Sites of Involvement
Typically, chondroblastoma occurs in the epiphyses of the long bones. While the occurrence is typically at the end of the major tubular bones, it can also occur at a secondary ossification center, such as the greater trochanter.
More than 75 % of the cases develop at the epiphyseal and epimetaphyseal region of the distal and proximal femur, proximal tibia, and proximal humerus.
Chondroblastoma can also occur at the epiphyseal equivalent sites of the flat bone such as the acetabulum and iliac crest. Though rare, however, chondroblastoma may arise in the patella, calcaneus, or other tarsal bones which are one of the typical occurrence sites of the chondroblastoma.
Cases involving the craniofacial bone can be found in the base of the skull and temporal bone (Fig. 21.11).
Occasionally, multifocal synchronous chondroblastomas were reported.
Clinical Symptoms and Signs
A typical clinical presentation is localized pain. That may occur as a singular incident to prolonged episodes lasting several months or years.
In addition, the patient can also suffer from swelling, gait disturbances, and joint stiffness.
A few patients may also experience knee joint effusion.
Furthermore, tumoral involvement of the temporal bone may result in hearing loss, tinnitus, or vertigo.
On physical examination, patients usually report tenderness in the affected area along with limitation of motion and muscular atrophy.
Image Diagnosis
Radiographic Features
Chondroblastoma is usually located in the medullary portion and arises either at the epiphysis or apophysis of the long tubular bone (Fig. 21.12). Extension to the metaphysis can be seen at times (Fig. 21.1).

Fig. 21.1
The radiograph of the femural proximal end with a chondroblastoma located in the greater trochanter (an apophysis)
The size of chondroblastoma is usually less than 5–6 cm. Conventional radiographs typically demonstrate well-defined, geographic bone destruction with either a spherical or an oval shape (Fig. 21.2).

Fig. 21.2
The radiograph of the femoral head shows a round osteolytic bone lesion at the subchondral portion. The lesion is confined to the epiphysis
There are amorphous calcific foci within the lesion. In rare cases, extensive calcifications can be seen on plain radiograph. The lesion shows a marginal sclerotic rim on plain radiograph, and it shows expansion of the cortex with periosteal reaction in cases of extension to the cortex (Fig. 21.3).
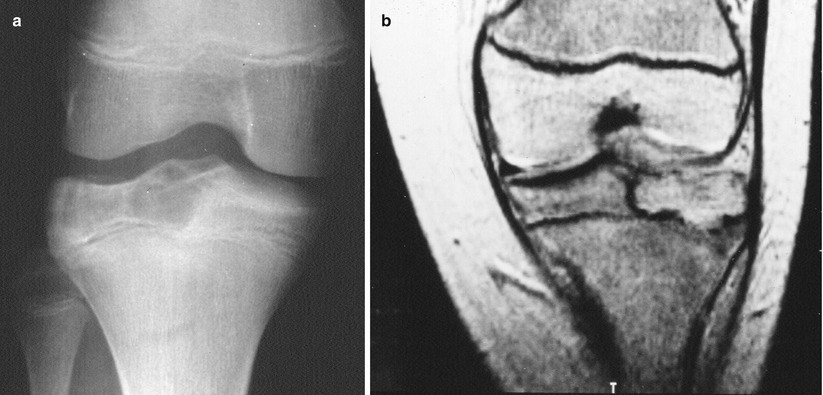
Fig. 21.3
Radiograph (a) and MRI (b) of a knee show an epiphyseal lytic lesion bordered by sclerotic bone rim
However, pathological fracture is not frequently seen. In a typical case, the contour of the involved bone is not usually changed.
MRI Features
On MR imaging, chondroblastoma shows low signal intensity on T1-weighted images and variable signal intensity on T2-weighted images. Sometimes, the lesion shows perilesional high signal intensity on T2-weighted images, indicating inflammatory or edematous changes.
Image Differential Diagnosis
Giant Cell Tumor
Most giant cell tumors develop in skeletally mature adult patients. Radiographically, chondroblastoma shows a more distinct delineation than giant cell tumors which typically lack a reactive sclerotic margin.
Clear Cell Chondrosarcoma
Is a more aggressive lesion, frequently expanding the bone and permeating the cortex
Pathology
Gross Features
Since chondroblastoma is usually small, it is treated by curettage.
Grossly, it appears as fragments of soft pink to gray tumor tissue with occasional zones of hemorrhage and calcification.
Small cystic spaces can be commonly found.
On rare occasions, the boundary of the resected specimen is well delineated and a sclerotic rim is observed.
Occasionally, the cystic change is so prominent that it resembles an aneurysmal bone cyst.
Histological Features
Histologically, the basic cells are chondroblast. Typical chondroblasts are oval shaped and have well-defined cytoplasmic border. They are rather uniform round to polygonal in shape (Fig. 21.4). The cytoplasm ranges from pink to focally clear and with distinct cell borders (Fig. 21.5).
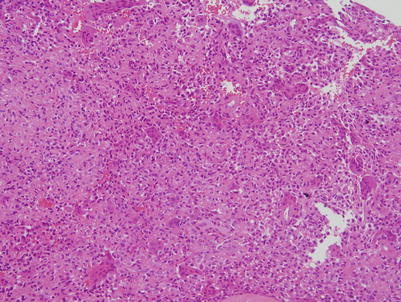
Fig. 21.4
At low-power view, there are numerous giant cells and oval-shaped chondroblasts
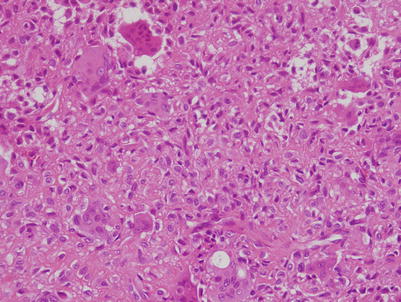
Fig. 21.5
High power illustrating oval-shaped chondroblasts with central groove and giant cells
The nucleus is located in the central portion of the cytoplasm and is oval or round shaped. A longitudinal groove is typical, accounting for the so-called “coffee bean” appearance. There is one or two inconspicuous nucleolus. Usually chondroblasts are packed in pseudo-lobulated sheets.
There are randomly distributed multinucleated giant cells which have 5–40 nuclei. Another diagnostic clue is immature chondroid matrix that appears as variably sized nodules composed of light-staining, amorphous, bluish to eosinophilic material surrounded by chondroblasts (Figs. 21.6 and 21.7).
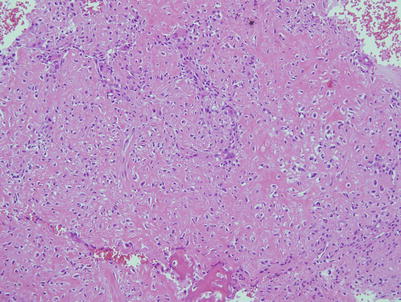
Fig. 21.6
Chondroblastoma shows eosinophilic to amorphous pink fibrochondroid matrix
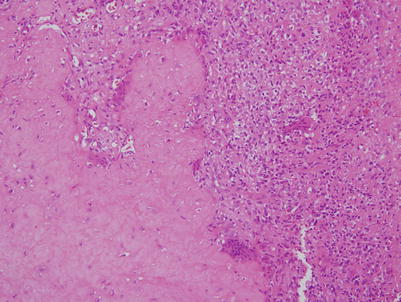
Fig. 21.7
Occasionally, this pink matrix shows acellular lobulated appearance
Mature hyaline cartilage is very rarely present. Ossification can occur, occasionally abundant. Especially, this kind of ossification is frequently observed in talus and calcaneus lesions. A fine network of pericellular calcification is found around the degenerating tumor cells, which is often called “chicken wire calcification” (Figs. 21.8 and 21.9).
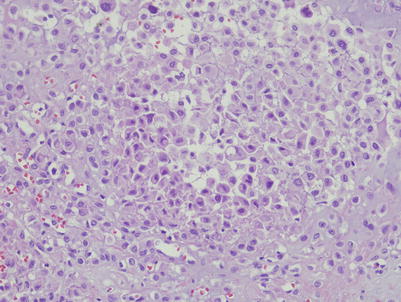
Fig. 21.8
Typical example of chickenwire calcification showing pericellular thin lines of calcification
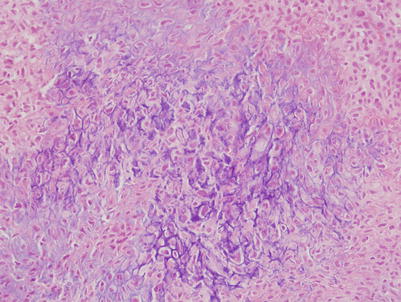
Fig. 21.9
In this area, more dense mineralization is present, with suggestive “chickenwire” pattern.
Mitosis can be found in the mononuclear cells, although uncommon. Atypical mitosis is extremely infrequent.
Often individual chondroblasts can show considerable cytologic atypia such as enlarged, irregular, and hyperchromatic nuclei. However, this finding is not indicative of malignant disease and has no impact on patient prognosis.
Focally spindle cell change can be seen in chondroblastoma and it is very difficult to diagnose. Brown to yellow granular pigment is frequently observed in skull chondroblastomas, which serves as a very useful feature for diagnosis. These are iron-staining positive.
Secondary aneurysmal bone cystic change is present in about one-third of chondroblastomas (Fig. 21.10). In most cases, this cystic change is observed at the microscopic level.
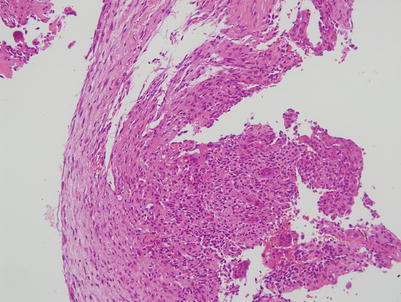
Fig. 21.10
Secondary aneurysmal cystic changes are evident
Fig. 21.11
Radiograph (a) and CT scan (b) of a chondroblastoma located in a temporal bone
Fig. 21.12
Radiograph (a) and CT scan (b) of a chondroblastoma in a femoral condyle. Lytic lesion with mottled calcified spots and peripheral sclerotic rim
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








