1 Clinical reasoning in Western acupuncture
Background
Using acupuncture to treat musculoskeletal disorders should follow a clinical reasoning process (CRP), the thinking behind practice, as identified by physiotherapists for manual therapy interventions (Jones & Rivett 2004), the norm being to identify predominant tissue and pain mechanisms presented by the patient as a means of identifying effective intervention. The layering method is a clinical reasoning model (CRM) developed specifically for clinicians to treat musculoskeletal conditions with acupuncture, using a mechanism-based approach (Bradnam 2007). It aims progressively to target different physiological processes within the central nervous system (CNS) in order to provide the best effect for each individual. The layering method is a Western approach to acupuncture, but does allow a clinician to integrate traditional Chinese acupuncture (TCA) point selection into clinical reasoning.
Theoretical knowledge underpinning the model
The following knowledge must underpin the model:
The practical implementation of the model relies on:
Acupuncture mechanisms
Nociception
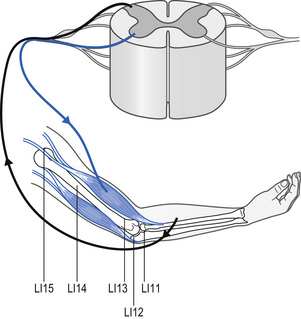
Three categories of acupuncture mechanisms have been described; peripheral, spinal, and supraspinal (Lundeberg 1998). Firstly, on needling, nociceptive afferents are stimulated and release vasodilatory neuropeptides into the muscle and skin they innervate, forming the basis of the local or peripheral effects of acupuncture (Sato et al 2000). This phenomenon, an axon reflex, releases neuropeptides into human skin such as calcitonin gene-related peptide (CGRP) and substance P (Weidner et al 2000). Sensory neuropeptides modulate immune responses and hence will assist in tissue healing (Brain 1997). Secondly, acupuncture will act within the spinal cord, known as spinal effects or segmental effects. To initiate spinal effects, the sensory stimulus must be applied to tissues that share an innervation with the appropriate spinal cord level (Fig. 1.1). Dorsal horn neurons activated by painful inputs may be inhibited by acupuncture via a gate control mechanism, producing a spinally mediated analgesic response. Neurons of the ANS efferent fibres can be influenced and both sympathetic and parasympathetic activity may be affected, depending on the position of the needles.
Lastly, acupuncture may influence alpha-motoneurons housed in the ventral horn of the spinal cord to alter reflex activity in muscles supplied by the segment (Fig. 1.1). At present the effect on motoneurons is still unclear: an immediate change in excitability has not been demonstrated in contrast to clinical observations (Chan et al 2004).
Neurohormonal responses
Responses affecting the immune, endocrine, and reproductive systems of the body can be affected by acupuncture (Carlsson 2002, Stener-Victorin et al 2002; White 1999). Recent advances in brain imaging technologies such as functional magnetic imaging (fMRI) and positron emission tomography (PET) have allowed investigations of the brain and have elucidated the effect of acupuncture on the CNS. Several analgesic points in the extremities will stimulate blood flow to cortical and subcortical brain regions (Lundeberg 1998). Activation is relatively non-specific and closely related to areas activated by painful stimuli, through what is known as the pain matrix (Lewith et al 2005). Studies show an increase in blood flow in the hypothalamus (Table 1.1) and a decrease in the limbic system (Table 1.2), a brain region where affective and emotional responses to pain are integrated with sensory experience. However, most of the brain regions activated by acupuncture are closely related to those areas mediating placebo analgesia and expectation (Lewith et al 2005), and it is unclear how much of the change is due to the acupuncture stimulus and how much is due to non-specific effects. Recently studies using transcranial magnetic stimulation (TMS) have shown that acupuncture modulates motor cortical excitability and that the effect (excitation or inhibition) is specific to the investigated muscle and the site of needle placement (Lo et al 2005; Maioli et al 2006). Maioli et al (2006) showed that changes lasted for fifteen minutes following the removal of the needle stimulus, suggesting longer term plastic changes in motor cortical excitability.
Table 1.1 Suggested points to stimulate blood flow to hypothalamus
| Meridian | Points |
|---|---|
| Large intestine | LI4 |
| Lung | LU5 |
| Gall bladder | GB34, GB40 |
| Spleen | SP6 |
| Stomach | ST36 |
| Liver | LIV3 |
Biella et al (2001); Fang Kong et al (2004); Hsieh et al (2001); Hui et al (2000); Wu et al (1999, 2002); Yan et al 2005; Zhang et al (2003)
Table 1.2 Suggested points for deactivation of limbic system
| Meridian | Points |
|---|---|
| Large intestine | LI4 |
| Gall bladder | GB34 |
| Spleen | SP6 |
| Stomach | ST36 |
| Liver | LIV3 |
Hsieh et al (2001); Hui et al (2000, 2005); Kong et al (2002); Wu et al (1999,2002); Zhang et al 2003
Clinical reasoning model: the layering method
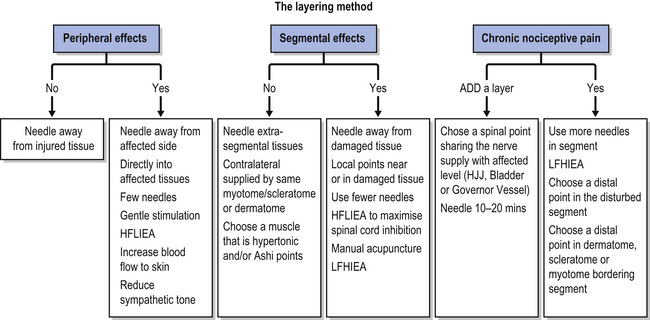
Clinical reasoning within acupuncture intervention requires that the clinician ask a series of questions as to what is required from the needle. The question provides a problem-solving pathway as to effects on pain and tissue mechanisms presented, appropriate points and stimulation parameters chosen, in an effort to provide an optimum intervention. The clinical reasoning questions can be seen in the flowchart in Fig. 1.2.
Local effects
Healing
If healing or treating scar tissue is the aim of therapy, blood flow can be improved by eliciting local effects of acupuncture, using local acupuncture points, or by putting the needle directly into the damaged tissue. Lundeberg (1998) recommended needling close to the injured tissue with LI stimulation to encourage peripheral neuropeptide release. However, in the early stages of an injury the increase in blood flow, substance P, and other inflammatory agents are potentially detrimental and have the effect of overloading, leading to increased pain and inflammatory response (Longbottom 2006a).
Segmental effects
Analgesia
Local points can induce segmental effects if desired. In acute pain, segmental blocking of painful afferent input can produce strong analgesia. Any acupuncture points in tissues that share an innervation via that spinal segment can be chosen, as long as the injured tissue is avoided (Bradnam 2007). In cases of acute nociceptive pain it is advised that fewer needles be used since the dorsal horn is already sensitized. If the condition becomes chronic, more needles can be added into the segment (Lundeberg 1998). Choosing distal points, in other muscles or tissues sharing the same innervation as the injured tissue, may offer a more effective treatment (Bradnam 2007).
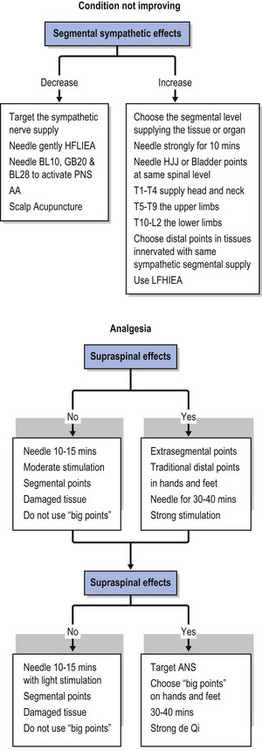
Sympathetic nervous system
For patients demonstrating clinical presentation suggestive of an overactive sympathetic nervous system (SNS) with oedema, sweating, and severe pain (Longbottom 2006a), acupuncture can induce specific manipulation of the ANS (Table 1.3). This may also be used when an increase in blood flow to a tissue is required (Bradnam 2007). Slow-healing conditions might be related to trophic changes in tissues via inhibition of the SNS (Bekkering & van Bussel 1998). The sympathetic neurons are housed in the segments of the thoracic and upper lumbar spines; needling at the appropriate spinal level will alter the outflow to that region. Hsu et al (2006) found with healthy volunteers that 2 Hz electroacupuncture (EA) applied to Bladder 15 (BL15) increased heart and pulse rate, and decreased skin conductance on the upper limb, all signs of increased sympathetic outflow. Also needling a peripheral point, using strong activation of de Qi, will stimulate afferent input into the chosen segment and will increase sympathetic outflow, and increase the blood flow to muscles (Noguchi et al 1999).
Table 1.3 Sympathetic supply and point suggestion
| Segmental level | Areas supplied | Suggested points |
|---|---|---|
| T1–T4 | Head and neck | Large intestine (LI4) |
| T5–T9 | Upper limbs | Bladder (BL15) |
| T10–L2 | Lower limbs | Bladder (BL23) |
Bekkering & van Bussel (1998).
If the desired effect is inhibition of sympathetic outflow gentle stimulation to the spinal points must be given. In addition, auricular acupuncture (AA) will increase parasympathetic activity (Lundeberg & Elkholm 2001), hence reducing sympathetic outflow. According to Longbottom (2006a), points that influence the cranial sympathetic outflow Bladder (BL10) and Gall Bladder (GB20), and sacral sympathetic outflow (BL28), will also activate the parasympathetic nervous system (PNS) and can be used to dampen overactive sympathetic responses. Scalp acupuncture has also been shown to stimulate the PNS and suppress sympathetic activity in healthy volunteers compared to control subjects (Wang et al 2002).
Supraspinal effects
Analgesia
Needles left into any points in the body for 30 to 40 minutes will enhance supraspinal effects as these are time and intensity related (Andersson & Lundeberg 1995; Lundeberg 1998; Lundeberg & Stener-Victorin 2002). De Qi must be achieved to elicit brain activity; the greater the intensity of stimulation and de Qi gained, the greater the blood flow to cortical regions (Backer et al 2002; Fang et al 2004; Wu et al 2002).
Activating the DNIC by segmental acupuncture is thought to produce analgesia that is stronger than that of extrasegmental needle placement but is only short lasting (Lundeberg et al 1988a). A combination of both segmental and extrasegmental needling is commonly used in clinical practice (Barlas et al 2006). However, when trying to activate DNIC to treat acute nociceptive pain, or centrally evoked pain, it may be prudent to activate them via extrasegmental inputs to avoid overloading the sensitized spinal cord segment. The hands, and to a lesser extent the feet, have large representation on the somatosensory cortex in the brain and are considered strong points in acupuncture analgesia.
In peripheral neurogenic pain the opioid pain inhibitory systems are less effective due to increased synthesis of the neuropeptide cholecystokinin, an endogenous opioid antagonist (Wiesenfeld-Hallin & Zu 1996). Here, EA applied with a high-frequency/low-intensity (HFLIEA) paradigm, activating the noradrenergic (non-opioid) pathways in the spinal cord, should be used (White 1999).
Autonomic outflow
Autonomic outflow is under central control by the hypothalamus regulating the SNS and PNS (Kandell et al 2000). Stimulation of this system is considered non-specific and depends on intensity and length of stimulation. To effectively activate central autonomic responses, the use of strong points, similar to those used to evoke central responses, has been recommended. Acupuncture stimulation may increase or decrease sympathetic activity depending on the state of the target organ or tissue (Sato et al 1997). For optimum treatment of body organs, Stener-Victorin (2000) recommended the use of high-intensity, low-frequency EA to provide a strong stimulus to the CNS.
Motor cortex
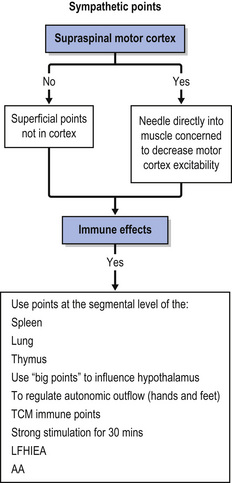
A novel use of acupuncture may be to specifically excite and inhibit motor regions of the brain associated with overactive or inhibited muscles during a motor task. This may facilitate acupuncture to be used in the treatment of various motor control disorders. Maioli et al (2006) needled acupuncture point Large Intestine 4 (LI4), and found that the motor cortical area for the abductor digiti minimi muscle was inhibited. However, there was no observation of significant alteration in motor cortical excitability of the flexor carpi radialis muscle, suggesting that the effects are localized to the region of the body being treated. The motor cortical areas for both these muscles, and a third, the first dorsal interossei, were facilitated following needling applied to a point in the leg Stomach 38 (ST38). Furthermore, Lo et al (2005) found that acupuncture to LI10 significantly increased motor cortical excitability to the area supplying the first dorsal interossei.
Immune system
Following acupuncture beta-endorphin and adrenocorticotropic hormone (ACTH) are released in equimolar amounts from the pituitary gland into the blood stream (Lundeberg 1999). In turn, ACTH may influence the adrenal gland, increasing the production of anti-inflammatory corticosteroids (Sato et al 1997). Beta-endorphin levels may fluctuate with changes in the number and activity of T-lymphocytes and natural killer (NK) cells. These effects may optimize healing effects under slow-healing conditions associated with immune deficiency or in those individuals exhibiting high-intensity demands on the body (i.e. elite athletes). To influence the organs producing T-lymphocytes and NK cells, the thymus and spleen and lung segments, supplying both sympathetic and parasympathetic innervation, should be needled together with parasympathetic AA points, because of their potential to influence vagal parasympathetic activity (Lundberg 1999).
Conclusion
This clinical reasoning model proposes a theoretical framework for the application of Western acupuncture, using current physiological theories to underpin and inform clinical decision-making, and as a basis for treatment progression. It is recommended that clinicians measure outcomes and use reflective practice when implementing the model since it has not yet been validated by primary research in a clinical setting.
1.1 Clinical reasoning in traditional Chinese medicine
The diagnostic process and identification of disease categories (Bian Zheng) is an essential process of traditional Chinese medicine (TCM); indeed the traditionally trained acupuncturist cannot formulate an intervention without it. This may offer some problems with diagnostic reliability and has implications within clinical trials using TCM philosophy and interventions (Zaslawski 2003). Over the past decade there has been a proliferation in acupuncture research with increased numbers of reports offering cautious acceptance of acupuncture as a statistically proven therapeutic technique for certain conditions (Ernst 2003). Many systematic reviews and meta-analyses of acupuncture have concluded that there was insufficient evidence to determine the efficacy of acupuncture; many trials reviewed were of poor quality, and required further rigorous research. In response, a number of authors have questioned the validity of such methodologies and have emphasized a need for further investigation of the research methodologies used (Birch 2001; Cummings 2000; Ezzo et al 2001; Lao et al 2001).
The pathological presentation in TCM is known as pattern identification (Bian Zheng) using a clinical reasoning model to determine the disease state and cause of the dysfunction, whether this be at a systemic organ level, presenting with the more chronic longer standing disease state (Zhang fu Bian Zheng), or superficial channel level, presenting with more acute shorter disease state (Jing Luo Bian Zheng). In Western acupuncture a parallel model of clinical reasoning, identifying the stage of the disease, and the mechanism and the source of pain presentation, is required to determine the effective stimulation of appropriate neurotransmitters in order to restore homeostasis, enhance pain modification, and facilitate movement and rehabilitation. Once a diagnosis has been reached, the treatment principle (Zhi Ze) can be formulated and the treatment method selected (Zhi Fa) (Zaslawski 2003).
The concept of illness or pattern diagnosis (Zheng) is fundamental as this will offer the practitioner information on nature (Table 1.4), source, location, cause, and pathomechanisms involved; it will ultimately lead to the correct intervention for the management of the presenting mechanism. If, for example, a patient presents with shoulder pain, aggravated by loading specific rotator cuff muscles, worse on muscle activity but eased by unloading, careful examination and assessment may well reveal that myofascial trigger points (MTrPts) are responsible for the presenting myofascial pain mechanism. Appropriate deactivation of those responsible dysfunctional muscles, re-education of muscle imbalance, and restoration of range of movement (ROM) may resolve the pathology without the use of segmental dorsal horn inhibition or descending inhibitory techniques. A patient presenting with complex shoulder pain brought about by abnormal CNS processing and increased sympathetic excitation may well describe pain in the shoulder, but the acupuncture intervention will require a more extensive pattern identification involving the status of the SNS, emotional status, and coping mechanisms. Acupuncture intervention may well be required to stimulate parasympathetic excitation, to promote sleep and well being, whilst a more prolonged intervention using pain gate and descending inhibitory intervention may be required over a longer period of time (Spence 2004; Streng 2007).
Table 1.4 Classification of the diagnostic system in traditional Chinese medicine
| Diagnostic classification system | Guiding principles |
|---|---|
| Ba Gang Bian Zheng | Eight principles of pattern identification Yin or yang Internal or external Deficiency or excess Cold or heat |
| Zang Fu Bian Zheng | Viscera and bowel patterns used primarily for herbal medicine |
| Liu Jing Bian Zheng | Six-channel pattern identification Superficial (yang) channels to deep (yin) channels |
| We Qi Ying Xue Bian Zheng | Four-level pattern in superficial channels especially warmth |
| San Jiao Bian Zheng | Differentiation of the three compartments (jiaos)—upper, middle, and lower—and externally contracted diseases especially warm diseases |
| Qi Xue Bian Zheng | Qi and blood pattern identification with changes in these substances Deficiency and excess |
| Jin Ye Bian Zheng | Body fluid pattern identification Phlegm and fire phlegm |
| Wu Xing Bian Zheng | Five-phase patterns of bowels and viscera |
| Jing Luo Bian Zheng | Channels and musculoskeletal pattern identification |
Knowledge of the cause of the presenting condition (pathogen) is essential, whether via injury (channel and network presentation or nociceptive pain mechanisms), infection (warmth disease, circulatory dysfunction, or viral invasion), chronic development (cold invasion, Qi or blood deficiency, bi syndrome, or system dysfunction), or acute onset (heat, Qi and blood excess). Regardless of whether it is an internal organ pattern or an external superficial channel pattern, the presenting condition will have a profound effect on pain mechanisms at different levels and as such should influence the choice of needle application, length of treatment, and method of stimulation.
If the primary reason for seeking intervention is pain modification, then the primary goal of intervention is to determine the presenting pain mechanism using the correct intervention. Ultimately, resolution of the pain mechanism will lead to resolution of joint range, functional restoration, and successful rehabilitation outcomes (Lewis 2006).
It is the structure of underlying knowledge, gained through repeated problem solving, matching knowledge with experience, that provides a pathway to guide the practitioner through the many stages of the recovery process. Few research studies identify the reasoning strategies that clinical practitioners utilize in an attempt to guide the intervention. Indeed, few studies are undertaken to determine the facts underlying the choice of intervention, although a large body of evidence relating to clinical reasoning in medicine (Cox 1999; Jones & Rivett 2003), physiotherapy (Cox 1999; Higgs 1992; Higgs & Jones 1995; Jones & Rivett 2003; Pitt-Brooke 1998), and many other health care professions is now at hand. This does not appear to be the case when acupuncture is incorporated into a physical therapy management regime. As a result, a prescriptive point-selective model has been widely used which may hamper the ability to progress the treatment or re-evaluate the acupuncture should progress be slow.
The development of expertise within any clinical field relies heavily on extensive clinical practice developing a highly structured and rich knowledge base (Bordage & Lemieux 1991; Custers et al 1996), which can be attained by physiotherapists using acupuncture within manual therapy. When a clinical reasoning model is used, based upon the knowledge of the changing pain state and disease process, treatment should be mirrored by changing acupuncture point selection and methods of application. Treatments should have no constant method just as the disease state has no constant presentation. As pain and dysfunction start to resolve, acupuncture point selection should vary. Equally, if improvement and healing are not forthcoming, a reappraisal of the disease state should be undertaken and may lead to alternate pain modification techniques and point selection.
‘Disease has no constant form, treatments have no constant method and practitioners have no constant formula.’ (Longbottom 2007)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree