Fig 5.1
Dislocated fracture of the medial clavicle, fixed by special clavicula plate
5.8.2 Fractures of the Middle Third of the Clavicle
More than 200 different methods of immobilization, bracing, or sling treatments have been devised for the nonoperative treatment of displaced fractures of the clavicle. The number of treatments attests to the extreme difficulty of achieving and maintaining reduction. Recommended periods of immobilization vary from 2 to 6 weeks, individualized to the patient’s comfort level. Secondary to the typical displacement of the lateral fragment with inferior and medial translation and anterior rotation, shoulder weakness and easy fatigability and thoracic outlet syndrome have been noted. There exists also an association between significant shortening (>15–20 mm) of the clavicle and symptomatic malunion.
5.8.2.1 Operative Treatment
Indication
Indications are open fractures, impending perforation of the skin, and fractures with associated vascular injury requiring surgical repair, relative indications are severe displacement and shortening.
Primarily, two widely accepted methods of fixation – plate fixation or intramedullary pinning – are used in the operative treatment of fractures of the middle third of the clavicle.
Plate Fixation
The approach is either straight over the clavicle or in the sagittal plane. For minimally invasive surgery, two incisions are made at each end of the plate. After dissection of the platysma the supraclavicular nerves are identified.
For plate fixation, dynamic compression plates, pelvic reconstruction plates, and anatomic precontoured plates have been used. Although their low profile may lead to less skin irritation, semitubular plates and mini-plates were found to be mechanically too weak for rigid fixation and are not recommended. Plate fixation has superior biomechanical strength that offers excellent rotational and length control and allows early weight bearing on the limb. The main disadvantages are the long skin incision and tissue dissection around the fracture, the hardware prominence, which may require plate removal, and possible refracture after the plate removal. As experience with precontoured “anatomic” plates and surgical technique increases, minimally invasive soft tissue handling can result in dramatic decreases in incision size. Intramedullary fixation offers the advantages of being a soft tissue friendly and minimally invasive or percutaneous procedure with the potential for improved cosmesis. The main disadvantages of the method of fixation (common to all “unlocked” intramedullary devices) are its inferior axial and rotational stability in nontransverse and comminuted fractures. The plate usually is placed on the superior aspect of the clavicle, because this placement has been shown to be the most advantageous biomechanically. An anterior approach is also possible. Whenever possible, branches of the supraclavicular nerves are identified, mobilized, and protected. A minimum of three bicortical screws are used distal and proximal to the fracture; a lag screw is placed whenever possible. Smaller fracture fragments (including a fairly consistent vertically oriented anterior cortical fragment) are “teased” into position without stripping all their soft tissue (Fig. 5.2).
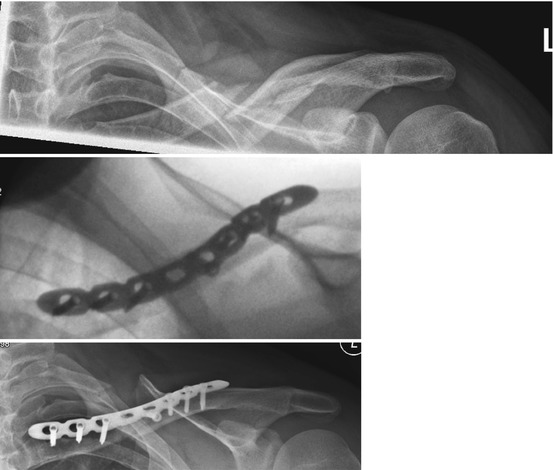
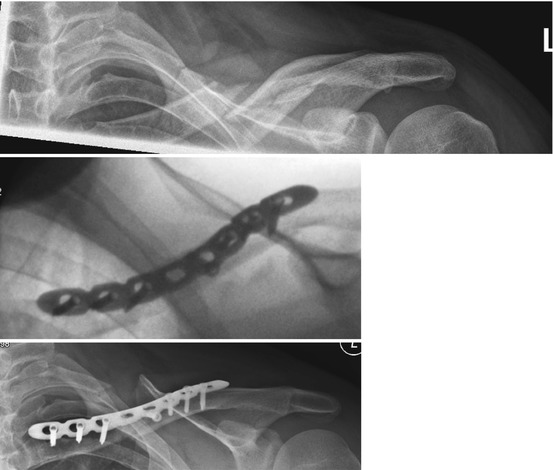
Fig. 5.2
Primary severe dislocated midshaft clavicle fracture fixed by an LCP
Elastic Stable Intramedullary Nailing
Intramedullary nailing has the advantage of being a minimally invasive or percutaneous procedure without disturbing the soft tissue. It also offers less pain and faster return to work, better functional results, and less shortening when compared with conservative treatment. The disadvantages are its inferior axial and rotational stability in nontransverse and comminuted fractures; in up to 30–40 % patients the clavicle diameter is too small for a closed procedure or closed reduction is not possible. Then it is necessary to open the fracture site [6, 7].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








