Chapter 2 Common presentations and diagnostic techniques
Common presentations of pelvic malalignment
Establishing the diagnosis of malalignment
Tests used for the examination of the pelvic girdle
Simultaneous bilateral SI joint malalignemnt
1. a failure of disc resection and subsequent desperation measures, such as disc-to-disc or lumbo-pelvic fusions, to relieve the persisting low back pain
2. the recognition of the short-and long-term complications of chymopapaine ‘discectomy’
3. the evolution of the computed tomography (CAT) scan and, subsequently, magnetic resonance imaging (MRI), with gradual recognition of the fact that disc protrusions were common but did not necessarily cause back pain.
1. Publications of studies in the mid-1990s suggesting initially that approximately 20–30% of low back and referred pain came from the SI joint itself and/or the surrounding ligaments, muscles and other soft tissues involved in the functioning of the joint (Maigne et al. 1996, Schwarzer et al. 1995).
2. Presentation of the first International World Congress on ‘Low Back Pain and its Relationship to the Sacroiliac Joint’, hosted by San Diego in 1992 and, subsequently, by other major cities on a tri-annual basis. The congress has become a forum for the presentation of clinical experience and ongoing research on the SI joint and the lumbo-pelvic hip complex and has led to the publication of a number of books and articles in this field (e.g. Vleeming et al. 2007; Lee 2011).
1. The ‘inner core’ muscles help stabilize the pelvis and lumbar spine and, in tandem with the ‘outer core’ muscles, ligaments and myofascia form a system of well-defined ‘slings’ or ‘cylinders’ that can:
2. As a result of the functional kinetic interlinkage of the skeleton with these core muscles and myofascial ‘slings’, pathology affecting any of these structures can stress other proximal and even distal sites, sometimes to the point of interfering with their proper function and causing them to become another ‘pain generator’ (Vleeming & Stoeckart 2007; see also Ch. 8). Rotation of a vertebra, pelvic malalignment, excessive tension in a particular ligament or muscle are all interlinked and affect the function of the rest of the musculoskeletal system. Treatment needs to address that fact; it cannot be restricted to one site and will often require use of more than one treatment modality in order to be successful.
3. Malalignment of the pelvis and spine initially may not be painful. However, with time the stress on an increasing number of structures is more and more likely to result in:
4. All these factors combined are now felt to be the primary cause and/or an aggravating factor in as many as 50-60% of those presenting with low back pain and referred pain symptoms from this site, or ‘pain generator’ (Vleeming & Stoeckart 2007). Pain may localize to the structure initially involved (i.e. vertebra, lumbosacral junction, SI joint or other) but even at the onset can present as referred pain felt only nearby or at a distant site on the same or opposite side (see ‘Introduction 2002’; Fig. 3.63). Eventually, the abnormal stress pelvic malalignment exerts on soft tissues and joints throughout the body may cause them to become painful and a source of referred pain, so that the actual site or sites where the pain is felt may be misleading to the person reporting the pain and to those trying to determine and treat the underlying problem that precipitated this chain of events. An example is the common complaint of pain ‘from the hip joint’ on one side, when the pain is actually:
5. Recognition of malalignment and the typical problems it can cause is, therefore, a key factor in helping determine whether the symptoms and signs on clinical examination are attributable to the malalignment per se, or whether the malalignment is covering up an underlying clinical problem.
The sacroiliac joint
The SI joints are planar joints that function to:
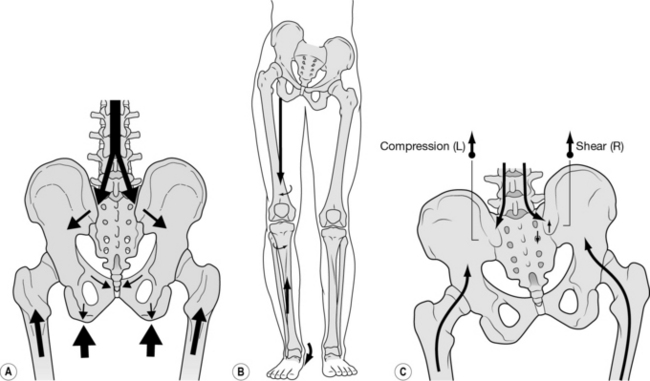
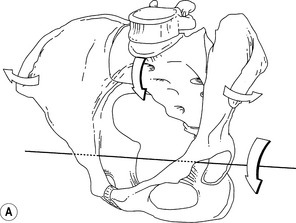
1. transfer the loads generated by gravity and the weight of the trunk and upper body to the ilia and onto the ischial tuberosities in sitting and through the hip joints to the lower extremities in standing (Fig. 2.1A)
2. transfer weight in the opposite direction, in sitting, standing, walking or falling onto one or both ischial tuberosities or the knees or feet – through the ilia onto the sacrum and upward by way of the lumbosacral junction (Fig. 2.1,B,C)
3. act as a shock absorber, particularly at heel-strike and
4. diminish any iliac-on-sacral surface translation or actual shear, when properly positioned (Fig. 2.1A).
Some SI joint motion does occur and seems to:
1. decrease the energy cost of:
3. help decrease stress on the pelvic ring of bones
4. absorb stresses and store energy
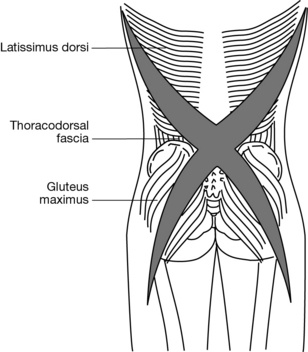
Fig. 2.35 The oblique systems of the ‘outer unit’. Posterior oblique system.
(From Lee 1999, as redrawn courtesy of Snijders et al. 1995.)
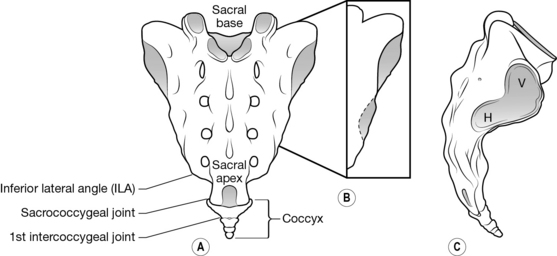
Anatomy, development and aging
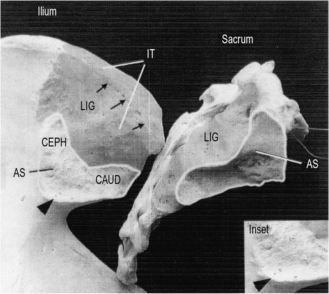
1. the articular surfaces of the SI joint eventually assume an L-shape, with a shorter, almost vertical, upper arm and a longer, lower arm directed posteriorly and inferiorly (Figs 2.2, 2.3C)
2. these arms can be oriented in a different plane relative to the vertical axis, creating a propeller-like appearance (Fig. 2.3B).
3. with time, the ‘propeller’ aspect of this ‘L-shape’ is accentuated by the development of complementary convexities and concavities, variously described as follows:
4. in addition, the sacrum widens anteriorly, creating an anterior-to-posterior wedging effect (Figs 2.2, 2.3, 2.4B, 2.10A, 2.11A, 2.46BD).
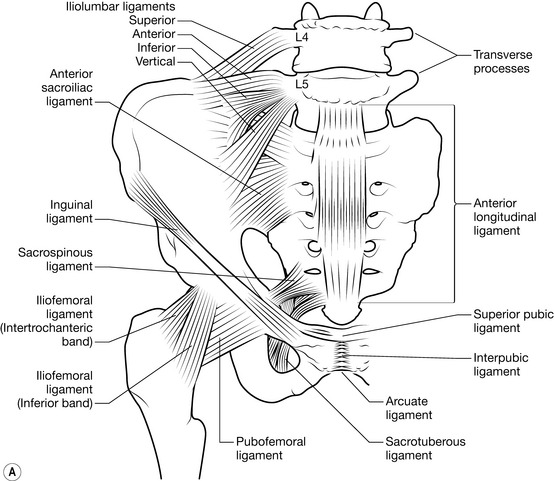
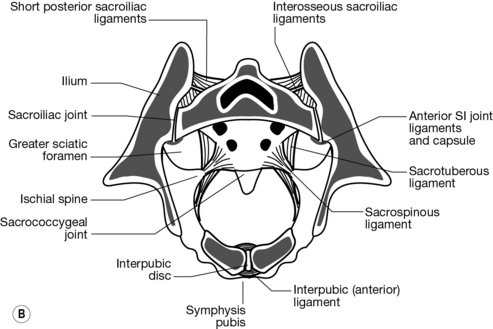
Third, the joint capsule thickens anteriorly to form the anterior or ventral sacroiliac ligament; this is a weak ligament that has been shown to be continuous with the anterior fibres of the iliolumbar ligament (Fig. 2.4A). The interosseous ligament forms the posterior border of the joint; it constitutes the strongest ligament supporting the SI joint and makes up for what is usually a rudimentary or even absent posterior joint capsule (Figs 2.4B, 2.13Aiii ). Additional support comes from the short posterior (dorsal) sacroiliac ligaments, the long posterior (dorsal) sacroiliac ligament, also the iliolumbar, sacrotuberous and sacrospinous ligaments (Figs 2.5A, 2.45). The sacrum literally ends up suspended between the ilia by these ligaments.
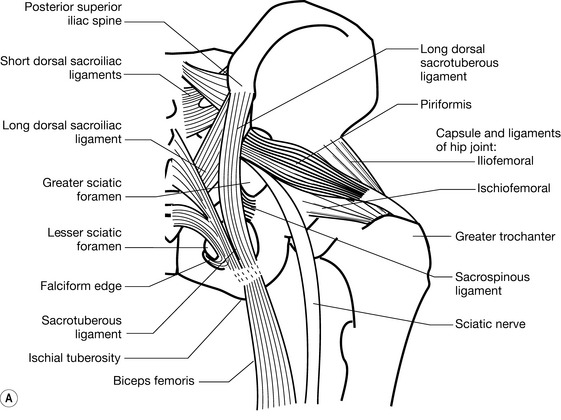

Fig. 2.5 (A) Posterior pelvic ligaments and muscles that act on the sacroiliac joint (see also Figs 2.37, 2.45). (B) Gluteus maximus.
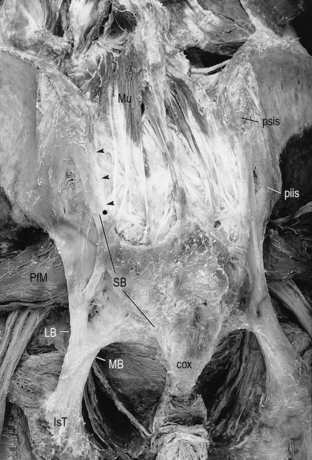
Fourth, Bellamy et al. (1983) observed that the SI joint is surrounded by the largest and most powerful muscle groups in the body but that none of these directly influenced the movement of this joint. However, as Lee pointed out (1992a), very few articulations in the body are actually capable of independent motion, and although the muscles crossing the SI joint are not typically described as prime movers of that joint, motion can occur at the SI joint as a result of their contraction. Lee went on to list 22 muscles that do affect SI joint movement, ranging from latissimus dorsi proximally to sartorius distally. Richard (1986) observed that 36 muscles have their insertion on each ilium but that only 8 of these are also attached to the sacrum; some of the others just cross the joint but provide a key function in establishing and maintaining the axes of movement (e.g. gluteus maximus posteriorly; see Figs 2.5B, 2.37) or stabilizing the joint (e.g. iliacus anteriorly; see Figs 2.46B, 4.2).
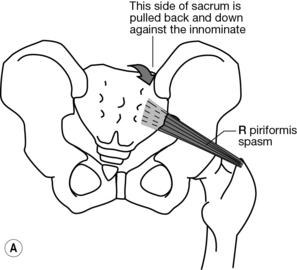
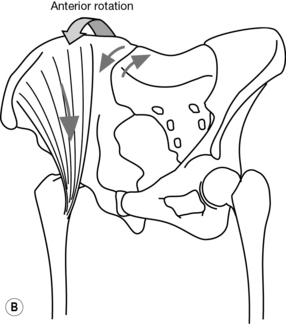
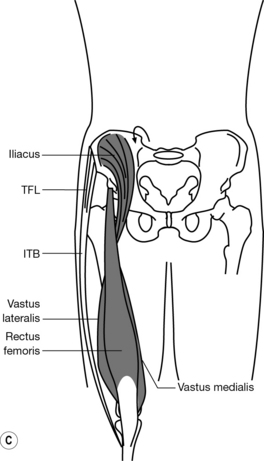
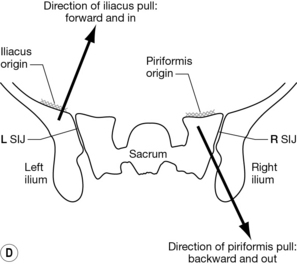
Fig. 2.46 Stabilization of the sacroiliac joint (SIJ) through wedging of the anteriorly widening sacrum (see also Figs 2.2B, 2.3, 2.4B, 2.10A, 2.11A). (A) Piriformis pulling the sacrum backward against the innominate. (B) Iliacus pulling the innominate forward against the sacrum. (C) Anterior innominate rotation through the action of iliacus, rectus femoris and the tensor fascia lata/iliotibial band complex. (D) Wedging effect viewed from the top of the joint.
The work of Vleeming et al. (1989a) is of particular interest in this respect. From their initial dissections on 12 cadavers, these authors reported that gluteus maximus was attached to the sacrotuberous ligament in all cases. In 50% of dissections, there was also a ‘fusion’ of the sacrotuberous ligament, unilateral or bilaterally, with the tendon of the long head of biceps femoris at its origin (Figs 2.6, 2.37). In some specimens, ‘fusion’ to the ligament was complete so that there was actually no connection of this muscle to the ischial tuberosity itself.
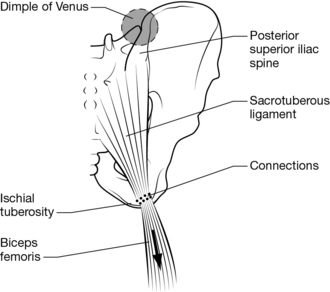
Fig. 2.6 Tension in the sacrotuberous ligament can be augmented by increasing tension in the biceps femoris, and vice versa, when there are fibrous connections between the ligament and the muscle (see also Figs 2.37, 2.59). Note the left ‘dimple of Venus’, overlying the depression formed at the underlying junction of the sacral base with the left ilium.
(Redrawn courtesy of Vleeming et al. 1997.)
Vleeming et al. (1989b) showed how load application to the sacrotuberous ligament, either directly to the ligament or by way of its continuations with the long head of biceps femoris or the attachments of gluteus maximus, significantly diminished the ventral (forward) rotation of the base of the sacrum (Figs 2.6, 2.59). They went on to demonstrate that these forces resulted in a compression of the sacral and iliac surface, increasing the coefficient of friction and thereby decreasing movement at the SI joint by what they termed ‘force closure’, which will be discussed further under ‘self-locking mechanisms’ and ‘form and force closure’ below (Vleeming et al. 1990a, 1990b). The link of the sacrotuberous (ST) ligament to rectus femoris has been repeatedly verified subsequently and also, more recently, evidence that this ligament is usually connected to semimembranosus as well (Barker & Briggs 2004).
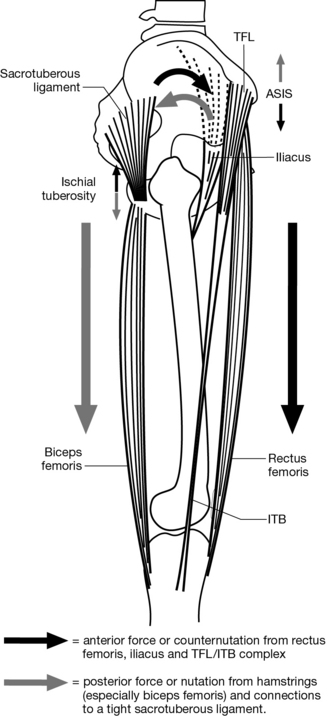
Fig. 2.59 Torquing/rotational forces on the innominate caused by tightness in the attaching muscles or ligaments (see Figs 2.46B,C for an anterior view). ASIS, anterior superior iliac spine.
These findings are but one illustration of how specific muscles may indirectly affect the sacrum, the innominate bones and hence the function of the joints of the pelvic girdle by causing joint motion, compression or both. Recent work by these and other authors (e.g. Pool-Goodzwaard et al. 2003; DeRosa & Porterfield 2007) has more clearly defined the role of these so-called ‘inner’ and ‘outer’ pelvic ‘core’ muscles as dynamic stabilizers of the SI joints in particular and of the lumbo-pelvic-hip girdle and trunk in general (see ‘Kinetic function and stability’ below; Figs 2.29–2.40).
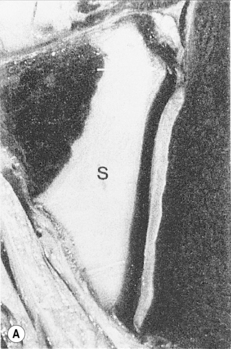
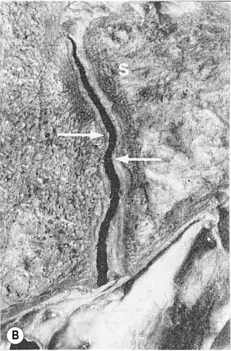
Fifth, the pre-pubertal SI joint surface is described as planar – flat opposing sacral and iliac surfaces that allow for small gliding movements in all directions (Fig. 2.7A). After puberty, most individuals develop ‘a crescent-shaped ridge running the entire length of the iliac surface with a corresponding depression on the sacral side’ (Fig. 2.7B); this complimentary ridge and groove are now felt to lock the surfaces together and increase stability of the SI joint (Vleeming et al. 1990a; Gracovetsky 2007). Also, ‘with increasing age the surfaces become more irregular and prominent’ (Cassidy 1992, 41). The apparent ‘roughening’ of these surfaces may be an adaptation to adolescent weight gain; certainly, work by Vleeming et al. (1990a, 1990b) supported the conjecture that these macroscopic changes represent functional, rather than pathological, adaptations. These authors presented evidence that articular surfaces with both a coarse texture and ridges and depressions have high friction coefficients, consistent with their view that the roughening represents a ‘non-pathological adaptation to the forces exerted at the SI joints, leading to increased stability’ (Vleeming et al. 1990a). The same authors raised two points of particular interest:
1. These physiologically normal intra-articular ridges and depressions could easily be misinterpreted as osteophytes on radiological studies. They pointed out that:
and that:
2. SI joints with intact cartilage showed the friction coefficient to be particularly high ‘in preparations with complementary ridges and depressions’. This led them to conjecture that:
This ‘blocked joint’ may refer to the frequent finding of a decrease or even absence of movement, also referred to as ‘locking’, in one or other SI joint on clinical examination of those presenting with ‘malalignment’ (discussed in detail under ‘Functional or dynamic tests’ below, and in Ch. 3). Note that this decrease or loss of mobility occurs ‘under abnormal loading conditions’. Normal interlocking of the surfaces contributes to joint stability and limitation of range of motion of the SI joint when this is functionally required; for example, to enhance the force-closure mechanism occurring on the weight-bearing side during the gait cycle (Snijders et al. 1993a, Vleeming et al. 1997, Hungerford & Gilleard 2007).
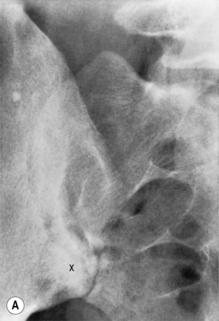
Sixth, the joint may retain its synovial features well into the patient’s 40s or 50s. The fibrocartilage covering the iliac side consistently starts to degenerate early in life, usually by the third decade in males and the fourth or fifth decade in females. By this time, narrowing of the joint space, sclerosis, osteophyte formation, cysts and erosions of the articular surfaces may be evident on X-Rays (Figs 2.8A, 4.38) and on CAT scan/computed tomography (Shibata et al. 2002). Given that these changes could be evident so early on yet were usually asymptomatic, Vleeming et al. (1990a) remarked that they most likely represented a functional adaptive change to an increase in weight. Shibata et al. (2002) and others (Schunke 1938; Bowen & Cassidy 1981; Walker 1986, 1992; Faflia et al. 1998) felt these were ‘degenerative changes’. Iliac osteoarthrosis is indicated by an initial fibrillation of the cartilage, plaque formation and eventual peripheral erosions and subchondral sclerotic changes.
Fibrous adhesions, although more common in older specimens, have been seen in younger males, but ‘to a lesser degree’. Faflia et al. (1998) reported a higher prevalence of advanced, asymmetric non-uniform SI joint degenerative changes in obese, multiparous females compared to age-matched normal-weight, non-multiparous women and to men (Lee 2004a). Whereas bony ankylosis is rare, para-articular synostosis has been reported to be a common finding in both males and females over the age of 50 (Valojerdy et al. 1989). Most will continue to show some SI joint movement well into their 70s and 80s (Bowen & Cassidy 1981, Cassidy 1992, Colachis et al. 1963). Some studies have actually refuted the existence of absolute intra-articular ankylosis in the elderly, suggesting that at these age levels they show primarily intra-articular fibrous connections and osteophytes, cartilagenous erosions, plaque formation (Resnick et al. 1975; Walker 1986) – all these resulting in narrowing of the SI joint space (Fig. 2.8B). Schunke back in 1938 reported that actual SI joint fusion attributable to ankylosing spondylitis was more likely to be found in younger subjects; if such a fusion was found in an older person, it was more likely attributable to them having suffered ankylosing spondylitis somewhere in their younger years.
SI joint mobility
Methods of assessment have included:
1. analysis of the SI joint in various positions of the trunk and lower extremities by:
2. computerized analysis using a metronome skeletal analysis system (Smidt 1995)
3. Doppler imaging of vibrations across the SI joint (Buyruk et al. 1995a, 1995b, 1997, 1999; Damen et al. 2002a)
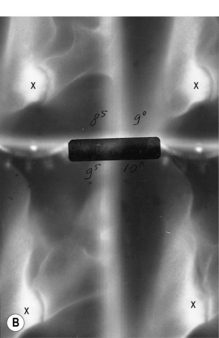
The question was settled more definitively by in vivo sudies using:
1. roentgen stereophotogrammetric analysis – a computerized dual-radiographic technique for assessing the relative movement of implanted titanium balls serving as reference points on the ilium and sacrum (Sturesson et al. 1989, 2000a, 2000b).
2. Kirschner rods implanted in both ilia and the sacrum in healthy volunteers (Jacob & Kissling 1995; Kissling & Jacob 1997).
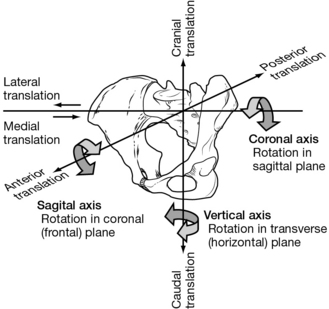
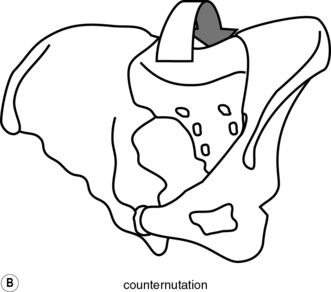
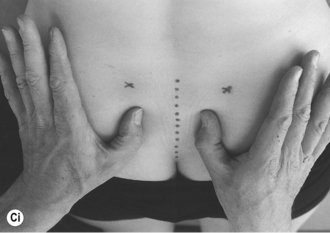
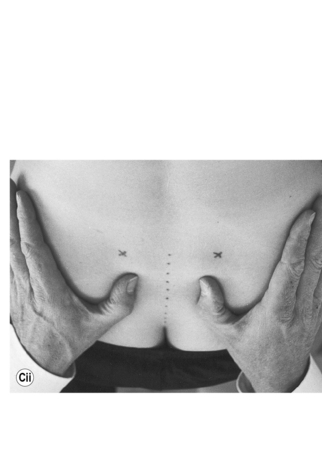
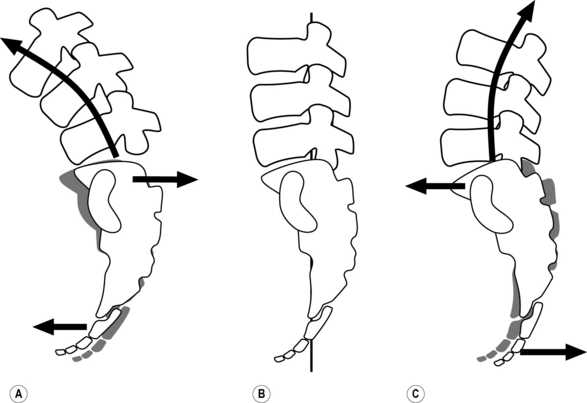
Fig. 2.9 shows how the pelvis as a unit can:
1. rotate around the 3 basic axes
2. move, or ‘translate’, along the 3 planes indicated
1. stiffness is variable between individuals, which is probably a key factor why range of motion is also likely to be variable
2. subjects with symmetrical side-to-side stiffness are more likely to be asymptomatic (no pelvic pain); whereas those with asymmetric stiffness are more likely to be symptomatic.
Most studies to date have, however, used a static approach to investigating a dynamic phenomenon. Even though studies have become increasingly refined, there is still some truth even now to the observation by Cassidy (1992) that ‘a valid and reliable method for measuring this motion in patients has not yet been developed’. Also, none of the authors cited have indicated whether or not there was malalignment of the pelvis at the time of the study, nor mentioned any particular presentation. Malalignment results in asymmetrical opposition of the SI joint surfaces and can cause unilateral SI joint hypermobility, hypomobility or even ‘locking’, all factors that would result in an asymmetry of configuration and/or mobility (see Chs 3, 4).
Axes of motion
Motion at the SI joint is complex, probably not occurring around just one fixed axis but being a movement combining rotation and translation (Beal 1982; Bernard & Cassidy 1991; Egund et al. 1978; Frigerio et al. 1974; Kissling & Jacob 1997; Walker 1992). A good description of the directions and degrees of freedom of movement at the SI joints was already found in Gray’s Anatomy in 1980 (Williams & Warwick). At risk of oversimplification, the primary motions that can occur are outlined in Box 2.1 and Figure 2.9.
Box 2.1 Axes of motion of the sacroiliac joint
Rotational movement, ‘anterior’ or ‘posterior’ around the coronal axis in the sagittal plane
1. of one or both ilia relative to the sacrum; if both rotate, this may be:
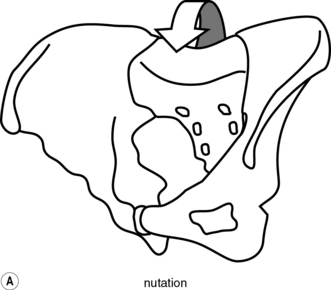
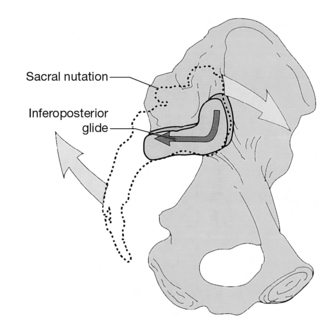
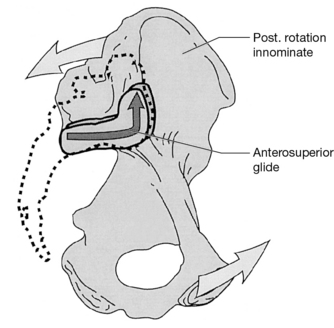
2. of the sacrum relative to both ilia; forward movement of the base has been designated as nutation and backward movement as counternutation (Figs 2.11, 2.17, 2.18, 2.19)
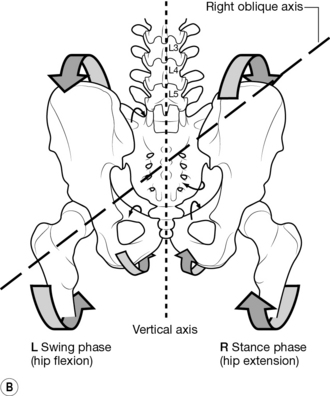
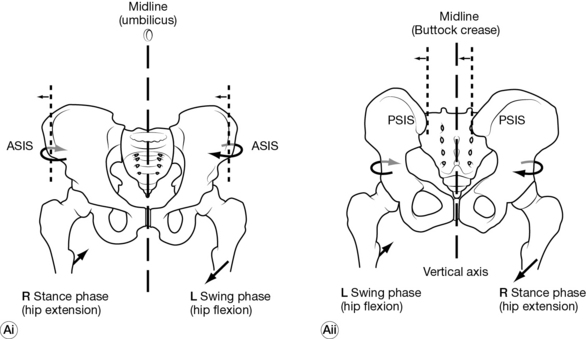
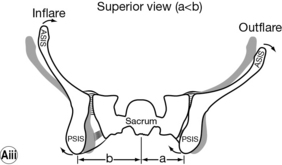
Axial rotation of sacrum and ilia in the transverse plane
1. sacrum and ilia rotating as one unit around the vertical axis
2. an ilium relative to the sacrum
3. the sacrum relative to the innominates around the vertical axis, in the transverse plane (Fig. 2.89):
Torsion of the sacrum around an oblique axis
1. torsion around the right or left oblique or ‘diagonal’ axis is one form, and usually happens in conjunction with some rotation around the vertical axis (Figs 2.14, 2.21 and Point 3 above)
2. the mean transverse axes (MTA) run from the sacral base down and over to the opposite innominate, crossing where the two parts of the L-shaped SI joint meet, at about the level of S2 (Richards 1986; Figs 2.3A, 2.10B, 2.14, 2.21, 2.42, 2.50)
3. these axes are named according to the side of origin from the sacral base (e.g. the right oblique axis starts from the right corner of the sacral base and runs downward and across to the left apex; Fig. 2.14)
Rotation and/or translation of the sacrum or an innominate results in a relative displacement of the SI joint surfaces (Figs 2.10, 2.11). Excessive rotation and/or translation in any direction can have a shearing effect. These surfaces may also become pathologically ‘stuck’ in any one position, Panjabi’s so-called ‘compressed’ joint (see ‘Kinetic function and stability’ below; Figs 2.23, 2.24). SI joint nutation makes for stability, and counternutation for instability; the amount of nutation, or counternutation, can be of a normal or pathological degree.
Muscles that can effect nutation, and increase stability, include those that can:
1. rotate the innominates posteriorly relative to the base of the sacrum (Figs 2.10, 2.21); e.g. rectus abdominis (Fig. 2.31B) and biceps femoris (Fig. 2.59)
2. rotate the sacral base anteriorly (Fig. 2.11A); e.g. semispinalis or erector spinae muscles (Figs 2.37, 2.38) and multifidi (Fig. 2.29)
Muscles that effect counternutation, and decrease stability, include those that can:
1. rotate the innominates anteriorly (Figs 2.10, 2.21); e.g. iliacus, rectus femoris and the tensor fascia lata/iliotibial band complex (Figs 2.46B,C, 2.59)
2. rotate the sacral base posteriorly (Fig. 2.11B); e.g. pubococcygeus, ischiococcygeus and iliococcygeus, all levator ani muscles originating from the pubic rami and pulling forward on the apex of the sacrum by way of their insertions into the coccyx (Fig. 2.53B)
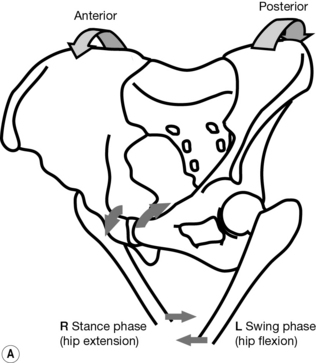
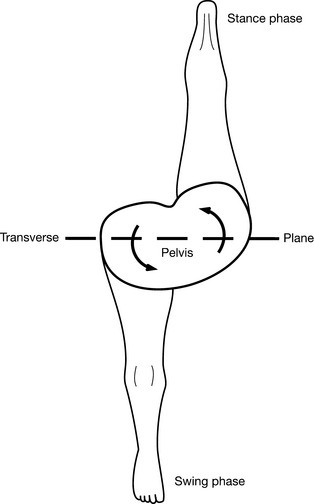
Biomechanics
Movement around the various axes of the SI joints occurs as part of normal movement patterns involving the spine, pelvis and lower extremities throughout our day-to-day activities (DonTigny 1985, Greenman 1992, 1997; Figs 2.12–2.16). The sacrum influences the relative movement of the innominates, and vice versa, as tension is increased in the connecting soft tissues – primarily ligaments and muscles – that act on the SI joint(s). This is a normal phenomenon, as described, but will be affected by the presence of tight structures; for example, a tight biceps femoris acting on an SI joint by way of its connections to the sacrotuberous ligament (Fig. 2.6). In addition, the movement is likely to be asymmetrical when such tightness is worse on one side compared to the other. When sitting, this tightness is less of a problem as the innominates are relatively ‘fixed’ and less mobile than when standing.
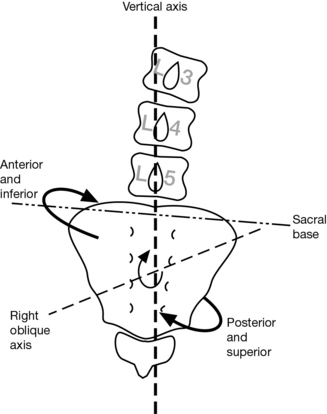
Fig. 2.14 Sacral torsion around the right oblique axis; also known as ‘right-on-right’ or R/R torsion pattern (see also Fig. 2.50)
Trunk flexion
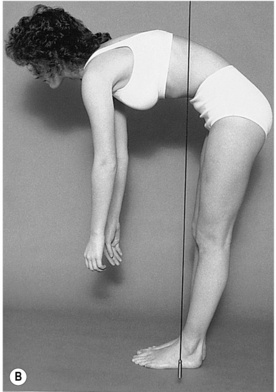
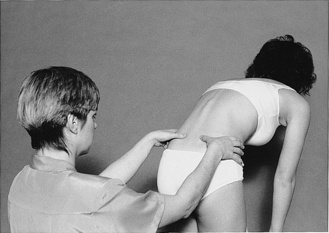
In standing
Flexion initially results in a simultaneous forward rotation of the sacrum and innominates around the coronal axis in the sagittal plane which may continue through full flexion (Kapandji 1974; Figs 2.17, 2.116A, 2.117). The right and left innominate should move an equal amount. Flexion somewhere past 50–60 degrees sees the innominates and sacrum continuing to rotate forward symmetrically in most people. In some, however, the sacrum now starts to counternutate, the base moving posteriorly and the apex (coccyx) anteriorly, decreasing the lumbosacral angle and, therefore, the lumbar lordosis (Fig. 2.18A). Counternutation from this point on may occur on account of:
1. a posteriorly directed force applied to the sacral base by the flexing lumbar spine
2. a maximal tightening of the ligaments (interosseous, sacrotuberous and sacrospinous) effected by the initial nutation (Fig. 2.19A)
3. the presence of any other factor capable of opposing the progressive nutation of the sacrum; for example, tightness of:
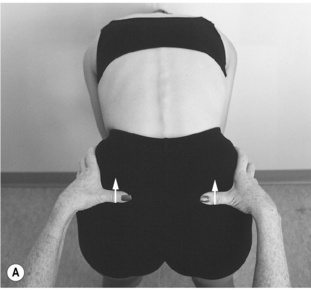

Fig. 2.116 Normal pelvic flexion/extension test. In standing (neutral position), the thumbs are on matching points – resting against the inferior aspect of the posterior superior iliac spines (PSIS; see also Fig. 2.71B). (A) On trunk flexion: the thumbs (= PSIS) move up an equal extent. (B) On trunk extension: the thumbs (= PSIS) move down an equal extent.
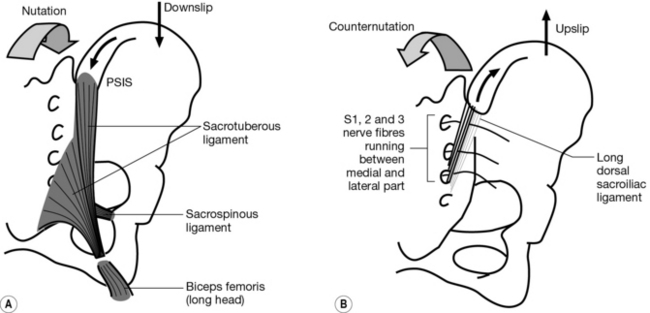
Fig. 2.19 Ligaments put under tension by the movement of an innominate or the sacrum relative to each other. (A) ‘Posterior’ rotation (= sacral nutation) and ‘downslip’ of an innominate: sacrotuberous, sacrospinous; also interosseous ligaments (not shown; see Figs 2.4B, 2.13A iii). (B) ‘Anterior’ rotation (= sacral counternutation) and ‘upslip’ of an innominate: long dorsal sacroiliac ligament.
In sitting
The initial movement on trunk flexion is one of sacral counternutation as the innominates rotate anteriorly relative to the sacrum. Counternutation increases the tension in the long dorsal sacroiliac ligament in particular, eventually resulting in posterior rotation of the innominates and sacral nutation on further trunk flexion (Figs 2.19B, 2.80B).
Trunk extension
In standing
On extension, the innominates should rotate posteriorly to an equal extent and the sacrum nutates, increasing the lumbosacral angle and hence the lumbar lordosis (Figs 2.16, 2.18C).
In sitting
Initially, the innominates do not move as the spine extends and the sacrum nutates. Once nutation has taken up all the slack in the interosseous, sacrospinous and sacrotuberous ligaments (Fig. 2.19A) and in the pelvic floor muscles and ligaments that attach to the coccyx, further extension will result in anterior rotation of the innominates (e.g. by increasing the traction force of the tight sacrotuberous ligament on the ischial tuberosity, pulling the innominate anteriorly).
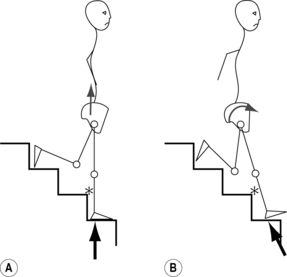
Landing on one leg
When jumping or missing a step and landing with the straight leg vertical and the foot directly underneath, the forces transmitted upward result in an ipsilateral SI joint movement consisting primarily of an upward translation of the innominate in the vertical plane relative to the sacrum (Fig. 2.20A). If there is a degree of angulation of the leg relative to the vertical axis at the moment of impact, there may be an element of anterior or posterior rotation in the sagittal plane. For example, missing the step(s) and landing with the straight leg angulated forward creates a force that can rotate the innominate anteriorly on that side, resulting in sacral counternutation and SI joint instability (Fig. 2.20B). Landing with the leg angulated backward can rotate the innominate posteriorly, resulting in sacral nutation and increasing SI joint stability. These changes are of particular importance when we come to consider the abnormal forces that can result in an ‘upslip’ and ‘rotational malalignment’ (Ch. 3). The biomechanics of standing on one leg are discussed in detail below (see ’Functional or dynamic tests’;Figs 2.121–125)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree