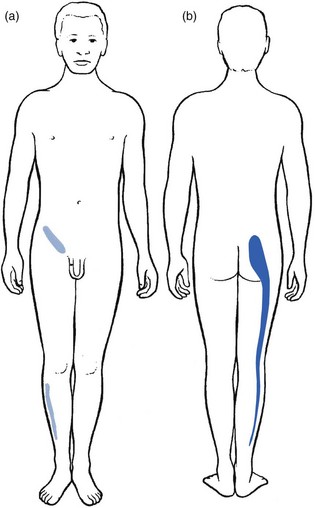
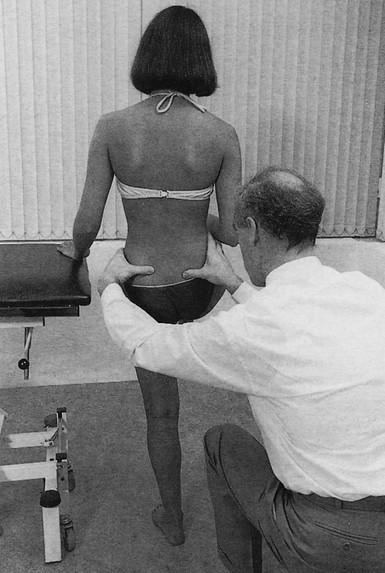
41 Sacroiliac arthritis, both rheumatic and septic, is a common cause of unilateral gluteal pain. The sacroiliac joint is a true synovial joint and therefore subject to the same inflammatory and infectious conditions that affect other synovial joints.1,2 However, the sacroiliac joint as a primary source of mechanical backache remains controversial and diagnoses such as ‘sacroiliac dysfunction’ or ‘sacroiliac subluxation’ are ill defined and difficult to substantiate.3–5 Much of the controversy is caused by lack of agreement on clinical criteria that justify the diagnosis of sacroiliac lesions. If the diagnosis is made only on the basis of pain localization or tenderness on palpation, sacroiliac lesions will be seen frequently. If the diagnosis is based on a thorough clinical examination of lumbar spine and pelvis, sacroiliac lesions will be rare. Unilateral pain and tenderness in the region of the sacroiliac joint is usually a manifestation of the confusing phenomena of referred pain and referred tenderness from a dura mater at a low lumbar level and not a reliable clinical proof of a sacroiliac disorder.6–9 Furthermore, mechanical testing of the sacroiliac joints – exerting tension on the sacroiliac ligaments without affecting the lumbar spine and the hip joint – is not easy. Most commonly used tests lack this requirement, which may explain the differences of opinion between examiners.10–12 A discussion of the disorders affecting the joint requires definition of the following terms: • Sacroiliac strain/sprain is overstretch or rupture of the capsuloligamentous structures as a result of abnormal joint movement. • Sacroiliac instability is a condition of abnormal joint mobility caused by capsuloligamentous laxity. • Sacroiliac subluxation is permanent displacement of the bony parts forming the joint. • Sacroiliac dysfunction is a reversible decreased mobility of the joint, the result of articular causes. • Sacroiliac arthritis is an inflammatory condition of the joint. The concept of a ‘sacroiliac sprain’ as a common cause of backache and sciatica was introduced by Goldthwait and Osgood in 1905 and reinforced by others.13,14 It still persists. However, MacNab8 noticed that sacroiliac sprains only occur below the age of 45 and in circumstances creating considerable force on the joint, such as those generated by falls from a height or motor vehicle accidents. Cyriax7 (his p. 364) advised reserving the term for cases of pain arising from the sacroiliac ligaments in the absence of arthritis. However, difficulty arises in those examples of early sacroiliitis in which pain and clinical signs precede the appearance of radiographic sclerosis. Clinical assessment does not differ from that described for the lumbar spine in low back pain disorders (see Ch. 36). When data from the history and functional examination suggest the possibility of a sacroiliac lesion, special tests can be performed and additional imaging studies requested.15 Most instances are the result of lumbar disc protrusions with segmental (L1, L2, L3 and S1, S2) or multisegmental (lumbar dural) reference of pain. Arthritis of the hip joint is another possibility: pain may be felt in the inner and upper part of the buttock because of segmental reference of this joint in the third lumbar segment (see p. 11). The innervation of the sacroiliac joint and its ligaments is wide and complicated.17 Studies confirm that the anterior portion of the joint is innervated by the ventral rami of L5, S1 and S2, and the dorsal portions of the joint by the dorsal ramus of L5 and a plexus derived from the dorsal rami of the sacral nerves.18–20 The superior part of the joint and the iliolumbar ligaments have an L2 and L3 origin. In sacroiliac strain or arthritis, pain is most often felt in the buttock, with radiation to the back of the thigh and the calf but never the foot. Often there is groin pain too.21 A typical distribution of pain is shown in Figure 41.1.22 History taking should cover preceding disease, trauma, pregnancy and delivery, occupation and working habits, as well as sports and recreational activities. Family and social history are of similar importance.23 In pelvic peripartum instability, the pain often starts in the third month or within the first few weeks after delivery. In sacroiliac lesions, a typical finding is that there is unilateral gluteal pain (often deep, dull and ill defined24–26), perhaps together with reference to the S1–S2 dermatomes, chiefly the posterior thigh. Pain may alternate in the right and left buttocks which strongly suggests a manifestation of early ankylosing spondylitis, particularly when it is found in males aged between 15 and 35. Some authors describe the adoption of an antalgic gait in painful disorders of the sacroiliac joint27,28 and a tilt of the trunk, most frequently towards the painless side.27 Some patients avoid sitting on the buttock of the affected side.28 Neurological symptoms, such as paraesthesia, weakness or numbness, are absent. Clinical examination of the sacroiliac joint is not routinely undertaken in low back pain and sciatica, except for one test – sacroiliac distraction (see Fig. 41.3 below) – because this is the most sensitive test to detect inflammation in the joint. Routine clinical examination of the lumbar spine can be negative but some symptoms may point in the direction of possible sacroiliac involvement because of low back pain and/or sciatica. In sacroiliac strain, the basic tests are usually not capable of evoking pain.29,30 It is only when movements really stretch the ligament and when this is prolonged that an injured ligament may react painfully. A diagnosis of ligamentous strain is thus based on the history, painful reactions after prolonged load, and the outcome of special sacroiliac tests (Box 41.1). The best-known palpation tests are the standing and sitting flexion palpation tests and the Gillett test.31 The Gillett test is performed as follows. The patient stands with the back to the examiner (Fig. 41.2), who places one thumb just underneath the posterior superior iliac spine and the other on the second sacral spinous process or on the contralateral superior iliac spine. The patient is asked to lift one knee as high as possible, which rotates the ilium on that side posteriorly and therefore moves the posterior superior iliac spine inferiorly relative to the opposite side. Fixation of the sacroiliac joint prevents this movement or, paradoxically, even gives rise to elevation of the posterior superior iliac spine as the patient compensates by tilting the pelvis at the point of maximal hip flexion. This manœuvre is usually painful in symptomatic patients.
Clinical examination of the sacroiliac joint
Introduction
Referred pain
Pain referred to the region of the sacroiliac joint
Pain referred from the sacroiliac joint16
History
Functional examination
Introduction
Sacroiliac tests
Palpation tests
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Clinical examination of the sacroiliac joint