Chapter 30 Common Issues in Orthopedics
Fractures
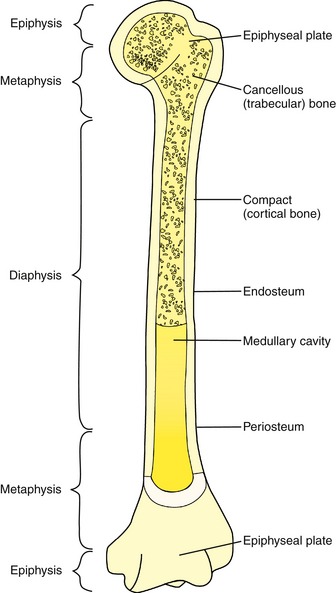
Fractures can be oriented in a variety of planes, and certain patterns are associated with greater risk of instability. Typical fracture orientations are transverse, spiral, oblique, compression, buckle, avulsion, stress, and greenstick. Additional features include the specific bone, region within the bone (diaphysis, metaphysis, epiphysis) (Fig. 30-1), and whether the fracture is complete or incomplete, open or closed, intra-articular or extra-articular, displaced or nondisplaced, angulated, shortened, or comminuted. In children, physeal involvement is a special concern.
Open fractures are surgical emergencies and require immediate irrigation and debridement, tetanus prophylaxis, and antibiotic coverage. Orthopedists typically refer to the Gustilo-Anderson classification for open fractures, which is based on the size of skin wound, soft tissue damage, and bone comminution (Box 30-1). Even a small puncture wound over a fracture may allow skin flora to infiltrate the fracture site and initiate an infection. Any open fracture warrants an immediate referral to an emergency department (ED) for orthopedic evaluation.
Box 30-1 Gustilo-Anderson Open-Fracture Classification
Growth Plate Fractures
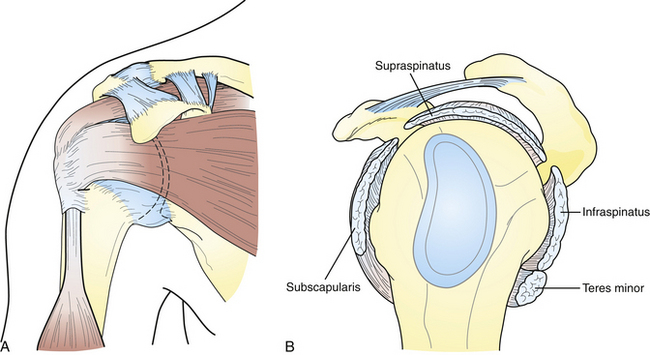
The physeal plate is a cartilaginous plate present in ends of long bones, adjacent to the metaphysis. This is the area that provides longitudinal growth to bones and eventually matures into bone. During growth, the physeal cartilaginous plate is weaker than the surrounding bone and often weaker than the ligaments and tendons that attach nearby, causing it to fracture before other areas. The Salter-Harris classification system describes these injuries (Fig. 30-2).
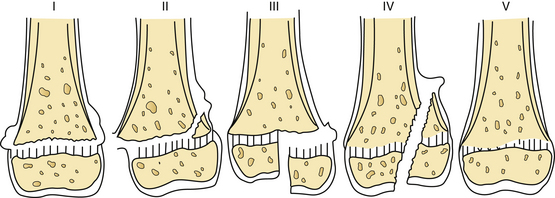
Figure 30-2 Types of growth plate injury (I to V) as classified by Salter and Harris.
(From Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg (Am) 1963;45:587.)
Salter-Harris Type IV
This intra-articular fracture pattern extends from the epiphysis, across the physeal plate, and through a portion of the metaphysis. Open reduction with internal fixation is usually needed to ensure anatomic alignment of the joint surface and perfect alignment and apposition of the physeal plate. Premature growth arrest and angular deformities can occur with Salter-Harris IV fractures. Prognosis can be good but depends on ability to restore growth plate.
Shoulder
Injuries of Clavicular Complex
Clavicle fractures account for 5% to 10% of all fractures and can be classified as either displaced or nondisplaced as well as by their specific location (proximal-distal) on the clavicle. Most fractures involve the midshaft (80%); however, distal third (15%) and proximal third (5%) fractures are also possible. Fortunately, most clavicle fractures can be definitively treated nonoperatively with a sling or a figure-of-8 dressing if they are minimally displaced or nondisplaced. Figure-of-8 bracing has been linked with skin necrosis over the fracture site, indicating the need for careful observation of skin integrity when used. In most cases, a simple sling for comfort is adequate over the first few weeks, followed by progressive range of motion (ROM) activities. More significant displacement (>100%), any tenting of the skin, significant comminution, or excessive shortening (>2 cm) may warrant surgical intervention, and referral to an orthopedist is recommended. Distal clavicle fractures have a higher rate of nonunion with nonsurgical treatment than midshaft or medial fracture patterns, so careful follow-up is necessary (Kahn et al., 2009; McKee et al., 2004).
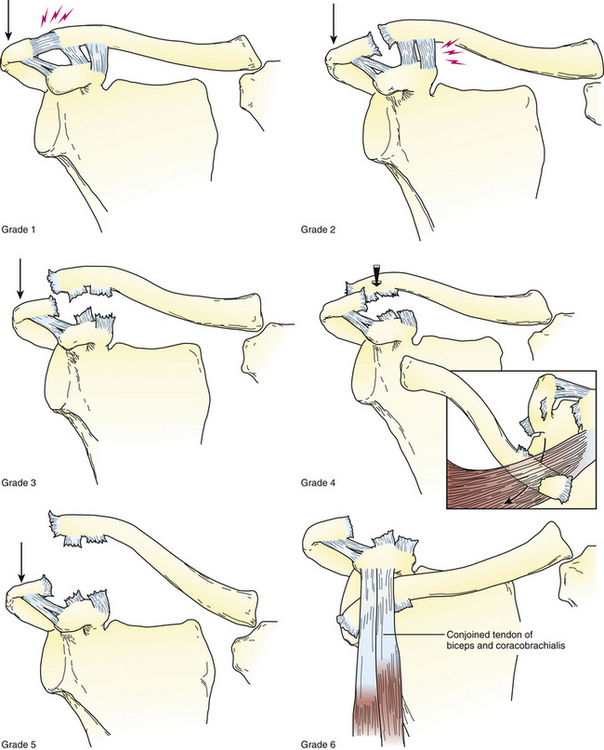
Acromioclavicular Joint
Acromioclavicular (AC) joint injuries are classified by the ligamentous structures involved and the degree of separation of the AC joint (Fig. 30-3). A grade 1 injury involves only a partial injury to the AC ligaments, no displacement occurs, and the coracoclavicular (CC) ligaments are intact. A grade 2 injury involves the complete injury of the AC ligaments, and therefore mild superior translation of the distal clavicle occurs (<100% translation), and CC ligaments are intact. Both grade 1 and grade 2 injuries have an excellent prognosis with conservative treatment, which includes local application of ice, reduction of stresses, and a sling for comfort. Most patients will have substantial active motion and functional use of the arm within 6 weeks. A grade 3 involves the complete rupture of both AC and CC ligaments. The distal end of the clavicle and acromion are now separated by more than a full clavicular width (>100% displacement). Stress radiographic views may magnify this separation even further; however, stress views rarely alter the treatment plan and are painful to patients and thus no longer considered required diagnostic images.
Sternoclavicular Joint
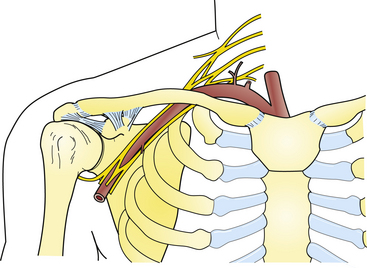
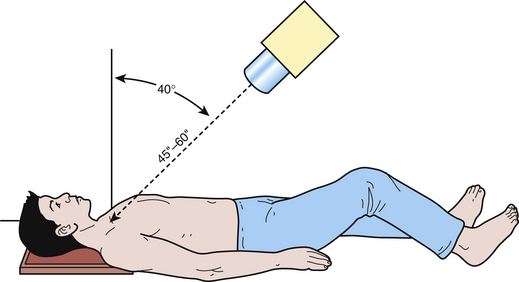
Patient with sternoclavicular (SC) injuries present with a history of trauma (e.g., landing on lateral aspect of shoulder) or a history of chronic overuse that has led to popping and pain over the medial aspect of the clavicle (Matave et al., 2005). Acute SC joint dislocations can be identified clinically with localized tenderness over the medial clavicular aspect, and gross deformity may be present. More often, however, patients present with a subtle chronic situation caused by esthetic findings with a palpable or gross asymmetry. The examination should always include an assessment of the patient’s airway and circulation, including cervical venous distention, because the great vessels and trachea lie immediately posterior to the SC joints (Fig. 30-4). Imaging studies should include an AP radiograph of the chest, views of the entire clavicle, and a tangential or serendipity view of the SC joint (Fig. 30-5). Because of overlapping shadows, these studies may be difficult to interpret. When suspicious, the best test is computed tomography (CT).
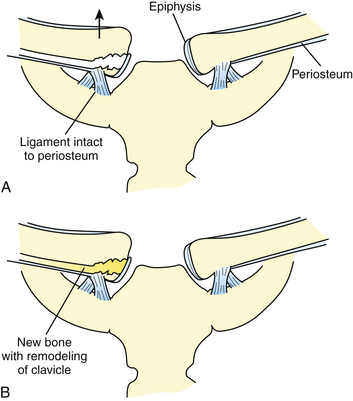
When treating injuries to the proximal clavicle, age of the patient and normal maturation of the proximal epiphysis are also important considerations. The medial clavicle epiphysis is one of the last to appear, at 19 to 23 years of age, and then the last to fuse, at 23 to 25 years of age. In patients younger than 23, these injuries are generally physeal injuries and not true dislocations, reducing the need for aggressive treatment (Fig. 30-6).
KEY TREATMENT
Shoulder Impingement and Rotator Cuff Disease
By far the two most common diagnostic categories about the shoulder are rotator cuff impingement and shoulder instability. The rotator cuff is a group of four muscles—supraspinatus, infraspinatus, teres minor, and subscapularis—that originate from the scapular surface, traverse just outside of the glenohumeral capsule, and insert onto the tuberosities of the humerus (Fig. 30-7). The rotator cuff initiates motion in the shoulder and stabilizes the humeral head in the glenohumeral joint.
The diagnosis of rotator cuff impingement is actually a continuum of pathologies, including subacromial bursitis, AC joint hypertrophy and spurring, rotator cuff tendinosis, partial rotator cuff tears, complete or massive rotator cuff tears, and ultimately, rotator cuff arthropathy; that is, degenerative disease related to chronic rotator cuff insufficiency (Almekinders, 2001). Patients generally present with shoulder pain exacerbated by repetitive overhead activities, perhaps weakness, and occasionally difficulty sleeping on the shoulder. Physical examination of the shoulder includes provocative maneuvers that exacerbate impingement findings and evaluate the function of each rotator cuff muscle (Tennent et al., 2003a, 2003b). Impingement testing includes straight, forward flexion of the shoulder (Neer sign), abduction and internal rotation of the shoulder (Hawkins sign), and adduction of the shoulder in a 90-degree, forward-flexed position (Figs. 30-8 and 30-9). The examiner must be cautious with the latter test because it may be positive with impingement but also with AC joint hypertrophy alone or with degenerative change of the AC joint.
To evaluate the infraspinatus and teres minor muscles, the examiner should evaluate external rotation against resistance. This is best done with the arm at the side, keeping the elbows near the torso, and asking the patient to rotate externally against resistance. Isolating the subscapularis muscle is more difficult. Resisted internal rotation with the arms at the side will recruit the pectoralis muscles and not isolate the subscapularis. To isolate the subscapularis, two tests have been described. In the lift-off test, the patient places the arm behind the back and lifts the hand into further internal rotation against resistance (Fig. 30-10). If able to do this, the patient’s subscapularis muscle is likely intact. Modification of this test has been described as the “tummy pat” or the “Napoleon” test, in which the patient abducts the elbow, which must be away from the body in the plane of the torso, and is then asked to pat the stomach against resistance (Fig. 30-11). Weakness or inability to press against resistance is considered to be a positive test. Once the diagnosis is made clinically, AP and axillary shoulder x-ray studies can be obtained to evaluate the extent of injury further or assess for concomitant injuries. MRI is not routinely indicated with an intact rotator cuff clinically, and we usually recommend trying a course of physical therapy for 6 to 12 weeks before ordering MRI (Park et al., 2005).
For incomplete rotator cuff tears (<50% of surface), a partial debridement and subacromial decompression using arthroscopy can provide effective, long-term relief of impingement pain. Management of rotator cuff tears greater than 50% or complete with clinical dysfunction is generally surgical. If the tear is identified before chronic retraction and muscle changes, primary arthroscopic or open repair has been effective in reducing pain and improving function. Rehabilitation after rotator cuff repair requires at least 6 weeks of passive ROM only, to protect the repair, followed by a gradual increase to resistance activities for the rotator cuff. Patients usually begin strengthening at 12 weeks. In patients with nonreparable chronic rotator cuff tears or those with advanced rotator arthropathy and degenerative disease, surgical interventions include muscle transfers, soft tissue grafts, hemiarthroplasties, and reverse shoulder hemiarthroplasties.
EVIDENCE-BASED SUMMARY
Shoulder Instability
The diagnosis of shoulder instability begins with the patient’s history and mechanism of injury, which often include episodes of subluxation, dislocation, or apprehension. Classically, anterior instability is appreciated when the arm is placed in abduction and external rotation (Tennent et al., 2003a, 2003b) (Fig. 30-12). Inferior instability is appreciated when the patient tries to hold a heavy object and the shoulder subluxes inferiorly. Posterior instability is frequently associated with a fall on an outstretched arm, or occasionally with weightlifters who lock out their arms in extension while bench pressing. The clinical examination targets these specific pathologies with the classic apprehension test for anterior instability, performed with the arm in abduction and external rotation, and the patient having the sensation of the arm going out of place. In the relocation test the examiner then presses the humeral head back into a reduced position, thus eliminating the sensation of apprehension. Posterior instability is assessed in a supine position with the arm forward-flexed 90 degrees with a posteriorly directed force. Inferior instability is assessed by pulling inferiorly on the arm and looking for or feeling the humerus come out the socket and looking for a concavity just below the acromion, called the “sulcus sign” (Fig. 30-13).
The conservative treatment of shoulder instability is targeted at balancing the flexibility, optimizing the motor strength, and optimizing the function of the kinetic chain. The core component is rotator cuff–strengthening exercises as well as scapular stabilizer exercises. Controversy surrounds the ideal treatment for a first-time shoulder anterior dislocation. In young athletes or military populations, the risk of recurrence and future shoulder problems approaches 90%. Surgical treatment with repair of labral detachments has led to a high rate of return to play and return to performance, with a low risk (<10%) of recurrent instability for a first dislocation. Older nonathletic patients (>40) with first-time dislocation have a reduced risk of recurrent instability (<50%), so surgical treatment is unnecessary. However, if any patient has recurrent instability or pain, surgery to repair the torn capsule or labral lesions is strongly recommended, with outcomes ranging from 75% to 95% good to excellent results. The Bankart procedure is most often performed and involves direct repair of the torn labrum back to the glenoid from which it was detached (Fig. 30-14). Classically, this procedure was performed open, although the current trend is toward arthroscopic assistance.
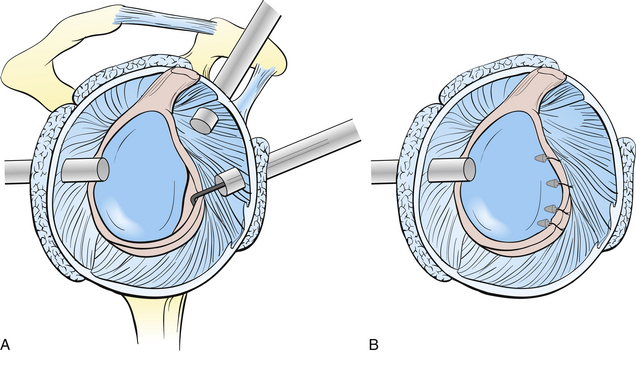
Figure 30-14 A, Detachment of the anterior inferior labrum (a Bankart lesion). B, Subsequent suture repair.
KEY TREATMENT
Elbow
Lateral Elbow Tendinopathy
Counterforce straps can effectively reduce discomfort in some patients (Fig. 30-15). The strap is applied just distal to the area of maximal tenderness. The strap may relieve some of the tension exerted on the affected muscle tendon units during activities, thereby reducing pain. However, straps, medications, and injections should not replace therapeutic exercises, which include massage, stretching, and strengthening exercises. The most effective stretch is performed with the elbow extended, forearm fully pronated, and wrist flexed. From this position, gentle traction is applied to the middle and ring fingers toward the olecranon. Strengthening exercises with light weights for wrist extension and forearm supination can be done.
Most patients with lateral elbow tendinopathy will obtain excellent relief of symptoms with the program just described, although minimal evidence exists to support these plans (Bissett et al., 2005). If these measures do not lead to adequate relief, other protocols can be added. Formal physical therapy is often used in recalcitrant cases. Treatments such as prolotherapy, dry needling, platelet-rich plasma injections, and extracorporeal shock wave therapy are still experimental, and studies have not fully proved their effectiveness. Surgical intervention is sometimes needed and has excellent results.
KEY TREATMENT
Medial Elbow Tendinopathy
Medial elbow tendinopathy or medial epicondylitis, commonly called “golfer’s elbow,” is caused by repetitive overuse of the wrist flexor and forearm pronator muscles that originate at the medial epicondyle of the humerus. Patients present due to pain in the medial aspect of the elbow, rarely weakness, and loss ROM. Pain is worsened by gripping and lifting activities, particularly with the hand in palm-up position. Common positive findings include tenderness to palpation of the medial epicondyle of the elbow and over the proximal wrist flexor and forearm pronator muscle tendons. Pain is intensified with resisted wrist flexion and forearm pronation (Fig. 30-16). Patient discomfort often limits strength. Elbow motion, ligamentous stability, and neurovascular status are typically intact.
Olecranon Bursitis
Olecranon bursitis is a common cause of painless elbow swelling from repetitive friction of the olecranon against a firm surface or traumatic impact. Patients most often present with a painless swelling at the dorsal tip of the elbow, described as “a golf ball” or “goose egg” (Fig. 30-17). With trauma-induced swelling, pain and a hematoma may be present. Pain, redness, warmth, and lymphadenopathy may accompany septic bursitis. ROM loss, instability, neurovascular compromise, and strength loss are uncommon. On examination, there is a soft, fluctuant area of swelling directly over the olecranon. Diagnostic studies are generally not necessary to make a diagnosis of olecranon bursitis. However, plain radiographs should be obtained if trauma preceded the bursitis or fracture or dislocation is suspected.
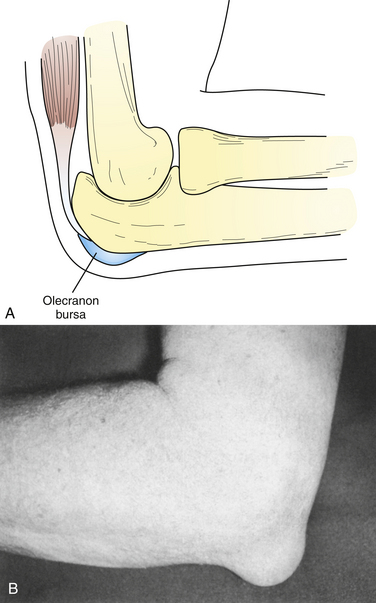
Figure 30-17 A, Relation of the olecranon bursa to the skin and olecranon. B, Photograph of an enlarged olecranon bursa.
(From Singer KM, Butters KP: Olecranon bursitis. In Delee JC, Drez D [eds]. Orthopedic Sports Medicine: Principles and Practice, vol 1. Philadelphia, Saunders, 1994, pp 890, 892.)
Treatment includes compression, ice, and avoidance of impact at the olecranon. NSAIDs may help to reduce swelling. If the fluid collection is large or infection is suspected, aspiration of the bursa can be done in the office with a large-bore needle under sterile conditions. The bursa fluid should be clear and straw colored but may be bloody in a traumatic injury. If an infection is not suspected clinically once the fluid is withdrawn, a corticosteroid can be injected. Corticosteroids should never be injected if infection is a possibility. Oral antibiotics can be started if an infection is present. A local incision and drainage (I&D) may be required in the presence of an infection and abscess. Aspiration does not replace compression wrap, ice, and avoidance of impact. Fluid may reaccumulate but should decrease. Serial aspirations are an option in a recurrent aseptic bursitis, but bursectomy is occasionally needed for definitive treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree