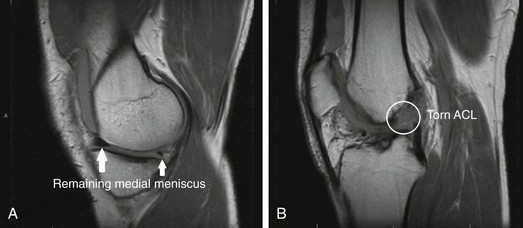
Chapter 61 The menisci play a crucial role in maintaining the structure and function of the normal knee. They contribute to shock absorption, joint lubrication, knee stabilization, proprioception, and load sharing.1–3 These roles are significant in protecting the articular cartilage. For example, the medial meniscus carries up to 50% of the load in the medial compartment when the knee is extended.4 Fairbank showed significant changes in the knee joint after medial and lateral meniscectomies.5 Although chondral changes occur more rapidly after lateral meniscectomies, medial meniscectomy more predictably results in degeneration within the knee.5,6 These findings lead surgeons toward meniscal-preserving treatments whenever possible.7 Unfortunately, in certain patients meniscal pathology may be severe enough to necessitate subtotal or total meniscectomy to appropriately address a patient’s symptoms. The progression toward degeneration in postmeniscectomy knees is accelerated with an associated injury to the anterior cruciate ligament (ACL).8,9 In addition, the results of ACL reconstruction in knees with medial meniscal deficiency are usually worse than in knees with an intact medial meniscus.10 Thus, the menisci and ACL likely play a synergistic role in preserving knee stability. The medial meniscus acts as a secondary stabilizer to anterior tibial translation. Medial meniscectomy in the ACL-deficient knee increases anterior tibial translation by 58% to 90%.3 With ACL deficiency, forces in the medial meniscus increase from 52% to 197%.11 In addition, a combined ACL and medial meniscal deficiency results in anteromedial rotatory instability of the knee. For this combined deficiency, performance of meniscal allograft transplantation combined with ACL reconstruction has been advocated to diminish pain, to improve knee stability and function, and to delay degenerative changes in the knee. We present our preferred technique to address this challenging condition as well as our clinical outcomes. The physical examination should begin with inspection to document the presence of an effusion or visible swelling, trauma, or skin compromise. Next, the range of motion and strength are documented. The patient’s stance, gait pattern, and overall limb alignment should be evaluated and compared with the contralateral side. Joint line tenderness and degree of quadriceps atrophy (if any) should also be noted. Ligamentous stability of the knee should be assessed and compared with uninjured side. Specific attention should be paid to evaluation of the ACL with the Lachman, pivot-shift, and anterior drawer tests. Increased anterior tibial translation during the anterior drawer test that is equal to or greater than translation noted during the Lachman test suggests a loss of secondary stabilizers, most commonly from a deficient posterior horn of the medial meniscus, but also from posteromedial or posterolateral insufficiency.12,13 Appropriate sizing of the meniscal allograft facilitates healing of the graft after transplantation. Thus meniscal grafts should be matched in both size and laterality. Measurements from the PA and lateral radiographs of the knee are used to size the meniscus, as described by Pollard and colleagues—the most common technique used by American Association of Tissue Banks (AATB)–certified tissue banks.14 This sizing method allows for an accurate estimate (within 3 to 4 mm) of the graft14 without the need for additional imaging. This size is given to the tissue bank, and an appropriately matched graft is obtained. The meniscal allografts are sterility harvested and fresh-frozen. They should not be irradiated before transplantation.
Combined Anterior Cruciate Ligament Reconstruction and Meniscal Allograft Transplantation
Preoperative Considerations
Physical Examination
Imaging
Surgical Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine