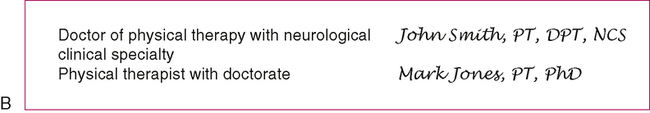
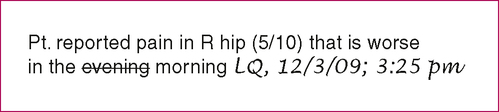
After reading this chapter, the reader will be able to: 1. List and describe the key aspects of physical therapy documentation as a legal record. 2. Use the correct method for signing notes and correcting errors in documentation. 3. Describe the Health Insurance Portability and Accountability Act (HIPAA) and the Privacy Rule and discuss the implication for physical therapy documentation. 4. Discuss the importance of appropriately documenting informed consent as part of a physical therapy evaluation. 5. Discuss the three legal reasons why a physical therapist’s documentation may be scrutinized. Several key legal aspects pertinent to physical therapy documentation are outlined below: • Legibility. Handwritten entries should be legible and written in ink. • Dated. All notes must be dated with the date that the note was written. Backdating is illegal and should never be done. It is recommended that all notes be written or dictated on the date that an evaluation or intervention is performed. If a note is not written on the date, then both the date of the evaluation/intervention and the date the report was written should be indicated. For notes in an interdisciplinary medical record, the time of treatment should also be recorded. • Authentication. All physical therapy documentation must be authenticated by a PT, or when appropriate, a physical therapy assistant (PTA). All notes must be signed, followed by the writer’s professional abbreviation, and dated. The American Physical Therapy Association House of Delegates (APTA HOD, 1999) has recommended use of standard professional designations: PT for physical therapists and PTA for physical therapist assistants (Figure 3-1, A). • Degrees and certifications. The APTA supports the following preferred order when a therapist or assistant has additional degrees or certifications (Figure 3-1, B). These are not relevant legally but are important to promote consistent communication throughout the profession: 2. Highest earned physical therapy-related degree 3. Other earned academic degree(s) 4. Specialist certification credentials in alphabetical order (specific to the American Board of Physical Therapy Specialties) 5. Other credentials external to APTA 6. Other certification or professional honors (e.g., FAPTA) (APTA HOD, 1999) • PTA authentication. PTAs can typically sign only treatment notes; all evaluations must be written and signed by a PT. Depending on individual state practice acts, PTs may be required to co-sign each note written by a PTA. • Student PT and PTA authentication. SPTs or SPTAs (individuals who are enrolled in a PT or PTA educational program) are allowed to write notes in the medical record. These notes must be signed and dated by the student and also must be authenticated by a supervising licensed PT or PTA (see also APTA Guidelines, Appendix A) (Figure 3-1, C). • Errors. If an error is made in a handwritten note or a printed copy of an electronic note, the therapist should place a single line through the erroneous word and write his or her initials near the crossed-out word. The date and time of correction should also be included (Figure 3-2). • Blank lines or spaces. Blank lines or large empty spaces should be avoided in the record. A single straight line should be drawn through any open spaces in a report. • Abbreviations. The writer should use only those abbreviations authorized by his or her facility (Appendix B provides a list of commonly used abbreviations in rehabilitation settings). Abbreviations should be kept to a minimum; if in doubt, write it out (see Chapter 2 for information on using abbreviations). Only information that is directly relevant to the patient’s medical condition, prognosis, or intervention plan should be documented in a medical record. Sometimes conflicts or personal issues arise between therapists and patients, and between patients and their physicians or other medical professionals. Generally, information of this nature should not be included in clinical documentation. Box 3-1 contains definitions of key documentation terms.
Legal Aspects of Documentation
Documentation as a Legal Record
KEY LEGAL ASPECTS OF PHYSICAL THERAPY DOCUMENTATION
INFORMATION TO INCLUDE IN A NOTE
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Legal Aspects of Documentation