Combined Ligament Injuries of The Knee: Anterior Cruciate Ligament/Posterolateral Corner and Medial Collateral Ligament/Posterior Cruciate Ligament: Diagnosis, Treatment, and Rehabilitation
Mark McCarthy
Lawrence Camarda
Jill Monson
Robert F. LaPrade
Multiligament knee injuries present challenging scenarios for orthopedic surgeons. Advanced physical exam skills are required to focus in on specific ligamentous structures, followed by radiographic imaging that can be complicated to evaluate. The decision to operate or to treat conservatively requires advanced knowledge of classification systems and applying them to tailor to each individual patient. The surgical procedures themselves are technically challenging and demand precision. Finally, the surgeon and patient must be prepared for a long rehabilitation process and treat any complications that may arise. This chapter is designed to be an outline to diagnose and treat two specific patterns of multiligament knee injuries: the anterior cruciate ligament (ACL)/posterolateral corner (PLC) and the medial collateral ligament (MCL)/posterior cruciate ligament (PCL).
ACL/PLC INJURIES
Introduction
PLC injuries are challenging to diagnose and treat. When faced in clinical practice with an acute knee injury, it is vital to keep injuries to the PLC structures in mind throughout the patient encounter. It is well known that injuries to the ACL are common. However, it has also been reported that ACL tears occur, quite commonly, as part of a multiple ligament injury pattern (1, 2). The section of the chapter is dedicated to give hints on the history and physical exam to heighten a clinician’s awareness of a possible underlying PLC injury in the setting of an ACL tear, as well as imaging and treatment options of this difficult injury pattern.
Clinical Evaluation
History
Most PLC injuries occur in the setting of other ligament injuries, with the ACL/PLC combination being one of the most common patterns (2). The mechanism of injury is often a hyperextension varus injury (a blow to the anteromedial knee). Patients will often report a sense of instability with everyday activities, especially for positions where the injured knee is in extension. In addition, a thorough history should include questions regarding the functioning of the common peroneal nerve, both for sensation and for motor function, because the literature has reported a 15% incidence of concomitant common peroneal nerve injuries with PLC injuries (2). Any reported numbness, tingling, or weakness with ankle dorsiflexion and/or great toe extension should be dutifully noted.
Physical Exam
After inspecting and palpating the knee for an effusion and tenderness, a focused knee exam to assess its stability should be performed. A straightforward initial test is the external rotation recurvatum test (3). With the patient supine, the clinician lifts the lower extremity by the patient’s great toe, with the other hand holding the patient’s thigh as needed to assess for knee hyperextension. Increased recurvatum, or hyperextension, often indicates a severe multiligament injury, often involving the ACL, but is also seen when both cruciate ligaments are injured and/or a disruption of the PLC structures exists. In one study of 134 consecutive patients with posterolateral knee injuries, 10 patients demonstrated a positive external rotation recurvatum test. All 10 of these
patients had a combined ACL/PLC injury pattern (3). Further, this same study found that 30% of patients with a combined ACL/PLC insufficiency pattern had a positive external recurvatum test. When comparing with the contralateral normal lower extremity, measurements can be taken based on increased heel height differences of the affected leg.
patients had a combined ACL/PLC injury pattern (3). Further, this same study found that 30% of patients with a combined ACL/PLC insufficiency pattern had a positive external recurvatum test. When comparing with the contralateral normal lower extremity, measurements can be taken based on increased heel height differences of the affected leg.
To further specifically assess the PLC, it is helpful to perform the varus stress test, both at 0° and at 30° of knee flexion. To most accurately define the amount of abnormal motion due to injury, the test is best done at 0° by stabilization of the thigh against the examining table and then applying a varus force across the knee by grasping the foot or ankle. At 30°, the leg can be brought over the side of the exam table, with the thigh again stabilized against the table, and a varus force applied (Fig. 77.1). The contralateral knee must be examined to assess for any physiologic varus laxity. The clinician’s fingers should be placed at the lateral joint line to estimate the amount of lateral joint space opening. Injuries are graded 1, 2, and 3 based on lateral compartment gapping in millimeters, progressing from lower grades indicating partial tears to higher grades that often indicate complete tears of posterolateral structures. To quantify this more accurately, an in vitro study in which PLC structures were sequentially sectioned was performed to simulate isolated PLC injuries and combined cruciate ligament injuries. When an isolated fibular collateral ligament injury was simulated, the average increase in lateral joint space opening with an applied varus stress was 2.7 mm. This increased to 4.0 mm for grade 3 PLC injuries (4). A positive varus stress test at 0° often implies a severe PLC injury in addition to a cruciate ligament injury because the stabilizing effect of the cruciates in full extension is lost.
To assess the integrity of the ACL, the Lachman test is performed with the knee in 15° to 25° of flexion. ACL tears are graded as mild, moderate, and severe based on the approximate displacement found and, again, compared with the contralateral knee. When combined with a PLC injury, the Lachman test becomes more pronounced, both in reproducible displacement and in relative instability. A pivot shift test can be performed as well, with greater subluxation often indicating a possible combined posterolateral knee injury and ACL tear. Here, the clinician loads the leg with an axial/valgus force. As the knee is brought from extension to flexion, the subluxed knee undergoes reduction due to the stabilizing effect of the iliotibial band at approximately 20° to 30° of knee flexion.
The posterolateral drawer test is helpful to establish the amount of posterolateral rotation of the knee. Like the posterior drawer test, the knee is not only flexed to 90° but also externally rotated approximately 15° to better isolate the popliteus complex. Increased posterolateral rotation compared with the other knee is often seen with popliteus complex injuries. As an adjunct to the posterolateral drawer test, the reverse pivot shift test, which is basically a dynamic posterolateral drawer test, can be performed as well. Here, the knee is flexed to approximately 45°, with a valgus stress applied as the knee is brought out into extension. For a positive test, the knee sits subluxed in flexion and is reduced by the iliotibial band at around 30°.
The dial test, or tibial external rotation test, is done at 30° and 90° of knee flexion with the patient either prone or supine (5). While stabilizing the thigh, the lower leg is externally rotated at both positions (Fig. 77.2). Increased external rotation of at least 15° at 30° of knee flexion compared with the normal contralateral knee indicates a severe PLC injury. If this injury is an isolated PLC injury, the external rotation should decrease to about 5° at 90° of knee flexion. If the amount of external rotation at 90° of knee flexion remains around 15°, a combined PCL/PLC injury pattern is likely.
Imaging
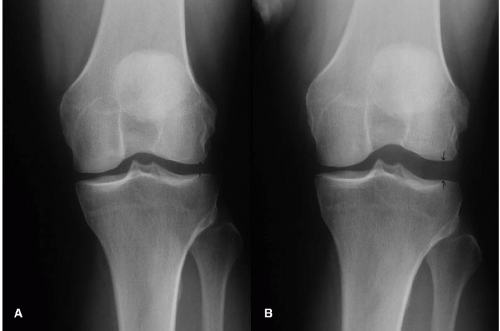
Radiographic images are necessary to precisely define the injury pattern and assist in preoperative planning. Some nonspecific X-ray findings that suggest a PLC injury include a Segond fracture, or bony avulsion of the capsule from the mid-third lateral tibial plateau. Also, an arcuate fracture,
an avulsion of the fibular head, and styloid at the attachment sites of the PLC structures are best viewed on plain radiographs, whereas the associated ligaments attached to the avulsion fracture, however, are best viewed on coronal and sagittal MRI images (6). Varus stress X-rays at 20° of knee flexion can be performed to more accurately assess lateral joint space gapping (Fig. 77.3). To reiterate, gapping greater than 4 mm has been found to correlate with grade 3 PLC injuries (4). Although X-rays are an appropriate imaging study to begin the radiographic assessment, the preferred imaging modality for acute injuries is an MRI.
an avulsion of the fibular head, and styloid at the attachment sites of the PLC structures are best viewed on plain radiographs, whereas the associated ligaments attached to the avulsion fracture, however, are best viewed on coronal and sagittal MRI images (6). Varus stress X-rays at 20° of knee flexion can be performed to more accurately assess lateral joint space gapping (Fig. 77.3). To reiterate, gapping greater than 4 mm has been found to correlate with grade 3 PLC injuries (4). Although X-rays are an appropriate imaging study to begin the radiographic assessment, the preferred imaging modality for acute injuries is an MRI.
 FIGURE 77.2. Dial test at 30°: Excess external rotation observed, indicating severe PLC injury and high likelihood of multiligament involvement. |
MRI has been proven to consistently identify specific PLC structures and also injuries to these structures (6) This is a pivotal aspect of each clinician’s diagnostic workup. In an acutely injured knee, it may be challenging, even impossible, to reliably diagnose PLC structure injuries due to patient guarding and other associated injuries. This is critical in operative planning, not only because of the high incidence of concurrent ACL/PLC injuries (1, 2) but also because reconstructing one’s ACL without recognition of PLC structure insufficiency is a known cause of ACL graft failure (7).
Decision Making
Once a diagnosis has been made, treatment thereafter is largely based on a few general principles. The severity of the injury, as delineated by the grading system described below, is a major component in deciding to pursue an operative or nonoperative treatment plan. Grade 1 and 2 injuries are typically treated nonoperatively, as described below.
If a surgical intervention is deemed appropriate, the timing of that surgery based on the date of injury becomes important. For injuries less than 3 weeks old (acute injuries), primary repair of the PLC structures is recommended if possible. When injuries have occurred longer than 2 months from the time of surgery (chronic injuries), it is appropriate to perform an anatomic reconstruction. Again, in the setting of a combined ACL/PLC injury, it is necessary to reconstruct the ACL in combination with the PLC for a better functional outcome. Should the chronic PLC injury be present with a combined genu varus malalignment, the patient should undergo a valgus-producing, openingwedge high-tibial osteotomy prior to PLC reconstruction.
Classification
PLC injuries are typically graded 1, 2, and 3. Grade 1 injuries have minimal disruption of the PLC structures and are not associated with significant increases in abnormal joint movement. Grade 2 injuries have partial tearing and moderate abnormal joint motion. Grade 3 PLC injuries are associated with complete disruption of PLC structures and markedly abnormal joint movement (8). To further quantify ligamentous laxity, some authors describe using 1+, 2+, and 3+ in regard to instability of the PLC, (9) along with varus joint space gapping, described above (3) The treatment of these injuries based on their grade is discussed in the next section.
Treatment
Nonoperative Treatment
It is recommended to treat grade 1 and 2 PLC injuries nonoperatively initially. Studies have found this to yield good results. One study had seven patients diagnosed
with 1+ varus instability who were treated nonoperatively. Six of those patients were completely stable on follow-up, with one, treated with a plaster cast, having persistent 1+ varus instability (10). In another study, 11 patients with grade 2 PLC injuries treated nonoperatively were analyzed at an average follow-up of 8 years and had good results (11).
with 1+ varus instability who were treated nonoperatively. Six of those patients were completely stable on follow-up, with one, treated with a plaster cast, having persistent 1+ varus instability (10). In another study, 11 patients with grade 2 PLC injuries treated nonoperatively were analyzed at an average follow-up of 8 years and had good results (11).
For nonoperative treatment, the patient is placed into a knee immobilizer in full extension for 3 to 4 weeks with no knee motion permitted. The patient is instructed on performing quadriceps sets and straight leg raises in the immobilizer. Further more, strict nonweight-bearing status is kept during this period. Thereafter, the patient begins range of motion (ROM) and weight bearing as tolerated. Once patients can ambulate without a limp, they may be off crutches. For 6 to 10 weeks, patients are not allowed any active hamstring exercises. Closed-chain quadriceps exercises are allowed during this time. It is important to remember that this treatment plan only concerns conservative management of the PLC structures. In cases of concomitant ACL insufficiency, it is recommended to perform a reconstruction to achieve better stability.
Special circumstances arise when treating highly trained athletes with grade 1 or 2 PLC injuries. For these athletes, a medial compartment unloader brace can be used to allow them to return to competition sooner. In these conditions, they are required to wear the unloader brace at all times except to shower. In most cases, athletes are able to return to competition within 2 to 3 weeks. Varus stress radiographs are necessary in following these patients to verify that the partially torn Fibular collated ligament (FCL) does not stretch out with this program.
Operative Treatment
Acute injury operative treatment
Acute primary repair of the PLC should be performed within the first 2 weeks following the injury. Once past 3 weeks from the injurious event, it has been found that significant scar tissue planes develop within the posterolateral knee, tissues become retracted, and tissues no longer hold sutures well (5).
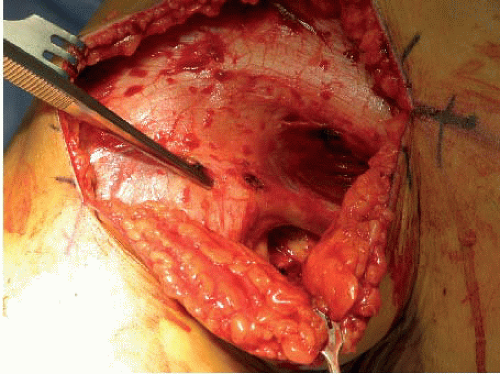
The PLC of the knee can be adequately exposed through a lateral hockey-stick-shaped (Fig. 77.4), straight, or curvilinear incision (12) Major structures such as the biceps femoris (Fig. 77.5), iliotibial band, FCL, Popliteofibular ligament (PFL), and the popliteus tendon should be identified and evaluated. The common peroneal nerve should be identified and a neurolysis should be performed (Fig. 77.6). Repair of the injured structures proceeds from deep to superficial. Anatomic repair of soft-tissue avulsions from bone should be attempted through direct suture, suture anchors, and interference screws. If the severity of the injury precludes a direct repair, the involved structure can be augmented with a hamstring tendon, a portion of the biceps femoris tendon or iliotibial band, or reconstructed with an anatomic FCL or PLC reconstruction (5).
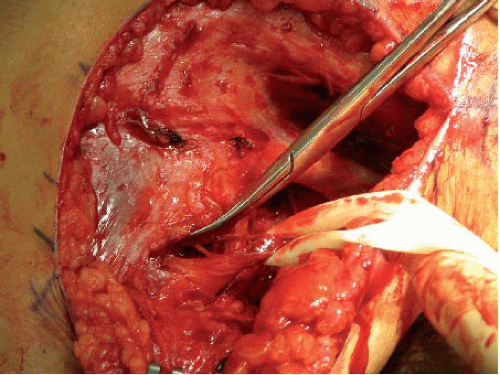 FIGURE 77.6. Common peroneal nerve isolated, protected with Penrose drain.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|