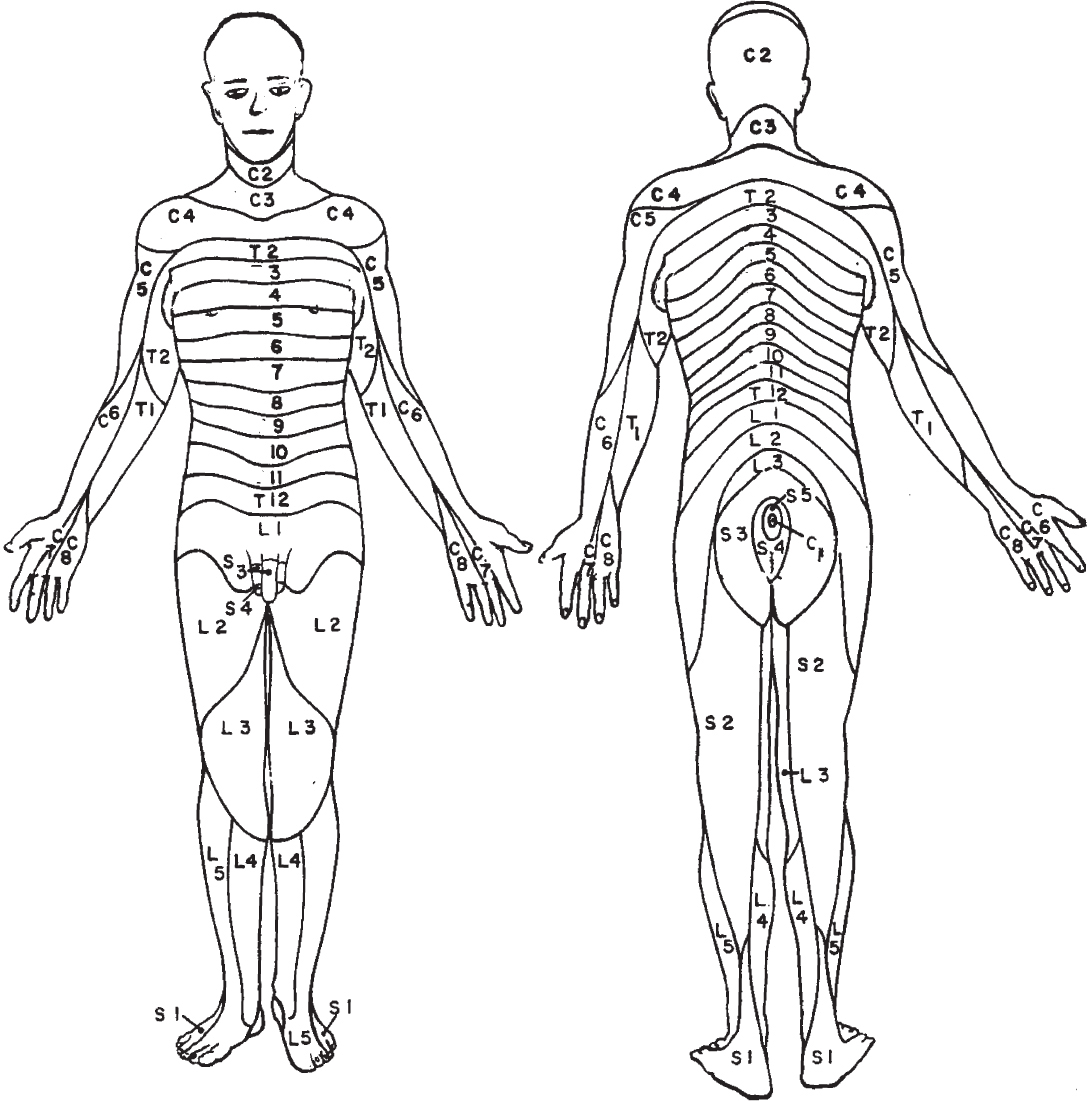
Fig. 1.1 Dermatomes.
Upper Extremity Muscle Innervation
Because most muscles are innervated by multiple segments, it is necessary to know all the roots controlling a given muscle. Fig. 1.3 indicates the roots contributing to a given muscle in the upper extremity. For purposes of strength grading, the following five-grade scale has been widely used:
• Grade 1: Flicker
• Grade 2: Less than antigravity
• Grade 3: Maintains position against gravity
• Grade 4: Moves against submaximal resistance
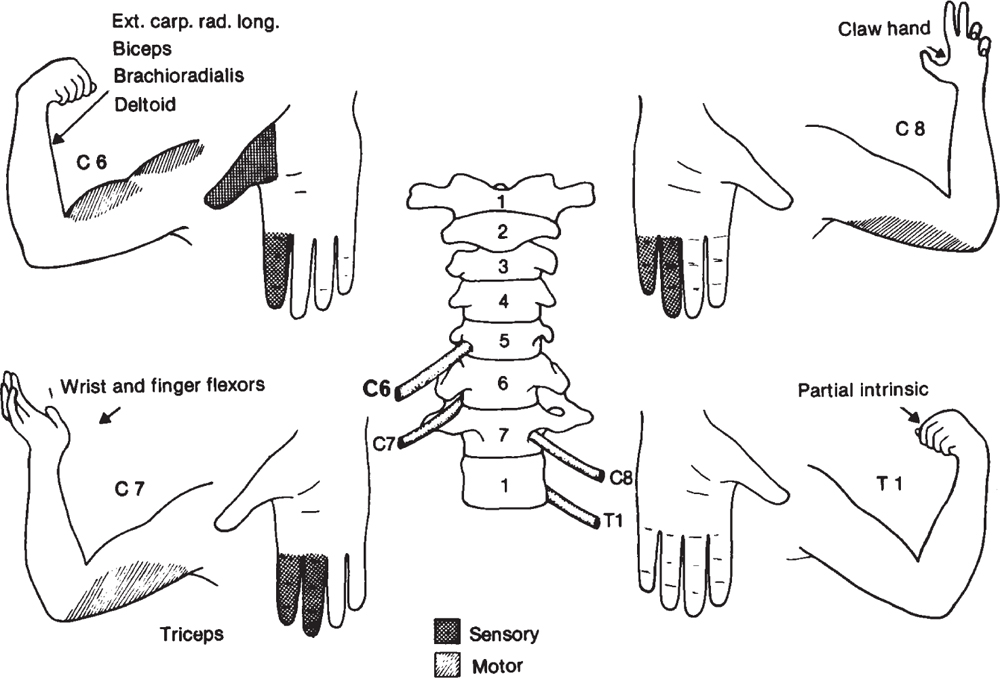
Fig. 1.2 Sensory and motor innervation C6 to T1. Note: Only sensory loss is shown in the shaded hand, and only muscle involvement is shown in the arm. (From McQueen JD, Khan MI. Neurologic evaluation. In Sherk HH, Dunn EJ, Eismont FJ, et al, eds. The Cervical Spine. 2nd ed. Philadelphia: J.B. Lippincott; 1989: 206 (Fig. 4-5). Reprinted with permission.)
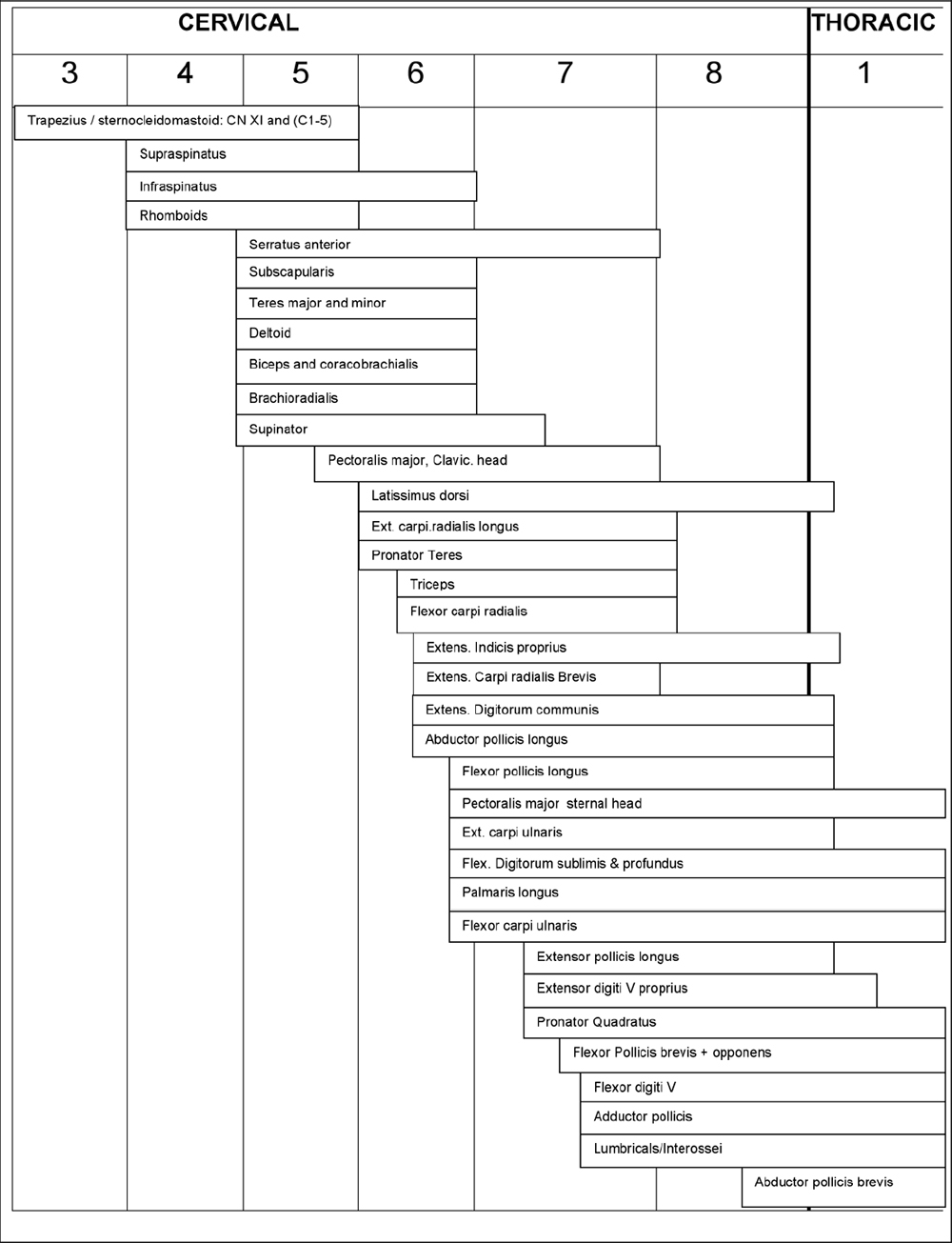
Fig. 1.3 Innervation of muscles of upper extremity.
Formation of the Brachial Plexus
Unless one works with the brachial plexus constantly, it is difficult to remember its anatomy accurately. The anatomy is depicted here to understand injuries from birth and later trauma. Most traction injuries involve the upper roots (Fig. 1.4).
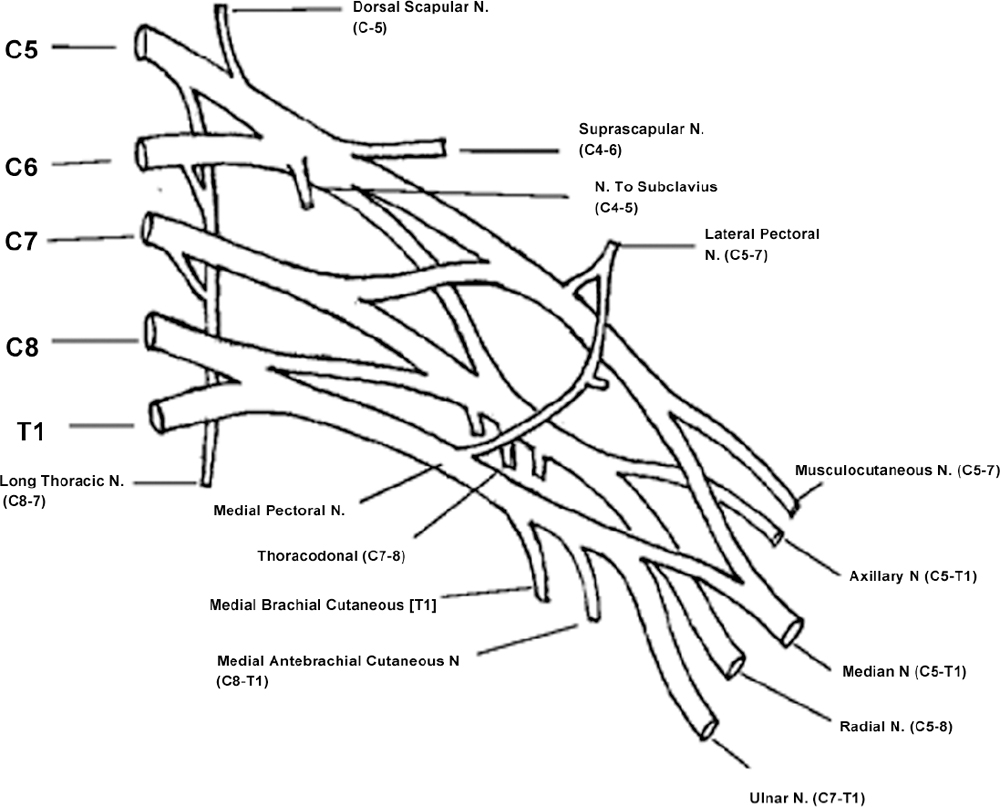
Fig. 1.4 Formation of the brachial plexus.
Peripheral Nerve Testing in the Upper Extremity
In evaluating an injury of the upper extremity in children (such as for supracondylar fracture), it is important to have methods to test the peripheral nerves: the median nerve may be tested by grip or finger flexion and the anterior interosseous nerve (a branch of the median that can be selectively injured) by testing distal interphalangeal flexion of the index finger and thumb, forming an “O.”
• Radial nerve: By extending the thumb, the wrist or the metacarpophalangeal joints.
• Ulnar nerve: By crossing fingers, abducting fingers, or flexing the distal interphalangeal joint of the fifth finger (Fig. 1.5).
Lower Extremity Motor Innervation
Knowledge of lower extremity motor innervation is important for understanding spina bifida, lumbar disk herniation, spinal cord injury, and other conditions. Innervation of muscles is by descending spinal segments at progressively distal levels of the limb, with the notable exception of gluteus maximus, medius, and minimus (L5 through S2).
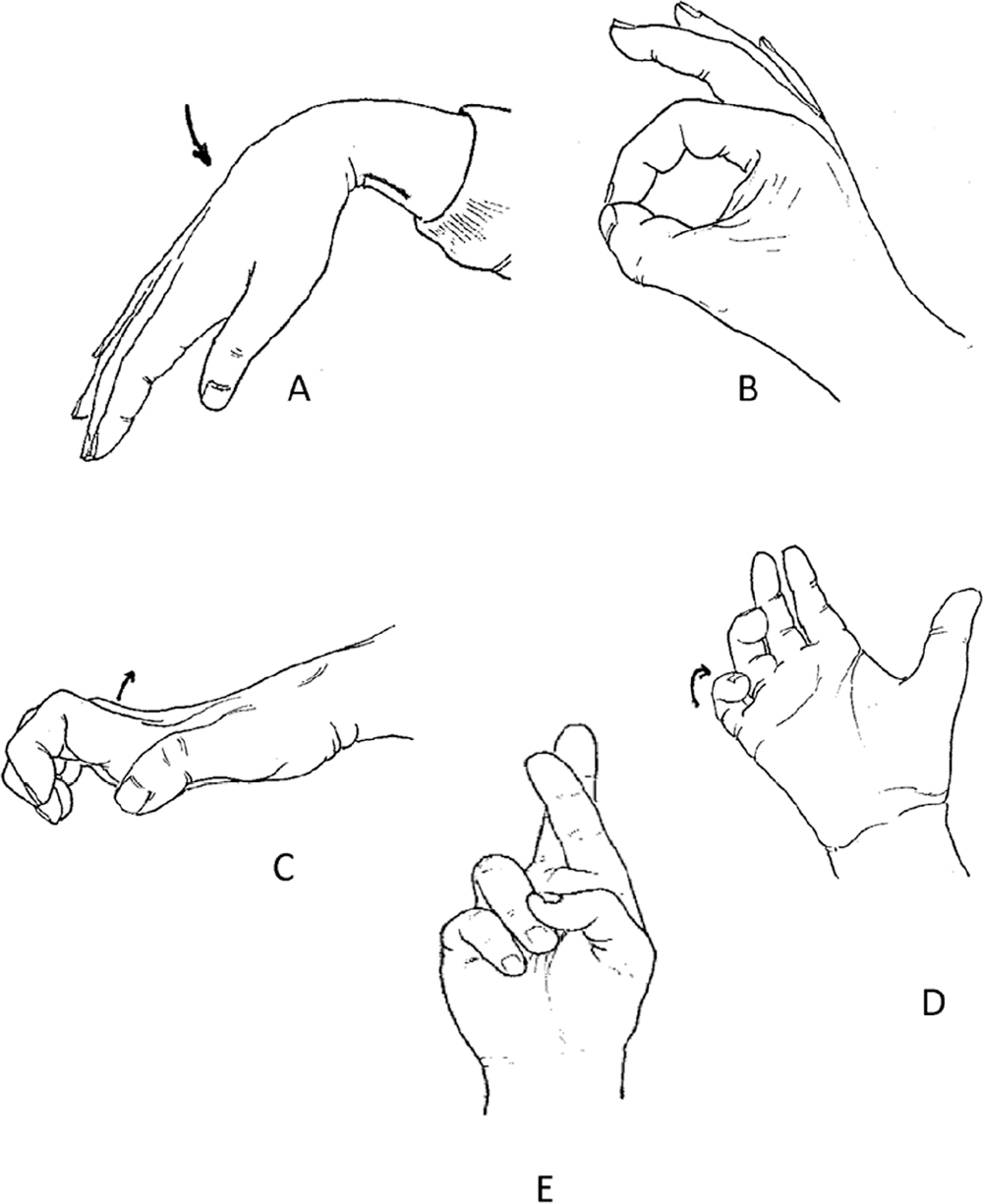
Fig. 1.5 Documentation of the status of all nerves and circulation before treatment of supracondylar humerus fractures. This involves (A) checking active palmarflexion (median nerve); (B) flexion of distal interphalangeal joints of the index finger and thumb–anterior interosseous nerve; (C) dorsiflexion of the metacarpophalangeal joints–posterior interosseous nerve; (D) flexion of the fifth finger distal interphalangeal joint; or (E) crossing of index and second fingers–ulnar nerve.
The most important motors to know are iliopsoas (L1 through L3), adductors (L2 through L4), quadriceps (L2 through L4), hamstrings (L4 through L5), anterior tibialis (L4 through L5), gastrocnemius (S1), and glutei (L5 through S2) (Fig. 1.6).
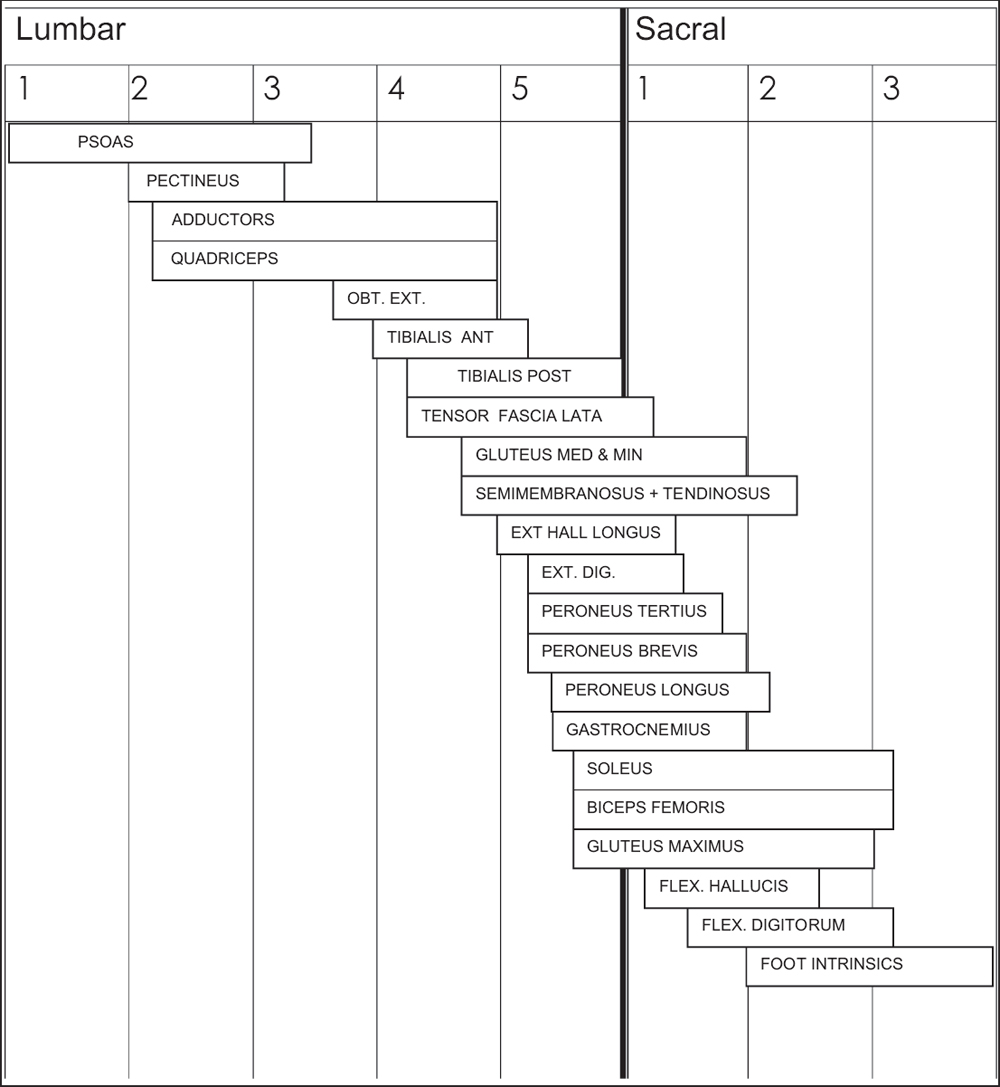
Fig. 1.6 Segmental innervation of muscles of the lower limb.
 Skeletal Development
Skeletal Development
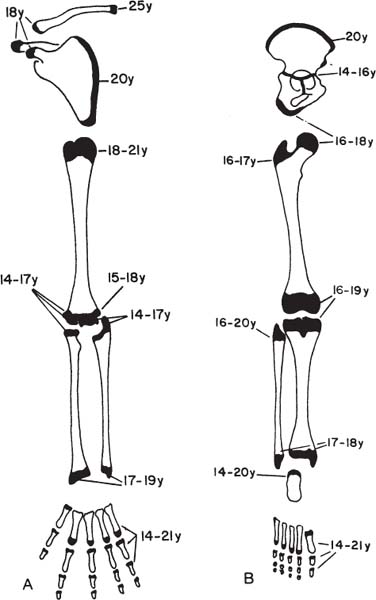
Appearance of Secondary Ossification Centers and Physeal Closure
In many situations it is important to know whether an epiphysis should be ossified at a given age, such as in evaluating a patient with a hip dislocation, skeletal dysplasia, or elbow fracture. Normal times for appearance and closure of the long bones are given in Fig. 1.7; for the hand and foot, see Fig. 1.8.
The following are some important milestones:
1. The distal femoral epiphysis is the first to ossify, at ~39 weeks’ gestation; the proximal tibia ossifies 1 week later.
Fig. 1.7 Age of appearance of secondary ossification centers (A) and physeal closure (B) in the long bones. (From Ogden JA. Radiologic aspects. In Ogden JA, ed. Skeletal Injury in the Child. 2nd ed. Philadelphia: W.B. Saunders; 1990:84 (Figs. 3-28 and 3-29). Reprinted with permission.)
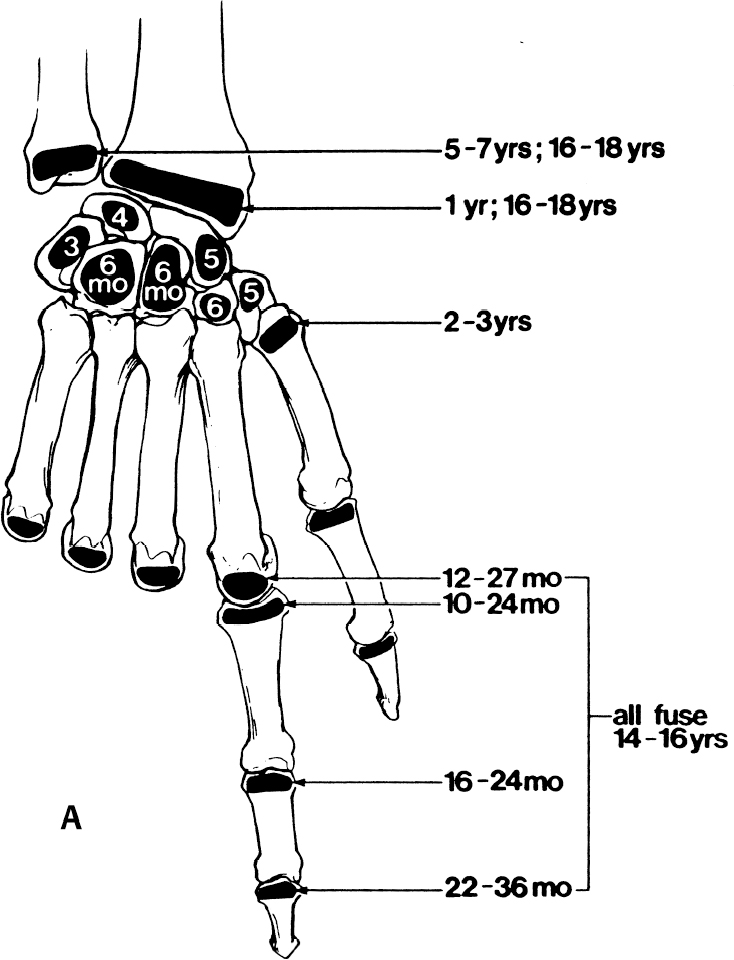
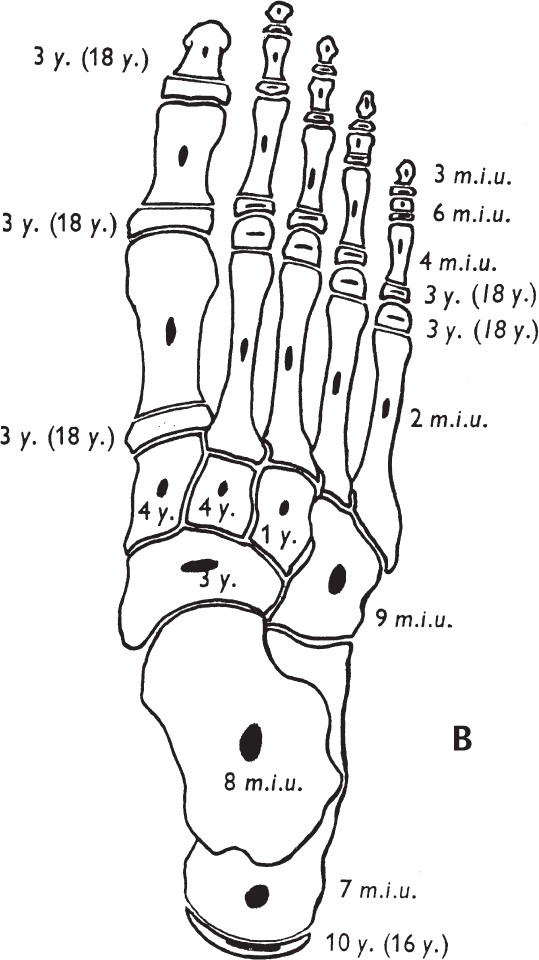
Fig. 1.8 Age of appearance of secondary ossification centers and physeal closure in the hand (A) and foot (B). ([A] from O’Brien ET. Fractures of the hand and wrist region. In Rockwood CA Jr, Wilkins KE, King RE, eds. Fractures in Children. 3rd ed. Philadelphia: J.B. Lippincott Co., 1991: 320 (Fig. 4-1). Reprinted with permission. [B] from Aitken JT, Causey G, Joseph J, Young JZ. The foot. In Aitken JT, Causey G, Joseph J, Young JZ, eds. A Manual of Human Anatomy. Vol IV, Lower Limb. 2nd ed. Edinburgh: E & S Livingstone; 1966:80 (Fig. 30). Reprinted with permission.)
2. The mean time for ossification of the proximal femoral epiphysis is 4 months, but normal may be up to 11 months. The greater trochanter ossifies at 4 to 6 years.
3. The triradiate cartilage closes before Risser I.
4. The tarsal navicular does not ossify until 3 to 4 years, so its location must be inferred from the position of the first metatarsal.
5. The last physis to close is that of the medial clavicle, at age 20 to 25 years.
6. The sequence of ossification about the elbow can be remembered by the mnemonic CRITOE (Fig. 1.9):
• C apitellum (age 2)
• R adial head (age 5)
• I nternal epicondyle (age 7)
• T rochlea (age 9)
• O lecranon (age 10)
• E xternal epicondyle (age 11)
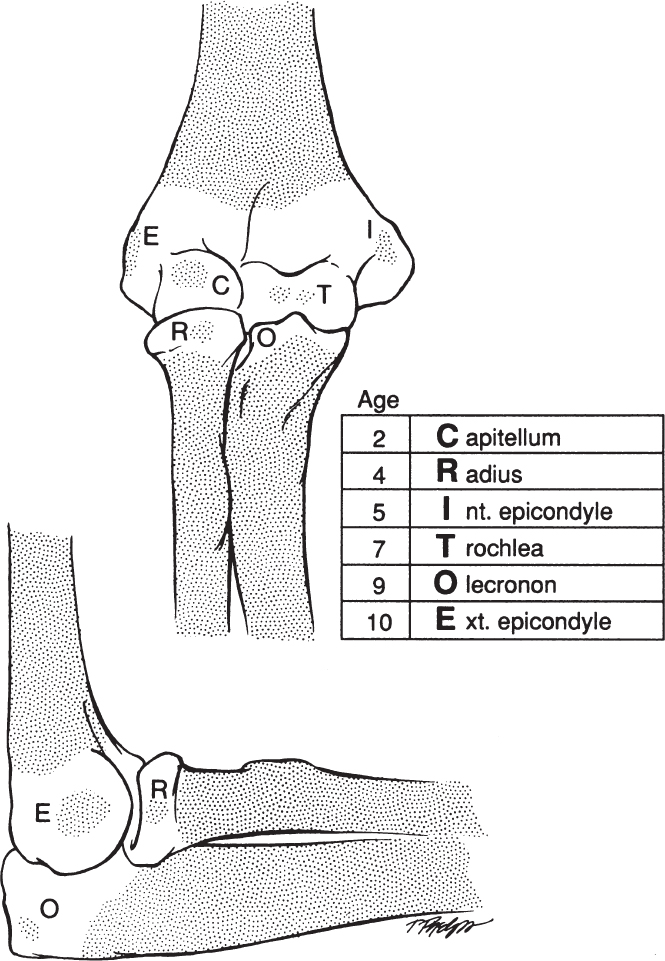
Fig. 1.9 Appearance of age of ossification centers about the elbow can be summarized by mnemonic CRITOE. (From Sponseller PD. Orthopaedic injuries. In Nichols DG, Yaster M, Lappe DG, Buck JR, eds. Golden Hour: The Handbook of Advanced Pediatric Life Support. St. Louis: Mosby Year Book; 1991:350 (Fig. 18-3). Reprinted with permission.)
7. Angle of distal humeral articular surface: This angle is key to understanding any angular change about the elbow. It is best measured by the Baumann angle, between the humeral shaft and the lateral condylar physis (Fig. 1.10). Its normal value is 72 ± 4 degrees. There is no difference between sexes or ages from 2 to 13 years.
8. Determination of skeletal age using the elbow: This can be determined by the olecranon or modified Sauvegrain method (Fig. 1.11). The five stages include (1) bipartite olecranon, (2) half-moon–shaped olecranon, (3) rectangular olecranon, (4) partially fused, or (5) fully fused. They occur at 6-month intervals of skeletal age from 11 years in girls and 13 in boys. The fully fused olecranon occurs at skeletal age of 13 in girls and 15 in boys and marks the deceleration of growth velocity.
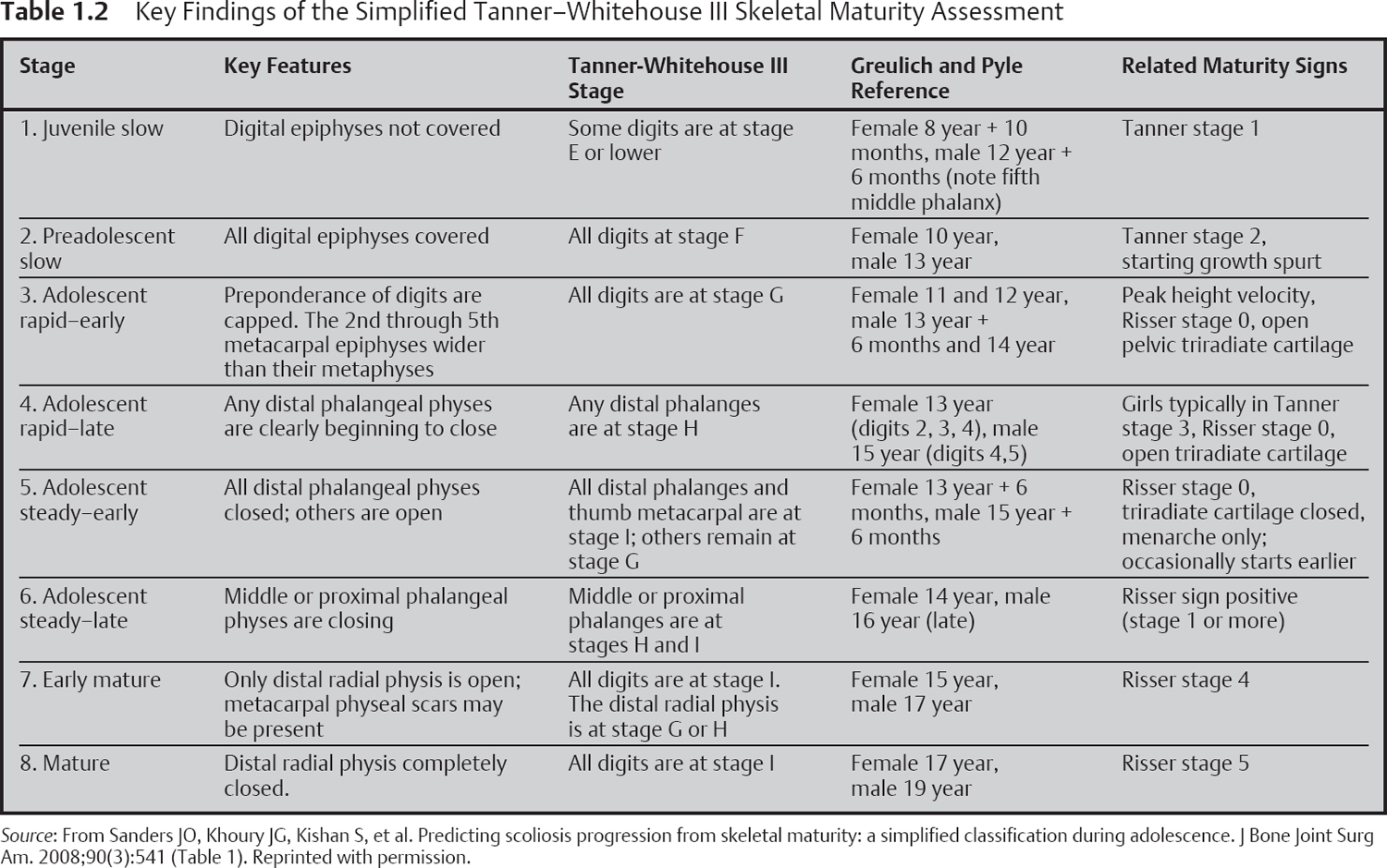
9. Determination of skeletal age using the Modified Tanner–Whitehouse III Skeletal Maturity Assessment (Table 1.2 and Fig. 1.12)
Patients with curves over 30 degrees at stage 3 to 4 are at high risk of progression to surgery, and patients with curves less than 20 degrees at this stage are at low risk.
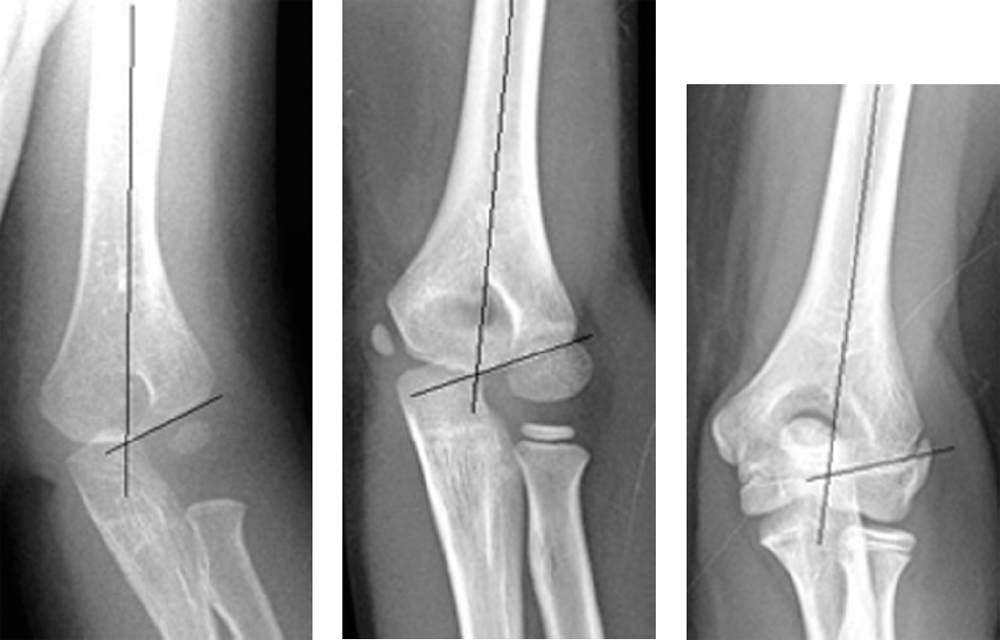
Fig. 1.10 Differing configuration of the distal humerus and landmarks used for measurement of the Baumann angle.
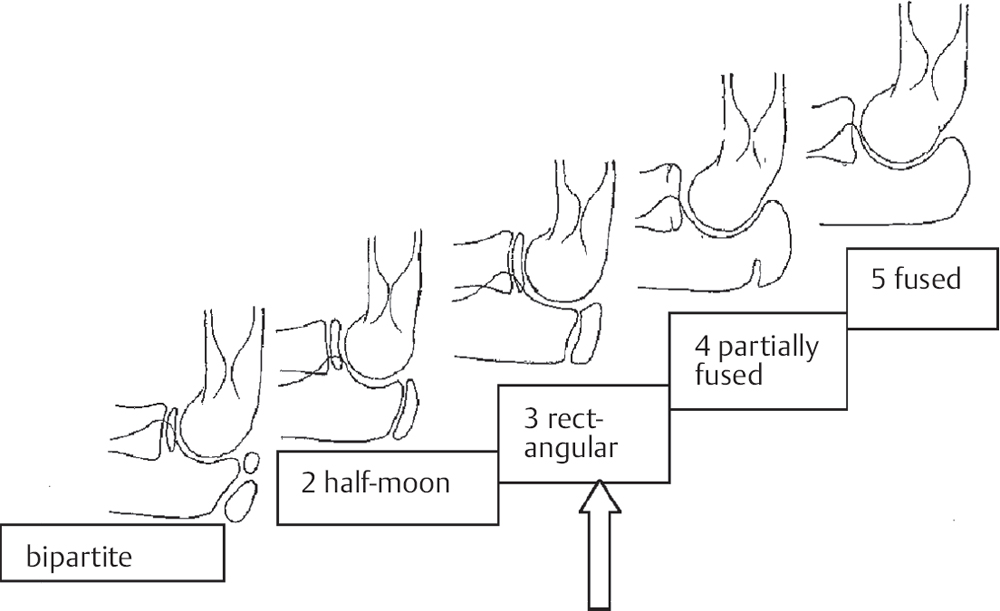
Fig. 1.11 Simplified Sauvegrain method for skeletal maturity assessment.
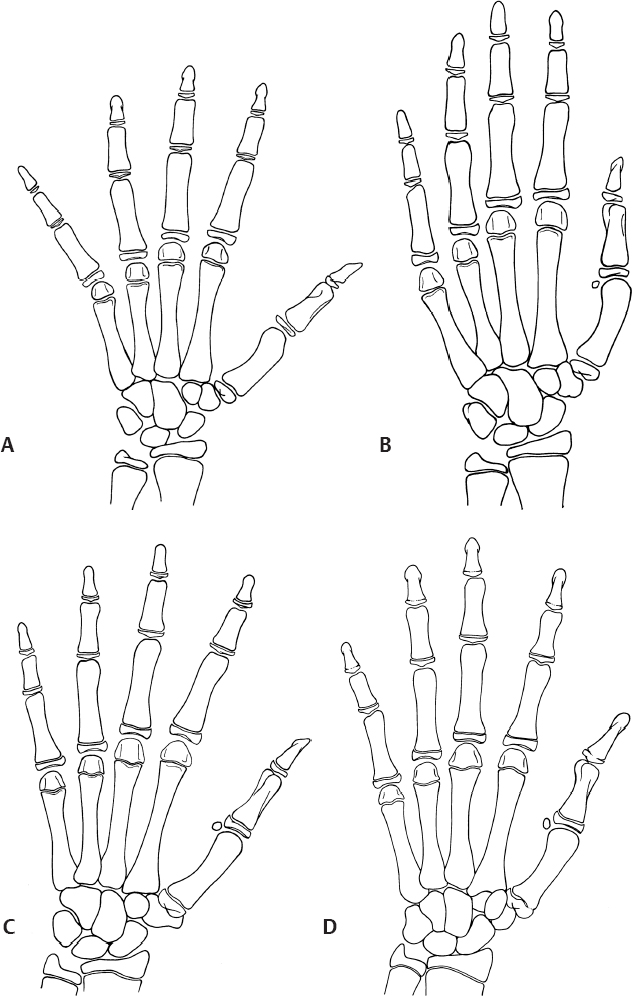
Fig. 1.12 Simplified Tanner–Whitehouse III method for skeletal maturity assessment. Note that the distal phalangeal epiphyses are the key to the curve acceleration phase (CAP). When they are capped, the phase is beginning, and when they are all closed, the phase has ended. (A) Stage 1: All digital epiphyses not covered (epiphyses not as wide as metaphyses). (B) Stage 2: All digital epiphyses are covered. (C) Stage 3: Most epiphyses cap their metaphyses. Capping is a small bend over the metaphyseal edge. This is also the beginning of the CAP.(D) Stage 4: At least one of distal phalanges closed. (From Sanders JO, Khoury JG, Kishan S, et al. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am. 2008;90(3):540-553 (Figs. 1-B, 2-B, 3-B, 4-B). Reprinted with permission.)
Cervical Spine Radiographic Normal Values for Children
Alignment
1. The cervical spine in children is characterized by increased mobility at C2–3, termed pseudosubluxation, which should not exceed 3 mm.
2. The tip of the odontoid should not be more than 1 cm from the basion of the skull (anterior rim of the foramen magnum).
3. The physis of the odontoid normally fuses between 3 and 6 years.
4. The atlas–dens interval should be less than 4 mm.
5. The Power ratio is the ratio of the distance from basion to posterior arch of C1 divided by the distance from the opisthion to the anterior arch of C1. This ratio should be less than 1.
6. The retropharyngeal space should not exceed 8 mm; if greater, it could signify bleeding from a fracture or a dislocation.
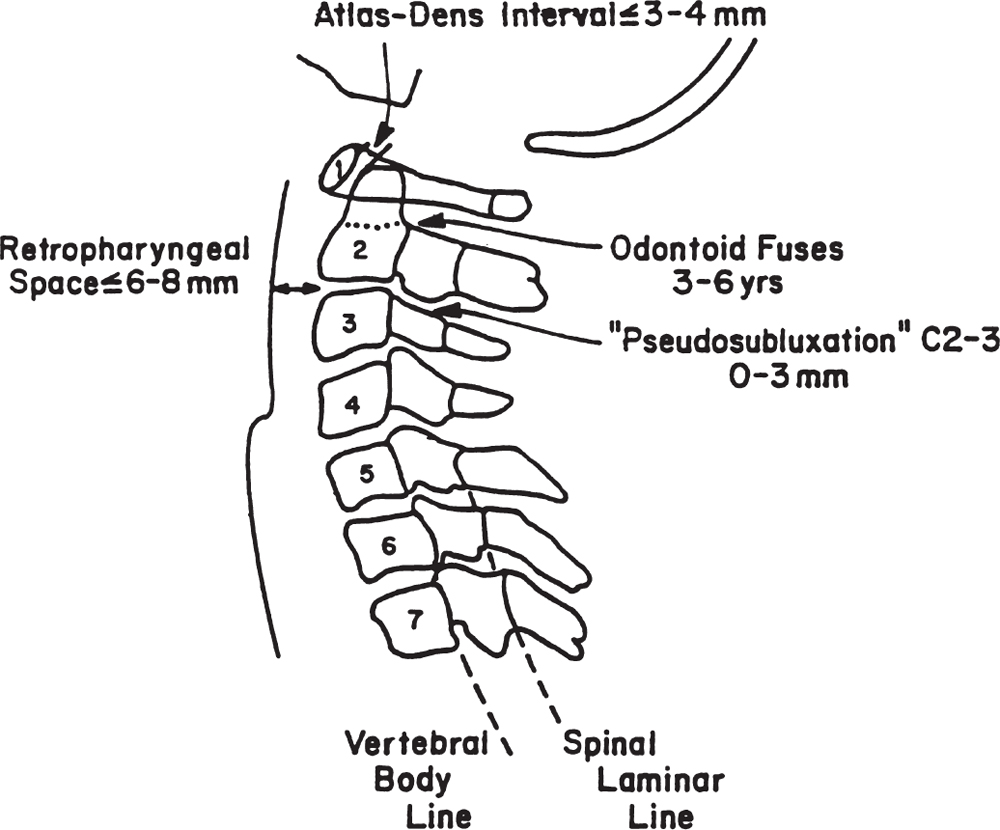
Fig. 1.13 Normal values of cervical spine alignment for children. (From Spon-seller PD. Orthopaedic injuries. In Nichols DG, Yaster M, Lappe DG, Buck JR, eds. Golden Hour: The Handbook of Advanced Pediatric Life Support. St. Louis: Mosby Year Book; 1991:353 (Fig. 18-4). Reprinted with permission.)
7. The spinal laminae should form a smooth line posteriorly.
8. The vertebral bodies may be wedged anteriorly, especially on their superior surfaces, until age 10 (Fig. 1.13).
Development of the Cervical Spine
First Cervical Vertebra (Atlas)
1. Body: Not ossified at birth; the center (occasionally two centers) appears during the first year after birth; the body may fail to develop, and forward extension of neural arches may take its place.
2. Neural arches: Appear bilaterally at approximately the seventh fetal week; most of the anterior portion of superior articulating surface is usually formed by the body.
3. Synchondrosis of spinous processes: Unites by the third year. Union rarely is preceded by the appearance of a secondary center within the synchondrosis.
4. Neurocentral synchondrosis: Fuses at approximately the seventh year (Fig. 1.14).
Second Cervical Vertebra (Axis)
1. Body: One center (occasionally two) appears by the fifth fetal month.
2. Neural arches: Appear bilaterally by fetal month 7.
3. Neural arches fuse posteriorly by the year 2 or 3.
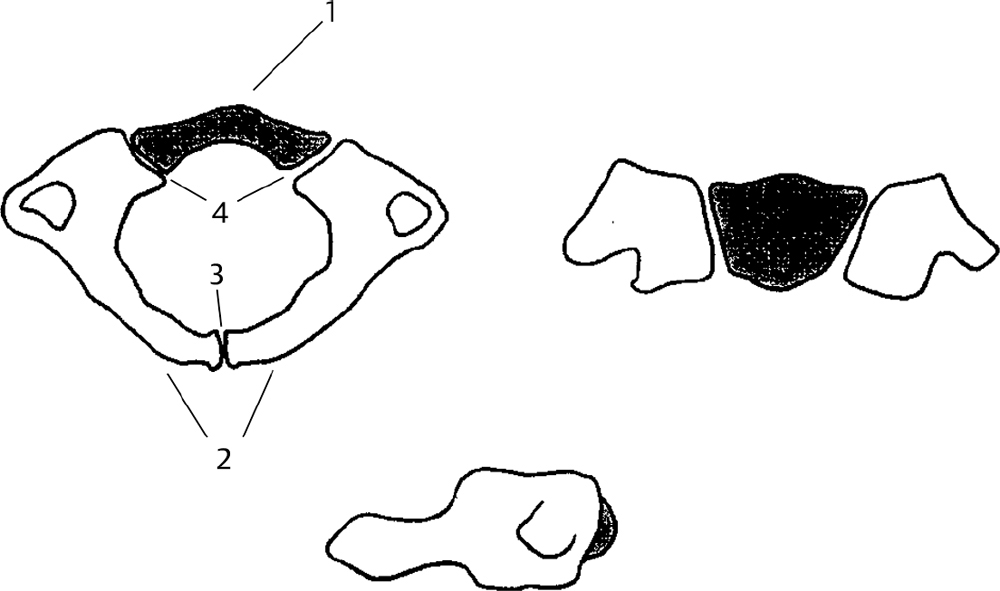
Fig. 1.14 Axial, coronal, and sagittal views of the developing atlas. The first cervical vertebra is formed by three ossification sites: the anterior arch (gray), or centrum, and the two neural arches (white). (From Oh BC, Wang MY. Cervical anatomy and surgical approaches. In Kim DH, Betz RR, Huhn SL, Newton PO, eds. Surgery of the Pediatric Spine. New York: Thieme; 2008:95 (Fig. 8-1). Reprinted with permission.)
4. Bifid tip of spinous process: Occasionally a secondary center is present in each tip.
5. Neurocentral synchondrosis: Fuses at 3 to 6 years
6. Inferior epiphyseal ring: Appears at puberty and fuses at around 25 years
7. “Summit” ossification center for odontoid: Appears at 3 to 6 years and fuses with the odontoid by 12 years
8. Odontoid (dens). Two separate centers appear by fetal month 5 and fuse with each other by month 7
9. Synchondrosis between odontoid and neural arch: Fuses at 3 to 6 years
10. Synchondrosis between odontoid and body: Fuses at 3 to 6 years
11. Posterior surface of body and odontoid (Fig. 1.15)
Spinal Growth
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree