Fig. 13.1
Position of the patient for a PCL surgery. Left leg holder giving room to work through the posteromedial portal
In these cases we use pneumatic tourniquet. If the surgery takes over 100 min, it is necessary to discontinue the pneumatic tourniquet for 20 min and then use it again. Concerning the portals, we usually use 3: anterolateral, anteromedial, and posteromedial.
The first step is to perform the PCL arthroscopic reconstruction and afterward the medial reconstruction in the same surgical time.
After examining and treating meniscal and cartilage lesions of the medial, lateral, and patellofemoral compartments, we perform the PCL femoral anatomic tunnel inside out.
If patient has an intact band or a remnant of PCL, we always preserve it and perform an augmentation.
We use a femoral aimer (through the anterolateral portal) to place the exact anatomic tunnel position of the ligament, and we check the pin position through the same portal to be sure of the correct position. We try to reconstruct the AL band (Fig. 13.2a).
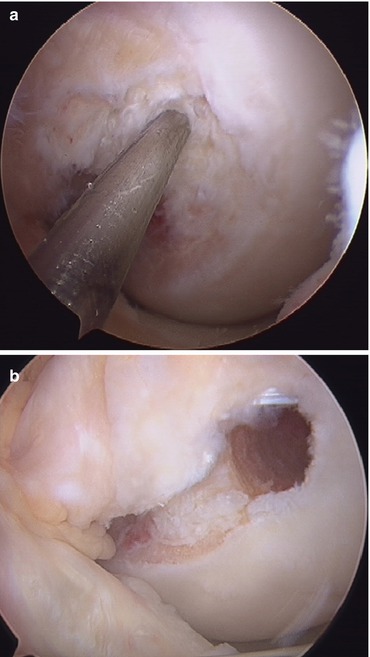
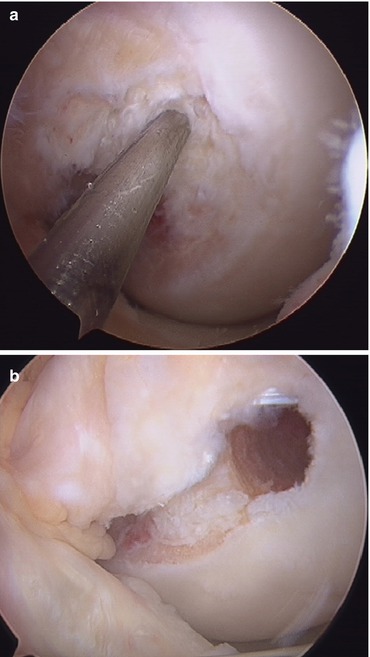
Fig. 13.2
(a) Guide pin in PM femoral bundle location for an augmentation procedure. (b) Bleeding bone bed in the outer wall of the medial femoral condyle for the PCL graft. Right knee
Regarding femoral tunnel size, for PCL we use a length of 25 mm and the width is the same as the graft, usually 8–9 mm.
Then with a shaver or rasp, we make a bleeding bone bed in the medial notch where the PCL graft will be placed (Fig. 13.2b).
When we have the PCL femoral tunnel ready, we perform the posteromedial portal and insert an 8 mm cannula in. And then we begin to clean the posterior tibia with a shaver or radiofrequency. We try to expose 20 mm of the posterior tibia to be able to locate the PCL guide easily. It is very useful to have a reliable and accurate PCL guide and curved curettes to protect the pin exit not to damage the knee posterior structures. It is a very good maneuver to use a curved rasp to make a bleeding bone bed in the posterior tibia where the PCL graft will lay. We use a guide that marks how deep we are in the posterior tibia, and as the tip guide is wide, it stops the pin from going farther and damaging the posterior neurovascular structures. For greater safety we can also use a special device with the guide so as to keep the pin from going further than the guide tip.
We raise the PCL graft through the tibial tunnel to the femur. It is very useful to have some malleable material as a plastic with a hole in both ends to do it (Fig. 13.3). To help the advancement of the graft, we use the trocar of the scope through the posteromedial portal as a pulley. In the proximal PCL graft, we make a suture with 2 cm baseball stitches for better screw fixation. We fix the proximal end of the graft with a 7 and 25 mm interferential BioScrew with the knee in 90°. Lastly we fix the distal PCL graft with a BioScrew which is one or two numbers higher than the graft and 30 mm long; the knee must be in 90° flexion with an antepulsion of the calf (because we are reconstructing the AL band).
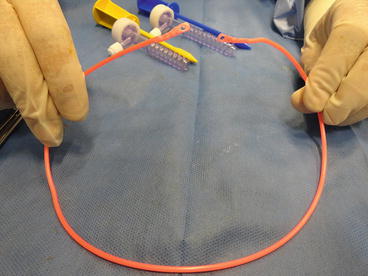
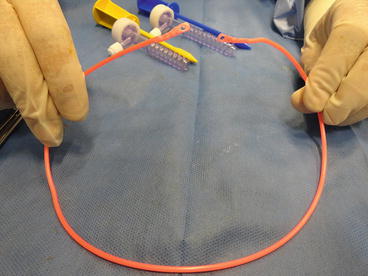
Fig. 13.3
Homemade plastic device to raise the PCL graft
Concerning medial or posteromedial instability, we prefer to reconstruct the sMCL and the POL. In cases when the patient has no posteromedial instability, we only perform the sMCL.
As regards posteromedial instability, we perform only one tunnel in the femur, 0.5 mm posterior and 0.5 mm proximal to the medial epicondyle [12], for proximal insertion of the sMCL and POL. The tunnel diameter size depends on the graft (usually 8 or 9 mm for a double anterior tibial allograft), but its length is always 30 mm. The proximal skin incision is approximately 20 mm long.
In tibia, for the sMCL we perform a tunnel in the anterior face of the tibia 60 mm distal to the knee joint line whose size depends on the graft (single anterior tibial allograft) and which runs through the whole tibia. For the POL we insert a 5 mm bioabsorbable anchor, with 2 sutures, 15 mm distal to the knee joint line and as far back as possible from the tibial anterior face. The distal skin incision depends on the patient, but if we have harvested hamstring tendons for the PCL, we use an oblique incision of 30–50 mm for the entire procedure.
We pass the graft underneath the semimembranosus attached to the periosteum.
In the femur, we fix the graft with an interferential BioScrew, which has the same diameter as the tunnel and is 30 mm long. We fix the sMCL with a 25 mm long BioScrew in 30° of knee flexion, respecting the same diameter as the tunnel, and if necessary, we add a staple. The last fixation is the distal POL, in full extension with the two reinforced sutures of the anchor (Fig. 13.4).


Fig. 13.4
Final reconstruction of the sMCL and POL. Right knee
Post-op
Immobilization should be in full extension, with a brace and partial weight bearing using crutches 6–8 weeks.
13.3.2 Posterior and Lateral or Posterolateral Instability
The posterolateral corner is a complex structure which contributes to knee stability.
The most important structures are the lateral collateral ligament (LCL) or fibular collateral ligament, the popliteus tendon, the popliteus fibular ligament (PFL), and the posterolateral capsule [13, 14].
A specific maneuver to assess posterolateral instability is varus stress in full extension and in 30° of knee flexion.
Others are dial test, posterolateral drawer test, recurvatum test, and inverse pivot shift test. It is always advisable to perform them bilaterally. If in the dial test the comparative external rotation is higher than 10°, in 30° and 90°, it shows that PCL and posterolateral structures are torn. But if in 90° the difference is lower than 10°, it shows that the PCL is intact.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








