Leaver-Dunn, Harrelson, Martin and Wyatt (2002), investigated the tendency of undergraduate athletic training students to think critically. Their research findings provide some useful considerations in terms of understanding critical thinking as a precursor to clinical reasoning. In their study, they employed an objective measure called the California critical thinking disposition inventory to quantitatively measure critical thinking. The inventory has a number of subscales, which depict the components of critical analysis. The weakest subscale was that of truth seeking, which highlights the ability of a critical thinker to reflect on knowledge and engage a quest to find the truth irrespective of current views. The reasons attributed to the weakness in the truth scale could be explained by emphasising the need to know the correct answer as opposed to understanding the reasons for the correct answer and the ability to reflect on the answers reached. Whilst this chapter does not explore critical thinking as a separate entity to clinical reasoning, knowledge of critical analysis and reflection is central to developing skills necessary for understanding clinical decisions and actions.
Development of clinical reasoning skills
Problem based learning
One possible approach to teaching and developing reasoning skills is problem based learning (PBL). PBL has its history firmly rooted within the teaching and education of medical practitioners although its application to other disciplines has been researched and documented (Wood 2003). PBL evolved through two assumptions: the first was that learning through problem solving is more effective than memory based learning for creating a usable body of knowledge; the second was that clinical skills, which are important for patient treatment are problem solving skills not necessarily memory skills. PBL is not a method as much as a total teaching approach and reflects the way learners learn in real life situations. It has been used in varied study contexts to develop critical analysis and thought, as well as problem solving skills (Duncan et al. 2007). Through the use of PBL within the sports rehabilitation curriculum, it is hypothesised that the cardinal skills of critical thinking, analysis and application will develop leading to greater levels of student intrinsic motivation. Using PBL with undergraduate students could enable the growth and evolution of critical analysis (Martin et al. 2008). One of the primary features of PBL is that it is student-centred. This refers to learning opportunities that are relevant to the students, the goals of which are at least partly determined by the students themselves. Creating assignments and activities that require student input also increases the likelihood of students being motivated to learn (Richardson 2005). A common criticism of student-centred learning is that students, as novices, cannot be expected to know what might be important for them to learn, especially in a subject to which they appear to have no prior exposure. The literature on novice-expert learning does not entirely dispute this assertion; rather, it does emphasise that our students come to us, not as the proverbial blank slates, but as individuals whose prior learning can greatly impact their current learning. Problem based learning encourages students to use and develop knowledge by examining problems or case study scenarios in a relevant, real-life and applied context (Martin et al. 2008). Like many of the teaching approaches, PBL needs to be used carefully, especially in the design of the problem. Savin-Baden (2003) noted that PBL is an approach to learning that is characterised by flexibility and diversity, in the sense that it can be implemented in a variety of ways, across subjects and disciplines in diverse contexts. As such it can therefore look different to different people at different times, depending on the staff and students using it. What is unique and yet similar is the locus of learning around problem scenarios rather than discrete subject areas (Duncan et al. 2007).
Savery (2006), notes that the widespread adoption of the PBL instructional approach by different disciplines, for different age levels, and in different content domains has produced some misapplications and misconceptions of PBL. Certain practices that are called PBL may fail to achieve the anticipated learning outcomes for a variety of reasons:
- confusing PBL as an approach to curriculum design with the teaching of problem-solving
- adoption of a PBL proposal without sufficient commitment of staff at all levels
- lack of research and development on the nature and type of problems to be used
- insufficient investment in the design, preparation and ongoing renewal of learning resources
- inappropriate assessment methods which do not match the learning outcomes sought in problem-based programmes
- evaluation strategies that do not focus on the key learning issues and which are implemented and acted on far too late.
Using PBL in developing clinical reasoning skills is useful. Unlike traditional information driven curricula, PBL begins with a problem, often based on real facts or simulations of real situations, and requires the student to work alone and in groups to find solutions. The advantage is that real problems do not have simple solutions and require comparison and analysis of resources. As such the student develops skills of retrieval, selection and discrimination and applies these to reason through answers and solutions to problems (Duncan et al. 2007). PBL is one way in which clinical reasoning skills can be developed.
To develop an appreciation of the dynamics of PBL within the evolution of clinical reasoning skills, it is important to briefly address two important concepts that directly impact this evolutionary process namely: Troublesome knowledge (TK) and threshold concepts (TCs). It is not the intention of this chapter to analyse these concepts in depth, nor to critique their application, but to rather introduce them as important consideration in the development of clinical reasoning knowledge.
Meyers and Land (2003) related a definitional construct of threshold concepts by outlining that in each discipline, such as sports rehabilitation, there are conceptual gateways or portals that must be negotiated to arrive at important new understandings. In crossing the portal or threshold transformation occurs in both knowledge and subjectivity. Meyers and Land (2008) and Land et al. 2008 expand this further by detailing the transformation as irreversible (no-going back) and integrative (involving the inclusion and fusion of different ideas and concepts in both detail and variation). Such transformation involves troublesome knowledge.
Perkins (1999) referred to troublesome knowledge as knowledge that is alien or counter-intuitive, ritualised, inert, tacit or academically challenging. Perkin further relates that threshold concepts could lead to troublesome knowledge within their own rights.
Sports rehabilitation and injury prevention as a subject area and professional practice is troublesome within itself. The scope of practice, content of learning, curriculum map and clinical competencies may, at times, be conceptually and practically difficult to identify and embed into a distinct clinical practice model that stands unique from similar clinical and healthcare practices. The explanation of the field of sports rehabilitation involves defending a scope of practice that is construed by some professionals and clinicians as alien, or a subset of physiotherapy practice, yet surprisingly different. To fully consider action and decision making within sports rehabilitation and the ensuing development of clinical reasoning skills, it is fundamental that clinicians, academics and students, identify the threshold concepts and then use approaches such as PBL, to navigate TK and TCs to develop reflective ways of thinking and practice. The ability to think and reason like a professional clinician, is an important goal of the sports rehabilitation student.
The model in Figure 16.2 integrates TCs and TKs into a clinical reasoning development framework and considers a 6-D approach in defining conceptual difficulties and thresholds.
Figure 16.2 6D approach to knowledge development within a conceptual threshold framework (Abrahamson 2009).
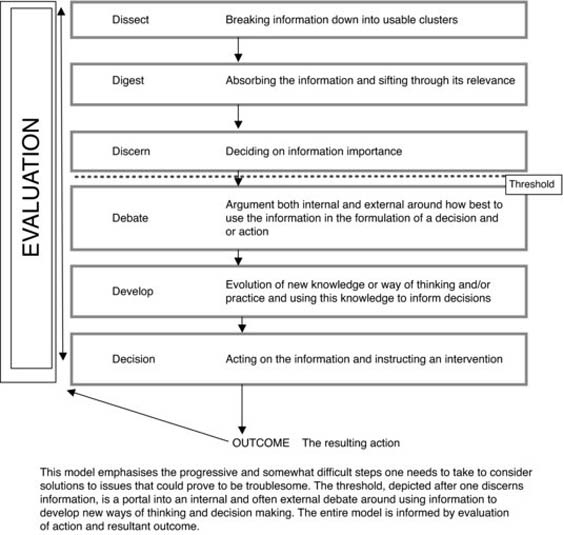
The model in Figure 16.2 develops a progressive strategy for thinking about action and clinical decision making. Säljö (1979), provides a useful analysis of learning as a developmental learning concept leading to a change in personal identity; that is the ability to master the strategies and competencies to think like a sports rehabilitator. To achieve this, learning must be aligned with understanding. The conceptual models align to illustrate the process of transformation and the traversing of TCs and TK.
The true characteristics of a proficient sports rehabilitator practitioner lie in the ability to cross thresholds, integrate new knowledge and construct bridges between the concepts to arrive at informed and evidence-based decisions and actions (Barrows and Pickell 1991).
In a recent study by Hauer et al. (2007) on the effect of causal knowledge on judgments of the likelihood of unknown features, the researchers reported that respondents perceived that technique problems in history taking and physical examination were readily correctable, but that poor performance resulting from inadequate knowledge or poor clinical reasoning ability was more difficult to ameliorate. Interpersonal skill deficiencies, which often manifested as detachment from the patient, and professionalism problems attributed to lack of insight, were mostly refractory to remediation. A possible explanation to this discrepancy could lie in the way in which problem solving/clinical reasoning skills are taught at an undergraduate level of training. Traditional approaches to teaching clinical skills are often based on the assumption that clinical reasoning is a skill, divorced from content knowledge. Although clinical reasoning skills and clinical knowledge could be developed and delivered separately, there is support for an integrated approach to improve the organisation and structure of relevant clinical knowledge and practices (Barrows and Pickell 1991).
Sports rehabilitation clinicians work within a framework of problematic situations. Many of these situations can be characterised by complexity, ambiguity, doubt and uniqueness. With this known entity, it may be better to conceptualise the skills required for professional practice and competency, in terms of smart action, as opposed to clinical reasoning. Differentiating the two at this level allows for a centred approach in dealing with judgment and decision making within a specific context and time. In other words smart action implies making the best decision under a given set of circumstances. It does not, however, mean always taking the right action. Smart action skills are often the catalyst for reflective analysis of performance. The evolution of this process provides the basis for professional development and critical awareness in decision making.
An important aspect of the development of higher cognitive skills and clinical reasoning ability is the ability to construct and use knowledge. The construction of knowledge requires an interpretation and processing of experience in order to appreciate reality. This often involves developing constructs to help understand reality and interpretation of experience. One cannot divorce thinking from the process, and that knowledge development requires thought, critical analysis and self-reflection on and of the knowledge construct. The next section will tease out the key elements that need consideration and development in mastering clinical reasoning skills.
How can we become better at clinical reasoning?
In order to become better, firstly we need to decide what needs improving. The majority of available research on clinical reasoning concludes that three processes interact in order to bring about good quality clinical reasoning (Higgs and Jones 2000; Higgs and Titchen 2001).
These three processes are knowledge, cognition and metacognition. These three interact throughout the process of receiving, interpreting, processing and utilising clinical information during decision making, clinical intervention and reflection on actions and outcomes.
Knowledge
Knowledge is essential for reasoning and decision making with knowledge and clinical reasoning being interdependent phenomena. There are two broad categories of knowledge. One is propositional knowledge (“knowing that”). This is achieved through research and scholarship (reading and being taught) and involves generalising information, looking for cause and effect relationships. The second type of knowledge is non-propositional (“knowing how”). Here knowledge is gained through practice experience. It would appear therefore that background knowledge is important but this must be task specific.
It is not the way problems are tackled, nor the thoroughness of the investigations, nor the use of problem solving strategies, but the ability to activate the pertinent knowledge as a consequence of situational demands, which distinguishes experienced from inexperienced physicians (Custers et al. 1992).
This ability to have and be able to recall task specific knowledge is one of the elements that marks out an experienced practitioner from a novice one. They are able to bring together many key elements of knowledge; anatomy, physiology, biomechanics, pathology, etc. and link them together to provide a rational explanation of the problem with which they are presented. This is often coupled with their practice experience (knowing how to do things), which then allows for a superior management of the patient. This use of knowledge is very much coupled to the process of reflection and this is covered in the next section.
Cognition and metacognition
Cognition is the act of thinking, with metacognition being the awareness and monitoring of cognition; that is, thinking about thinking. These two elements are integrated into clinical reasoning through the process of reflection. Reflection is an activity in which people recapture their experience, think about it, mull it over and evaluate it. Reflection itself involves two different aspects, one is reflection in action and the other is reflection about action. Reflection in action involves thinking about what you are doing, for example, whilst carrying out Lachman’s test at the knee, the practitioner should be reflecting on, “is this what I expected to find? If it isn’t, why isn’t it?” Reflection about action, is essentially thinking about what has happened after it has happened, questions such as, “what was good about what I did? What was bad? What can I improve for next time? What do I need to take away from the experience and store to use again?”
Reflection is the key to information processing in clinical reasoning. From a strong knowledge base, patterns can be identified; by reflecting in action the strength of the patterns relationship to the presenting problem can be tested. Reflection in action allows the solving of problems when the presentation does not fit a pattern through hypothetico-deductive reasoning. Finally, to complete the process, reflection about action becomes a process whereby those experiences can be stored and used to generate future patterns.
The process of clinical reasoning involves the testing of hypothesis in order to both discover what a patient’s problem is and develop an appropriate management strategy. There are a number of potential categories that this hypothesis can fit into, including: source of symptoms; mechanism of symptoms; contributing factors; precautions and contraindications; management and treatment; and finally prognosis.
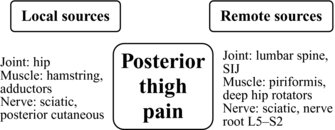
The source of symptoms can be considered by using a component model (Figure 16.3). As can be seen from Figure 16.3 the source of symptoms can either be local to the site of pain or remote from the site of pain, but capable of referring pain to the area of the pain. The mechanism of symptoms is what has caused the pain, this could be from an extrinsic source such as a kick or fall, it also could be from an intrinsic source such as with overuse injuries, were the tissues become overloaded and break down. The contributing factors are those factors that predispose the patient to the mechanism of injury occurring, they could include poor proprioception, muscle imbalances, shortened soft tissue structures or even lack of fitness and skill. The precautions and contra-indications are those factors that might limit any chosen course of action because of potential harm to the patient. The management and treatment hypothesis category is generating a plan for the patient, which, where possible, takes into account all of the above. For instance, not just treating the local source of symptoms but also those remote symptoms, which could perpetuate the problem, whilst also addressing any contributing factors that may cause the problem to reoccur or not be able to be resolved. Finally, the prognosis, taking into account all of the above, of how long will it take for the patient to get better? How much better will they get? And how long will it take? As you can see some of this information will come from knowledge, some from reflecting on the findings of the examination (reflection in action) and the progression of any treatments (reflection in and about action) and finally from collating the experiences of treating other patients and applying that information (reflection about action).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree