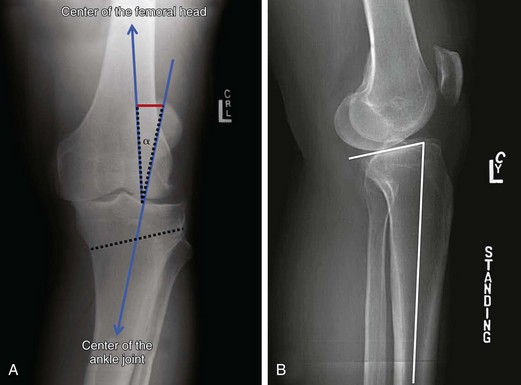
Chapter 62 In all patients with knee instability associated with joint arthrosis, thorough evaluation of the coronal (varus or valgus) and sagittal (tibial slope) alignment must be performed. In the past, knee instability was a contraindication to osteotomy. More recently, however, indications for high tibial osteotomy (HTO) have expanded to also include knee instability.1–3 This chapter describes the indications, planning, and surgical technique for combined anterior cruciate ligament (ACL) reconstruction and HTO. In the varus knee with ACL deficiency it is important to define the degree of varus alignment. The terms primary, double, and triple varus simplify the assessment of alignment and ligamentous deficiencies in a varus knee. Primary varus refers to the overall tibiofemoral varus osseous alignment (including medial meniscus and medial tibiofemoral articular cartilage loss). Double varus entails varus osseous alignment combined with separation of the lateral tibiofemoral compartment caused by lateral ligamentous damage (lateral condylar lift-off). The triple varus knee refers specifically to varus alignment resulting from (1) tibiofemoral osseous alignment, (2) increased lateral tibiofemoral compartment separation, and (3) varus recurvatum in extension caused by the abnormal increase in external tibial rotation and knee hyperextension, with involvement of the entire posterolateral ligament complex. The selection of an appropriate treatment must take into account the associated ligamentous injuries in addition to the varus malalignment.4 The use of combined ACL reconstruction and HTO is indicated in the following situations: 1. ACL rupture and severe varus alignment or hyperextension (more than 20 degrees) 2. ACL rupture and double or triple varus 3. ACL rupture, varus alignment, and symptomatic medial knee arthritis 4. ACL rupture, varus alignment, and lateral joint opening (lateral complex reconstruction or repair can be considered if residual lateral instability is present after combined HTO and ACL reconstruction) 5. ACL rupture, varus alignment, and external tibial rotation 6. ACL rupture and varus thrust 7. ACL rupture, varus alignment, and medial meniscus deficiency or osteochondral defects, when a combined medial meniscus transplant or performance of resurfacing procedures is planned We commonly plan the osteotomy as described by Dugdale and colleagues5 with a mild (3 to 5 degrees) valgus overcorrection (Fig. 62-1). After the correction, the mechanical axis (the line connecting the center of the femoral head with the center of the ankle joint) should pass through a point located at 62.5% of the tibial width, as measured from the tip of the medial edge of the proximal tibia. This point lies slightly lateral to the tip of the lateral tibial spine. In planning for opening wedge HTO, one line is drawn from this point to the center of the femoral head, and another line is drawn from this point to the center of the ankle joint. The angle between the two lines represents the angle of correction (α) (see Fig. 62-1). Next, the osteotomy line is measured from medial (approximately 4 cm below the joint line) to lateral (tip of the articular fibular head). This measurement is transferred to both rays of the α angle from the vertex. In this fashion the α angle is defined by two identical segments (equal to the osteotomy length), which are then connected by another line. This line serves as the base of an isosceles triangle and corresponds to the opening that should be achieved medially at the osteotomy site (see Fig. 62-1). In performing combined ACL reconstruction and HTO, the sagittal planning is very important. The tibial slope can be decreased with a more posterior plate positioning, to protect the graft (see Fig. 62-1). Opening Wedge High Tibial Osteotomy The surgery is performed with the patient supine on a radiolucent operating table (Box 62-1).1,3 A lateral post is positioned at the level of the thigh so that the foot can be dropped out of the table and at least 120 degrees of knee flexion can be achieved (Fig. 62-2). Intravenous antibiotic prophylaxis is performed. A tourniquet is placed around the proximal thigh. HTO is performed first. A 5-cm longitudinal incision is made, extending from 1 cm below the medial joint line midway between the medial border of the tubercle and the posteromedial border of the tibia.1,3 If a hamstring autograft is preferred, harvesting of the graft is performed at this point, to avoid damage to the tendons during proximal tibia exposure. The sartorius fascia is exposed by sharp dissection, and the pes anserinus is then retracted distally with a blunt retractor, exposing the superficial fibers of the medial collateral ligament (sMCL). The distal sMCL insertion is partially detached with a Cobb elevator. A blunt Hohmann retractor is then passed deep to the MCL to protect the posterior neurovascular structures. Next, the medial border of the patellar tendon is identified and retracted laterally with a hook or a second blunt lever. A guidewire is then drilled into the proximal tibia.1,3 The starting point of the wire is the anteromedial (AM) tibia at the level of the superior border of the tibial tubercle (about 4 cm distal from the joint line). The wire must be inserted aiming toward the tip of the fibular head (1 cm below the lateral articular surface). The guidewire positioning is assessed with fluoroscopy (Fig. 62-3). The tibial osteotomy is performed immediately distal to the guide pin, to protect against proximal migration of the osteotomy into the joint. The slope of the osteotomy in the sagittal plane is critical and should mimic the proximal tibial joint slope.1,3 A small oscillating saw is used to cut the tibial cortex from the tibial tubercle around to the posteromedial corner under direct vision. Thin, flexible osteotomes are then used to advance the osteotomy to within 1 cm of the lateral tibial cortex (Fig. 62-4). This is achieved with use of intermittent fluoroscopy and graduated osteotomes.6 The mobility of the osteotomy is checked by gentle manipulation of the leg with a valgus force and encouraged, if needed, by piling up two or three osteotomes.1,3 Graduated wedges are then engaged into the osteotomy and advanced slowly until the desired opening has been achieved (Fig. 62-5). Once the calculated preoperative correction has been achieved, a long alignment rod is used to check the mechanical axis. The rod is centered over the hip and ankle joints and, according to the preoperative planning, should lie at 62.5% or 50% of the tibial width, as measured from medial to lateral. The sagittal plane correction should also be assessed by fluoroscopy and by looking carefully at the size of the osteotomy opening. Considering the triangular shape of the tibia, if the opening at the level of the AM tibia is half the size of the opening at the level of the posteromedial tibia, the preexisting slope is maintained (Fig. 62-5B). The wedges (and the plate) can be moved anterior or posterior, according to the correction planned on the sagittal plane.
Combined Anterior Cruciate Ligament Reconstruction and High Tibial Osteotomy
Preoperative Considerations
Planning
Surgical Technique
Surgical Steps