Cervical Spine
EPIDEMIOLOGY
Cervical spine injuries usually occur secondary to high-energy mechanisms, including motor vehicle accidents (45%) and falls from a height (20%).
Less commonly, cervical spine injuries occur during athletic participation (15%), most notably during American football and diving events, and as a result of acts of violence (15%).
Neurologic injury occurs in 40% of patients with cervical spine fractures.
Spinal cord damage is more frequently associated with lower rather than upper cervical spine fractures and dislocations.
Approximately 2% to 6% of trauma patients sustain a cervical spine fracture.
Between 19% and 51% of cases of spinal cord trauma involve the cervical region.
Twenty percent of trauma patients who present with a focal neurologic deficit will have an associated cervical spine fracture.
ANATOMY
The atlas is the first cervical vertebra, which has no body. Its two large lateral masses provide the only two weight-bearing articulations between the skull and the vertebral column.
The tectorial membrane and the alar ligaments are the key to providing normal craniocervical stability.
The anterior tubercle is held adjacent to the odontoid process of C2 by the transverse ligament of the atlas (Gray’s Anatomy).
About 50% of total neck flexion and extension occurs between the occiput and C2, 25 degrees at occiput-C1, and 20 degrees at C1-C2.
The vertebral artery emerges from the foramen transversarium and passes between C1 and the occiput, traversing a depression on the superior aspect of the C1 ring. Fractures are common in this location.
The axis is the second cervical vertebra, whose body is the largest of the cervical vertebrae as it incorporates the odontoid process (dens).
Transverse ligament of the atlas (horizontal band of the cruciform ligament) provides primary support for the atlantoaxial joint.
The alar ligaments are secondary stabilizers of the atlantoaxial joint.
The facet joint capsules at occiput-C1 and C1-C2 provide little support.
Fifty percent of total neck rotation occurs at the C1-C2 junction.
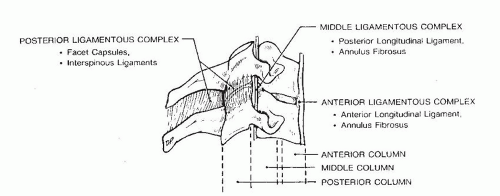
C3-C7 can be conceptualized as a three-column system (Denis) (Fig. 9.1):
Anterior column: The anterior vertebral body and intervertebral disc resist compressive loads, while the anterior longitudinal ligament and annulus fibrosis are the most important checkreins to distractive forces (extension).
Middle column: The posterior vertebral body and uncovertebral joints resist compression, while the posterior longitudinal ligament and annulus fibrosis limit distraction.
Posterior column: The facet joints and lateral masses resist compressive forces, while the facet joint capsules, interspinous ligaments, and supraspinous ligaments counteract distractive forces.
The vertebral artery enters the foramen transversarium of C6 and ascends through the foramina transversarium to C1. Injuries to the vertebral arteries are uncommon because of the redundancy of the vessel.
MECHANISM OF INJURY
Motor vehicle accidents (primarily in young patients), falls (primarily in older patients), diving accidents, and blunt trauma account for the majority of cervical spine injuries.
Forced flexion or extension resulting from unrestrained deceleration forces, with or without distraction or axial compression, is the mechanism for most cervical spine injuries.
CLINICAL EVALUATION
1. Patient assessment is indicated: airway, breathing, circulation, disability, and exposure (ABCDE).
Airway patency is the first priority.
Breathing or adequate ventilation is the next priority.
Circulation or recognition of the shock state is the next priority.
Disability refers to doing a brief neurologic examination.
Exposure is the final part of the initial examination. Completely undress the patient and maintain body temperature.
2. Initiate resuscitation: Address life-threatening injuries. Maintain rigid cervical immobilization.
3. Tracheal intubation and central line placement are often performed in the emergency setting. During intubation, manipulation of the neck can potentially displace unstable cervical fractures or dislocations. Manual in-line stabilization should be maintained throughout the intubation process. Alternatively, mask ventilation can be continued until fiberoptic or nasotracheal intubation can be safely performed. If an unstable spine is highly suspected, a cricothyroidotomy may be the safest alternative for airway control.
4. Evaluate the level of consciousness and neurologic impairment: Use the Glasgow Coma Scale (see Chapter 2).
5. Assess head, neck, chest, abdominal, pelvic, and extremity injury.
6. Ascertain the patient’s history: Query for mechanism of injury, witnessed head trauma, movement of extremities/level of consciousness immediately following trauma, etc.
7. Perform a physical examination.
Neck pain
Lacerations and contusions on scalp, face, or neck
8. Perform a neurologic examination.
Cranial nerves
Complete sensory and motor examination
Upper and lower extremity reflexes
Rectal examination: perianal sensation, rectal tone
Bulbocavernosus reflex (see Chapter 8)
RADIOGRAPHIC EVALUATION
Lateral cervical spine radiograph: This will detect 85% of cervical spine injuries. One must visualize the atlantooccipital junction, all seven cervical vertebrae, and the cervicothoracic junction (as inferior as the superior aspect of T1). This may necessitate downward traction
on both upper extremities or a swimmer’s view (upper extremity proximal to the x-ray beam abducted 180 degrees, axial traction on the contralateral upper extremity, and the beam directed 60 degrees caudad). Patients complaining of neck pain should undergo complete radiographic evaluation of the cervical spine, including anteroposterior (AP) and odontoid views. On the lateral cervical spine radiograph, one may appreciate:
1. Acute kyphosis or loss of lordosis
2. Continuity of radiographic “lines”: anterior vertebral line, posterior vertebral line, facet joint line, or spinous process line
3. Widening or narrowing of disc spaces
4. Increased distance between spinous processes or facet joints
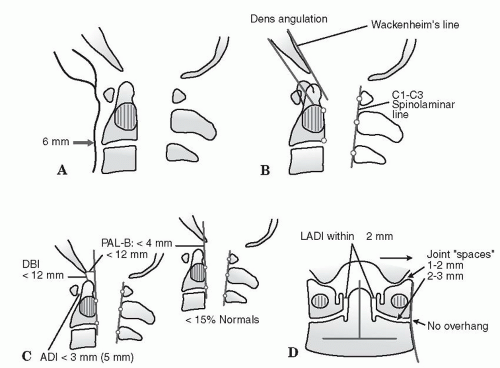
5. Prevertebral soft tissue swelling, which depends on the level in question, or an abnormal contour of the tissues (Fig. 9.2):
At C1: >10 mm
At C3, C4: >7 mm
At C5, C6, C7: >20 mm
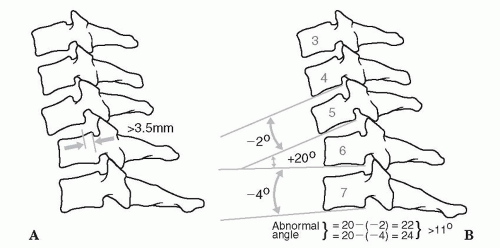
6. Radiographic markers of cervical spine instability, including the following (Fig. 9.3):
Compression fractures with >25% loss of height
Angular displacements >11 degrees between adjacent vertebrae (as measured by Cobb angle)
Translation >3.5 mm
Computed tomography (CT) scans and/or magnetic resonance imaging (MRI) may be valuable to assess the upper cervical spine or the cervicothoracic junction. CT scanning has largely replaced conventional radiography. CT scans and MRI are particularly important in the evaluation of the intoxicated and obtunded patient (see Chapter 2).
The proposed advantages of CT scans over a lateral cervical film as an initial screening tool are that it is more sensitive for detecting fractures and more consistently enables assessment of the occipitocervical and cervicothoracic junctions. A potential disadvantage of CT scans as an initial radiographic assessment is that subtle malalignment, facet joint gapping, or intervertebral distraction is difficult to assess using axial images alone.
The most useful applications of MRI are in detecting traumatic disc herniation, epidural hematoma, spinal cord edema or compression, and posterior ligamentous disruption. An additional application of MRI is the ability to visualize vascular structures. MR arteriograms can be used to assess the patency of the vertebral arteries.
Stress flexion/extension radiographs rarely, if ever, should be performed if instability is suspected; they should be performed in the awake and alert patient only. In a patient with neck pain, they are best delayed until spasm has subsided, which can mask instability.
The atlantodens interval (ADI) should be <3 mm in adults and <5 mm in children.
Traction x-rays are taken during reductions only.
CLASSIFICATION
Orthopaedic Trauma Association Classification of Cervical Spine Injuries
See Fracture and Dislocation Classification Compendium at http://www.ota.org/compendium/compendium.html.
INJURIES TO THE OCCIPUT-C1-C2 COMPLEX
As with other transitional regions of the spine, the craniocervical junction is highly susceptible to injury. This region’s vulnerability to injury is particularly high because of the large lever-arm induced cranially by the skull and the relative freedom of movement of the craniocervical junction, which relies disproportionately on ligamentous structures rather than on intrinsic bony stability.
Occipital Condyle Fractures
These are frequently associated with C1 fractures as well as cranial nerve palsies.
The mechanism of injury involves compression and lateral bending; this causes either compression fracture of the condyle as it presses against the superior facet of C1 or avulsion of the alar ligament with extremes of atlantooccipital rotation.
A CT scan is frequently necessary for diagnosis.
CLASSIFICATION (FIG. 9.4)
Type I: Impaction of condyle; usually stable
Type II: Shear injury associated with basilar or skull fractures; potentially unstable
Type III: Condylar avulsion; unstable
Treatment includes rigid cervical collar immobilization for 8 weeks for stable injuries and halo immobilization or occipital-cervical fusion for unstable injuries.
Craniocervical dissociation should be considered with any occipital condyle fracture.
Occipitoatlantal Dislocation (Craniovertebral Dissociation)
This is almost always fatal, with postmortem studies showing it to be the leading cause of death in motor vehicle accidents; rare survivors
have severe neurologic deficits ranging from complete C1 flaccid quadriplegia to mixed incomplete syndromes such as Brown-Séquard.
This is twice as common in children, owing to the inclination of the condyles.
It is associated with submental lacerations, mandibular fractures, and posterior pharyngeal wall lacerations.
It is associated with injury to the cranial nerves (the abducens and hypoglossal nerves are most commonly affected by craniocervical injuries), the first three cervical nerves, and the vertebral arteries.
The cervicomedullary syndromes, which include cruciate paralysis as described by Bell and hemiplegia cruciata initially described by Wallenberg, represent the more unusual forms of incomplete spinal cord injury and are a result of the specific anatomy of the spinal tracts at the junction of the brainstem and spinal cord. Cruciate paralysis can be similar to a central cord syndrome, although it normally affects proximal more than distal upper extremity function. Hemiplegia cruciata is associated with ipsilateral arm and contralateral leg weakness.
Mechanism is a high-energy injury resulting from a combination of hyperextension, distraction, and rotation at the craniocervical junction.
The diagnosis is often missed, but it may be made on the basis of the lateral cervical spine radiograph:
The tip of odontoid should be in line with the basion.
The odontoid-basion distance is 4 to 5 mm in adults and up to 10 mm in children.
Translation of the odontoid on the basion is never >1 mm in flexion/extension views.
Powers ratio (BC/OA) should be >1 (Fig. 9.5).
In adults, widening of the prevertebral soft tissue mass in the upper neck is an important warning sign of significant underlying trauma and may be the only sign of this injury.
Fine-cut CT scans with slices no more than 2 mm wide are helpful to understand articular incongruities or complex fracture patterns more clearly. MRI of the craniovertebral junction is indicated for patients with spinal cord injury and can be helpful to assess upper cervical spine ligamentous injuries as well as subarachnoid and prevertebral hemorrhage.
Classification based on the position of the occiput in relation to C1 is as follows:
Type I: Occipital condyles anterior to the atlas; most common
Type II: Condyles longitudinally dissociated from atlas without translation; result of pure distraction
Type III: Occipital condyles posterior to the atlas
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree