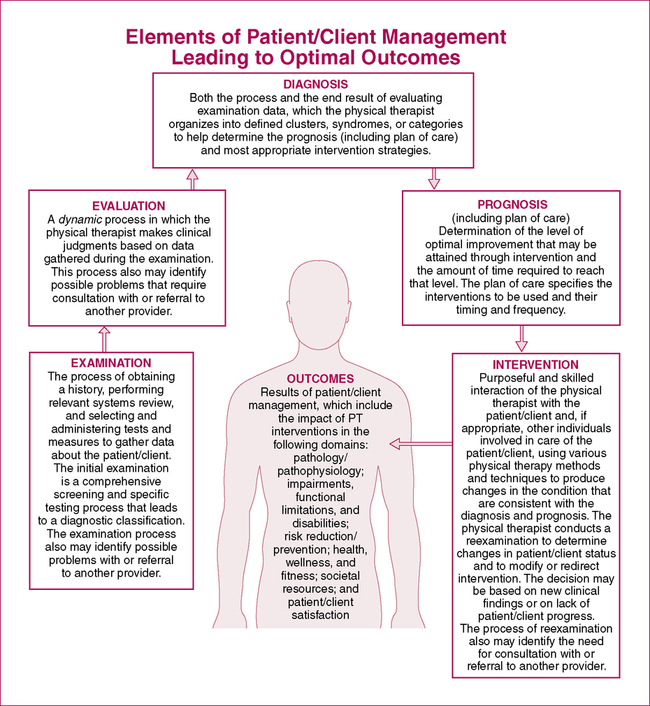
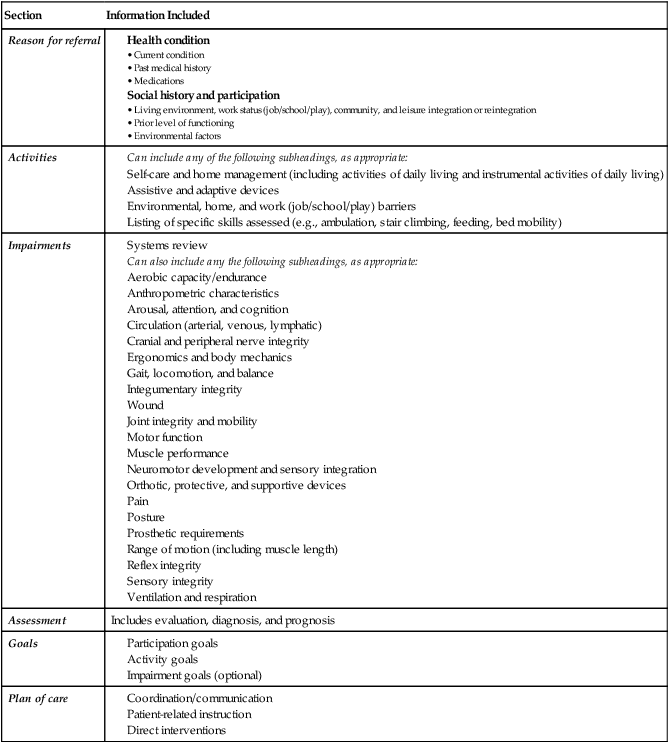
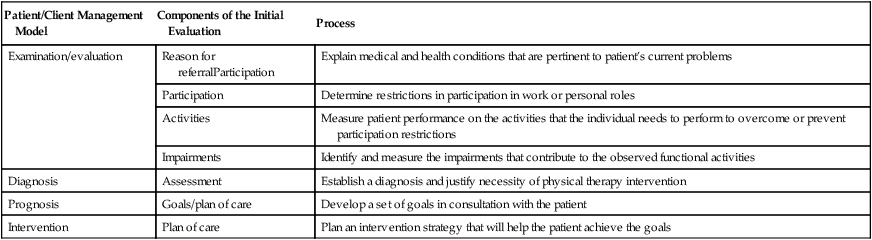
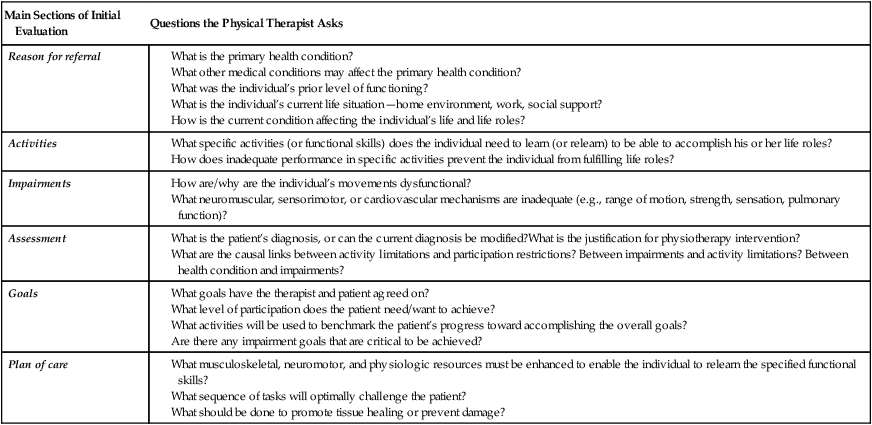
CHAPTER 4 After reading this chapter and completing the exercises, the reader will be able to: 1. Outline a model for organizing an initial evaluation based on a functional outcomes approach. 2. Identify the basic elements for each section of the initial evaluation format. 3. Describe the relationship between the American Physical Therapy Association’s Guide to Physical Therapist Practice patient/client management model and the sections of the initial evaluation format. 4. Categorize components of an initial evaluation into the initial evaluation format. 1. Documentation both shapes and reflects clinical problem-solving strategies. 2. A top-down model of disablement provides a useful framework for clinical problem solving, and thus documentation. 3. Documentation should be organized around functional outcomes. Two main formats for documentation are presented in this book: (1) a format for writing the initial evaluation of a patient and (2) a format for writing progress and treatment notes. Other types of documentation, such as discharge summaries, letters to referral sources, and others, can easily be constructed from these two main types. The major focus of this book is on the initial evaluation format because it is the most critical to establishing a framework for clinical decision making. Each section of the initial evaluation format is further detailed in separate chapters (Chapters 5 to 11). The format for progress and treatment notes is a modified form of the SOAP note (see Chapter 2) and is presented in Chapter 12. Practice exercises in categorizing statements into the different sections of the initial evaluation format are provided at the end of this chapter. The format for an initial evaluation is based on the top-down disablement model presented in Chapter 1. There are six main sections (Table 4-1). The first three sections include information related to the ICF framework: health condition and participation (Reason for Referral section), activities (Activities section), and body structures and functions (Impairments section). The next three sections present the diagnosis (Assessment), the Goals, and the Plan of Care. TABLE 4-1 Six Sections of the Initial Evaluation Format One of the important contributions of the Guide is the “patient/client management model.” This model describes the process by which a PT determines the critical problems that require intervention and develops an intervention plan to address those problems. The model defines five integrated elements of the process: examination, evaluation, diagnosis, prognosis, and intervention. The model is illustrated and each of the elements is defined in Figure 4-1. The initial evaluation format fits very closely with the patient/client management model (Table 4-2). In this format, examination and evaluation are combined. As is emphasized in the patient/client management model, evaluation is a dynamic process—not something that is initiated only after all data have been collected. Therefore there is an interplay between examination and evaluation. Data are collected and evaluated, and then decisions are made about what additional data to collect. This process often may involve hypothesis testing. In the functional outcomes approach the starting point for data collection is the Reason for Referral, which establishes both the primary reasons for referral and the patient’s participation restrictions. This then leads to specific examination procedures to determine which activities are related to the participation restriction and which impairments are leading to activity limitations. Thus the functional outcomes format applies a logical sequence to the reporting of the data that were collected. TABLE 4-2 Relationship of The Guide’s Patient/Client Management Model to the Documentation Format The critical step in clinical reasoning is establishing a diagnosis. The diagnosis establishes the causes of specific problems that the PT or PTA will address in the intervention strategy. Sometimes the diagnosis may be a statement of the nature and location of the health condition that is causing the problem. More commonly it is a statement of the causal links between impairments and activity limitations. Diagnosis is considered in more detail in Chapter 9. The following sections discuss each of the main components of the initial evaluation format in some detail. Each component is further detailed in Chapters 5 to 11, and case examples of complete intial evaluations can be found at the end of this chapter. Ideally, the format of your inital evaluation should guide your clinical decision making. Table 4-3 summarizes the evaluation process, emphasizing clinical decision making. This process uses a top-down model. After obtaining patient history and pertinent medical information, therapists ask patients about their participation restrictions, and then ascertain which activities are limited, and whether impairments exist in body structures and functions that contribute to these activity limitations and participation restrictions. This leads to a process of developing an assessment, which includes a diagnosis and prognosis, setting of goals, and developing a plan of care. TABLE 4-3 Process Used to Evaluate a Patient and Develop a Plan for Intervention The Reason for Referral typically entails a short narrative summary of the reason for evaluating a particular patient in physical therapy (see Chapters 5 and 6). This includes defining any previously established diagnosis and pertinent medical history, as well as the patient’s social history and current level of participation. This information is linked together in this one section as it provides the rationale for why the patient was referred for evaluation. The following two sections are therefore included in the reason for referral. Information in the Activities section is intended to identify the critical activity limitations that contribute to participation restrictions (see Chapter 7). What are the functional skills that (1) the individual needs to perform to fulfill his or her goals and required roles and (2) are they now in some way less than adequate? Activities should be reported concretely and completely and should be quantified to the degree possible. This can be done by use of quantifiable measurements (such as walking speed or distance walked), or by use of standardized tests that measure the activity level. This section identifies those impairments, such as range of motion limitations or strength deficits, that have a causal relationship to the observed activity limitations or might cause activity limitations in the future if not treated (see Chapter 8). This information should be documented using objective measures, such as degrees of range of motion or manual muscle testing grade, whenever possible. The Assessment section typically begins with an overall impression: a brief statement summarizing the patient’s reason for being referred for physical therapy. The PT then outlines a diagnosis that includes three components: differential diagnosis, classification based on etiology or movement system (if pertinent), and the relationship of the problem with activity limitations and participation restrictions (see Chapter 9). Normally this diagnosis will link either a health condition or impairment to activity limitations. APTA Guidelines for Physical Therapy Documentation state that a physical therapy diagnosis is required for all initial evaluations. The assessment concludes with a statement summarizing the PT’s recommendations and the necessity of physical therapy intervention (if applicable). This section identifies the expected outcomes of physical therapy intervention, the ends toward which physical therapy intervention is directed (see Chapter 10). Specific goals are written that are related to these outcomes. All goals must be measurable and must include a time frame. The goals can have several levels: • Participation goals: Typically one or two participation goals are useful to highlight the overall level of participation in work, social, recreational, and home activities that a patient is expected to achieve. • Activity goals: Activity goals state the predicted functional performance at the end of therapy. These goals must be related to a specific activity, skill, or task that can serve as a benchmark for an individual’s progress. • Impairment goals: Impairment goals document expected improvements or changes in impairments that will result at the end of therapy. These goals should have a clear relationship to the stated activity goals. For example, achieving a certain shoulder range of motion may be critical to the functional task of lifting or reaching. This section outlines the plan for achieving the goals listed in the previous section and presents a concise rationale for the intervention strategy chosen (see Chapter 11). It is useful to begin with the proposed frequency of treatments, as well as a tentative date for reevaluation. Many institutions mandate this approach. The intervention plan should then be documented in the following three categories: • Coordination and communication: Services that require coordination or communication with other providers, agencies, departments, and so on should be included here. • Patient-related instruction: The PT should document specific instruction or teaching of the patient or of the patient’s caregivers. • Direct interventions: These interventions are performed by the PT or PTA (e.g., therapeutic exercise, functional training, manual therapy techniques). (See Figure 11-1 for appropriate categorization and terminology from the Guide.) Four examples are included here to illustrate how the initial evaluation format might be used in actual practice.* Readers, especially beginning students, should not see this format as a rigid blueprint to be copied exactly in other situations. Rather, this format should be perceived as a starting point, a set of guidelines to be used for designing effective physical therapy documentation. Case Examples 4-1 through 4-4 show the variability in how the same format can be applied in different settings and for different patient populations. Some evaluations are shorter, some longer, and include different evaluative information (particularly in the Activities and Impairments sections) as is pertinent for each specific case.
Clinical Decision Making and the Initial Evaluation Format
Patient/Client Management Model
Components of the Initial Evaluation
Process
Examination/evaluation
Reason for referralParticipation
Explain medical and health conditions that are pertinent to patient’s current problems
Participation
Determine restrictions in participation in work or personal roles
Activities
Measure patient performance on the activities that the individual needs to perform to overcome or prevent participation restrictions
Impairments
Identify and measure the impairments that contribute to the observed functional activities
Diagnosis
Assessment
Establish a diagnosis and justify necessity of physical therapy intervention
Prognosis
Goals/plan of care
Develop a set of goals in consultation with the patient
Intervention
Plan of care
Plan an intervention strategy that will help the patient achieve the goals
A Description of the Initial Evaluation Format
REASON FOR REFERRAL
ACTIVITIES
IMPAIRMENTS
ASSESSMENT
GOALS
INTERVENTION PLAN
Case Examples
Clinical Decision Making and the Initial Evaluation Format