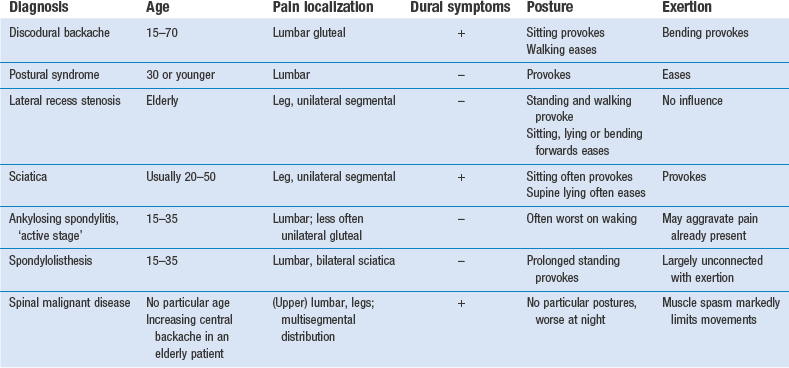
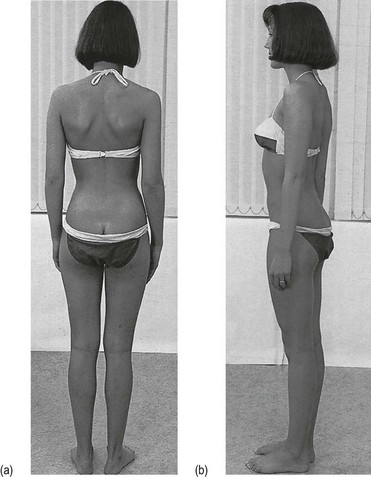
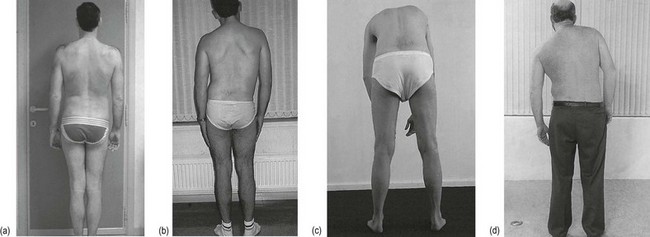
36 • Lumbago: a sudden attack of severe low back pain, causing some degree of fixation and twinges on attempted movement. • Backache: discomfort in the lower back. • Sciatica: pain that radiates strictly from the buttock to the posterior thigh and calf. It is restricted to a specific dermatome (L4, L5, S1 or S2) and may be accompanied by paraesthesia and motor and/or sensory deficit. In practice, however, the term is used inaccurately if pain and paraesthesia are felt in the anterior part of the thigh and/or lower leg (L2–L3). In lumbar spine problems, the mechanism of causation is usually reflected in the behaviour of the pain. Localization of the symptoms, their evolution and the relation to activity and posture differ according to the tissue involved. Pain in the lumbar and pelvic–gluteal area is usually of local origin but may also be referred from intra-abdominal or pelvic lesions. Sometimes lumbar pain is devoid of any organic basis and is then labelled as non-organic or ‘functional’. Local organic disorders may or may not be related to activity. The former are called activity-related spinal disorders, the latter non-activity-related spinal disorders (Box 36.1). • Inflammatory diseases, both septic and rheumatological. • Osseous disorders, such as osteoporosis, fractures or tumours. • Acquired defects of the vertebral arch. • Intraspinal lesions, such as neuroma, metastases and cysts. While taking the history, the examiner endeavours to find an answer to the following questions: • Is this an organic or non-organic lesion? • Do the symptoms point to activity-related disorders? • What sort of disc lesion is present? • What other type of lesion is more in accordance with the symptoms? • What type of person is the patient? Is it obvious that the degree of pain and effect on daily activities tally with appearance and behaviour? Because low back pain is most often caused by a soft tissue lesion and so is frequently attributed to disc disorders, the history serves in the first place to verify whether this is the case. ‘All discs are alike, all other lesions are different’ is Cyriax’s statement, which has been proved true in orthopaedic practice. Therefore, in disc displacements of all types, confirmation of the facts detailed in Chapter 33 is expected. During the history the interviewer should obtain specific data on the following: Sciatica caused by a posterolateral disc protrusion can be expected from adolescence to old age. In elderly patients, lateral recess stenosis is to be more frequently expected as the cause of root pain (Table 36.1). Also, degenerative spinal stenosis is a disease that occurs predominantly in the elderly. Table 36.1 Ankylosing spondylitis typically provokes alternating sciatica between 15 and 35 years of age. It is 4–9 times more frequent in men.1 In disorders of the lower back, symptoms can diversify. The clinician must try to obtain a clear impression not only of present discomfort but also of former events (see Box 36.4). Pain is the most common and important symptom and is usually what forces the patient to seek medical help. Other symptoms are not always mentioned spontaneously but should be asked about: the presence of paraesthesia, numbness, a cold foot or incontinence. All the different aspects of pain should be investigated: localization, onset, evolution and duration of the perceived ‘current’ pain; influence of movement and posture; and the presence of dural symptoms. It is also very useful to obtain information on the same factors in previous attacks (Box 36.2). Patients are first asked if they feel any pain at the present time and to point to its location. The method chosen may give information on emotional status. A stable patient generally places the palm of the hand at the site of maximal pain and moves it across the body to demonstrate the route of radiation. A psychologically unstable patient never touches the painful area but only points it out vaguely with the thumb.2 If the patient points to the upper lumbar area, the investigator should immediately be on the alert. Malignant diseases in the lower back have a great preference for this area (see p. 536). Pain in one lower buttock only is rarely dural; more commonly, it is a segmental reference from S2. The next question concerns the speed of onset: ‘How did it start: was the onset sudden or gradual?’ In ‘ligamentous postural’ syndromes, pain is particularly increased by maintenance of a particular posture, whereas altering the position relieves the pain. Moreover, the longer the position is maintained, the more intense the pain becomes. Barbor3 described the discomfort of ligamentous pain as ‘the theatre, cocktail party syndrome’: it is impossible to sit at the theatre or stand at the cocktail party without low backache occurring. In contrast, the symptoms are relieved by activity. This syndrome is typically found in the young. Another factor that may influence symptoms is raised intra-abdominal pressure during coughing and sneezing (Box 36.3). Pain in these circumstances may be a dural sign produced by sudden increased intradural pressure, which in turn causes sudden expansion of the dura pressed against the protrusion. Although it is very often related to a disc protrusion, it is clear that any space-occupying lesion in the lumbar spinal canal compressing the dura mater (e.g. a neuroma or malignant tumour) may evoke the same response. Often the patient will not mention it spontaneously, so the investigator must enquire about coughing and sneezing. Because mobility tests for the fourth sacral roots do not exist, it is almost impossible to evaluate their function. The diagnosis of cauda equina syndrome should therefore be made entirely on the history. Patients typically present with a classic triad of (1) saddle anaesthesia, (2) bowel and/or bladder dysfunction, and (3) lower extremity weakness.4 Some patients are timid and do not mention these symptoms, so it is important to ask about them in the three types of case in which a large posterocentral protrusion is to be suspected: acute lumbago, acute perineal pain and bilateral sciatica. It should be re-emphasized that manipulation is absolutely contraindicated; even traction is not at all safe if the slightest suspicion of compression of the fourth sacral roots arises. Prompt surgery is required and any delay results in substantial morbidity.5 • How does the patient enter the room? A posture deformity in flexion or a deformity with a lateral pelvic tilt, possibly a slight limp, may be seen. • How does the patient sit down and how comfortably/uncomfortably does he or she sit? • How does the patient get up from the chair? A patient with low back pain may splint the spine in order to avoid painful movements. • What is the facial expression? Is it in accordance with the pain the patient seems to suffer? The patient should be observed posteriorly and laterally. From the posterior aspect, the shoulders and pelvis should be level and equal, and the soft tissue structures on both sides should be symmetrical (Fig. 36.1a). The thoracic and lumbar vertebrae should be vertically aligned. The angles of the scapulae should be level with the seventh thoracic spinous process; the iliac crests should line up with the fourth lumbar vertebra. The lower extremities should share the body load and be in good alignment: the hip joints not adducted or abducted, knees not bowed or knock-kneed, feet parallel or toeing out slightly, and the calcaneal bones neither pronated nor supinated. From the side (Fig. 36.1b), the thoracic kyphosis and lumbar lordosis are observed and should have a normal curve. The pelvis should be in the neutral position, i.e. the anterior superior iliac spines lie in the same vertical plane as the symphysis pubis. Hip, knee and ankle joints should be neither flexed nor hyperextended. There is no clear evidence as to the significance of differences in leg length in the generation of spinal symptoms. If a platform under the shorter limb eases or even abolishes the pain while standing or on lumbar flexion or extension, a raised heel is advised. Some physicians recommend correction of any kind of leg length inequality. However, most investigators agree that mild leg length inequality of up to 15 mm is not a factor that contributes to low back pain.6,7 Correction is therefore only of importance in recurrent attacks of lumbago and in the presence of a difference of more than 15 mm. In lumbar disc displacements, six possible types of deviation (sciatic scoliosis) exist: • Towards the painful side. This shows that the displacement is situated medially, i.e. at the axilla of the nerve root. • Away from the painful side. In this case, the protrusion lies lateral to the nerve root, which is drawn away by the deviation of the trunk. • Alternating deviation. This demonstrates that the dura mater slips from one side to the other of a small midline protrusion. It is also diagnostic of a protrusion at the fourth lumbar level. • Deviation on standing, which disappears during flexion. • No deviation when standing erect but marked deviation on attempted trunk flexion. This is often seen in root pain. • A momentary deviation when the trunk is flexed halfway. The patient is seen to deviate suddenly at a particular moment during flexion, returning to a symmetrical posture as this point is passed. Usually pain is felt at the moment of deviation but occasionally it is not. This sign indicates that a fragment of disc alters its position at the back of the intervertebral joint and temporarily touches the dura mater.
Clinical examination of the lumbar spine
History
Introduction
Localization of the symptoms
Pathogenesis
Non-activity-related spinal disorders (Ch. 39)
Problem solving
Age and activities of daily living
Age (years)
Disorder
15
Spondylolisthesis
15–35
Ankylosing spondylitis
20–50
Disc lesions
Elderly
Spinal and lateral recess stenosis
Routine of history taking
Pain
Current pain
Side and level
Onset of pain
What factors influence the symptoms?
Previous attacks
Danger to S4 nerve roots
Inspection
The shape of the normal trunk
The pathological trunk
Posterior view
Static scoliosis (Fig. 36.2a)
Sciatic scoliosis (Fig. 36.2b)