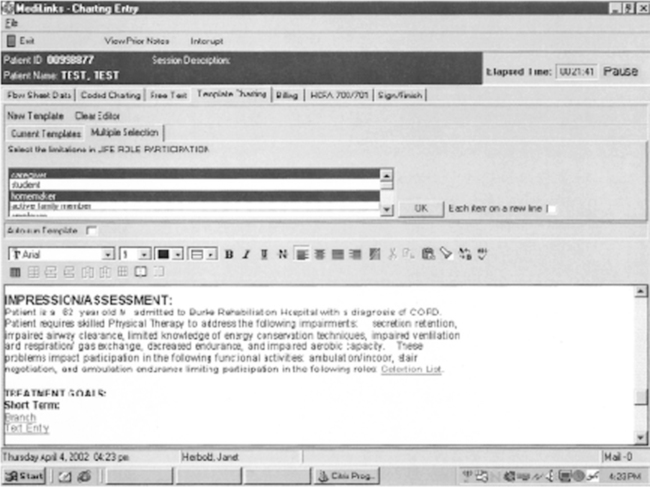
Inherent drawbacks to the pen and paper method of documentation include the following: • Legibility of the notes. Illegibly handwritten notes can lead to miscommunication, errors in practice, and denied payment. • Redundancy of medical and demographic information. Therapists frequently copy information written by another health care professional into their own notes. Components such as the patient’s diagnosis, date of birth, past medical history, and medications are frequently manually rewritten into therapy documentation. In addition, as the completion of regulatory forms such as the Inpatient Rehabilitation Form–Patient Assessment Instrument (IRF-PAI), the Minimum Data Set-Resource Utilization Groups (MDS-RUGS), and the Outcome and Assessment Information Set (OASIS) become necessary for reimbursement and payment, therapists and nurses must document both in the medical record as well as on the reimbursement form (Figure 15-1). Both practices result in redundancy and duplication of information at a time when efficiency of clinical practice and staff productivity are being scrutinized. • Difficulty with data retrieval for clinical research or outcomes analysis to promote evidence-based practice. It has become increasingly important to demonstrate treatment effectiveness through clinical research. With handwritten documentation it is very difficult and time consuming to manually review charts and analyze notes to determine the effectiveness of treatment techniques. In many cases, the variation in note-writing style and terminology makes it impossible to extract comparative data from handwritten notes from different clinicians even for the same type of patient condition. • Use of abbreviations. Abbreviations have been used for many years as a shortcut during handwritten documentation. This practice, although frequently time saving, can lead to errors in legibility and a multitude of terms meaning the same thing, thus creating confusion among clinicians. Some benefits of computerized documentation in physical therapy practice are listed in Box 16-1. Figure 16-1 illustrates these features in a software program (MediServe Information System, Chandler, Ariz.) with templates designed by a team of rehabilitation professionals (Burke Rehabilitation Hospital, White Plains, NY). In this example, the Impression/Assessment is coded to include key components, such as summarizing and drawing relationships between the patient’s impairments, activity limitations, and participation restrictions. All possible options for each of these components are listed as options in a pull-down menu (in this example, Life Role Participation). By using such a format, therapists are prompted to provide critical information so that it is always included in their documentation. Furthermore, the design of the template is structured so that the terminology is consistent with current practice and, importantly, the Guide to Physical Therapist Practice (American Physical Therapy Association, 2001).
Computerized Documentation
Drawbacks to Pen and Paper Documentation
Benefits of Computerized Documentation
STANDARDIZATION OF DATA ELEMENTS AND CHARTING PRACTICES
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Computerized Documentation
Only gold members can continue reading. Log In or Register to continue