Samuel P. Thampi
Travis R. von Tobel
Monica Habib
![]()
27: Cervical Radiculopathy
![]()
PATIENT CARE
GOALS
Evaluate and develop a rehabilitative plan of care for the patient with a cervical radiculopathy that is compassionate, appropriate, and effective.
OBJECTIVES
1. Perform a detailed history and physical examination of the adult with a cervical radiculopathy.
2. Identify the psychosocial and vocational implications of cervical radiculopathy.
3. Identify the key components of a rehabilitation program for the patient with cervical radiculopathy and formulate a sample rehabilitation treatment plan.
Comprehensive assessment of the adult with cervical radiculopathy involves close attention to the following:
 The duration of the pain (years/months/weeks)
The duration of the pain (years/months/weeks)
 The mode of onset (motor vehicle accident/job-related accident/insidious): In case of a motor vehicle accident, obtain history of specifics of the accident such as date of accident, restraint used if any, driver versus passenger, front-end collision/rear-end collision/side-impact collision
The mode of onset (motor vehicle accident/job-related accident/insidious): In case of a motor vehicle accident, obtain history of specifics of the accident such as date of accident, restraint used if any, driver versus passenger, front-end collision/rear-end collision/side-impact collision
 The location of pain: It is important to note if the pain is located on the right side, left side, or both, as you need to correlate the symptoms with the physical examination signs and radiological findings
The location of pain: It is important to note if the pain is located on the right side, left side, or both, as you need to correlate the symptoms with the physical examination signs and radiological findings
 Radiation of pain: Radicular pain is a common presentation in cervical radiculopathy. This is in contrast to axial pain as seen in facet and/or myofascial pain syndrome
Radiation of pain: Radicular pain is a common presentation in cervical radiculopathy. This is in contrast to axial pain as seen in facet and/or myofascial pain syndrome
 Neurologic symptoms: Evaluate of symptoms of tingling, numbness, weakness or bowel/bladder symptoms
Neurologic symptoms: Evaluate of symptoms of tingling, numbness, weakness or bowel/bladder symptoms
 Quality of pain
Quality of pain
 Intensity of pain
Intensity of pain
 Aggravating factors
Aggravating factors
 Alleviating factors
Alleviating factors
 Neck trauma associated with neck pain
Neck trauma associated with neck pain
 Ask if this is the first time that the pain has occurred or if this is an exacerbation of an ongoing neck pain
Ask if this is the first time that the pain has occurred or if this is an exacerbation of an ongoing neck pain
 Functional impact of the neck pain on activities such as driving, work, reading, sexual activity
Functional impact of the neck pain on activities such as driving, work, reading, sexual activity
 Diagnostic tests and treatments prior to current visit to physiatrist
Diagnostic tests and treatments prior to current visit to physiatrist
In reviewing the past medical history, it is important to ask about unplanned weight loss, fever, chills, and night sweats as malignancies and infections can present with neck pain. It is also important to ask about kidney disease, stomach ulcers, liver disease, and bleeding diathesis as these can be important considerations in planning treatment. For example, epidural injections can cause epidural hematomas in patients with platelet deficiency.
In past surgical history ask about prior spine surgeries, including the level of surgery and type of surgical instrumentation. Spinal fusion can lead to early degeneration in the levels above and below the level of fusion.
In family history, it is important to ask about history of malignancies.
When taking a social, vocational history, it is useful to inquire about the type of work the patient does, if working, and hobbies that have been limited because of the neck pain.
A listing of current drug allergies and medications should be made.
Physical examination consists of inspection, palpation, range of motion assessment, motor strength testing of key muscle groups, sensory examination, and special tests.
On inspection, the physiatrist should evaluate the cervical spine and upper extremities for any abnormal skin markings, scars, masses, alignment and bony deformities, erythema, and atrophy. Superficial and deep palpation should be performed with focus on tenderness of muscles, tendons, and bony structures of the spine and upper extremities. Active and passive range of motion values for the cervical spine and upper extremities should be recorded and compared against normal values. Table 27.1 provides some normative data for movement of the cervical spine.
TABLE 27.1 Range of Motion Cervical Spine (Measured by Goniometer)
| NORMAL (°) |
Flexion | 60 |
Extension | 50 |
Side bending, right | 45 |
Side bending, left | 45 |
Lateral rotation, right | 80 |
Lateral rotation, left | 80 |
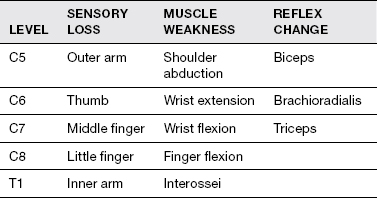
Relevant neurological examination consists of (a) sensory examination of the upper and lower extremities in key dermatomes using light touch and pinprick, (b) manual muscle testing of key muscle groups of the upper and lower extremities, and (c) muscle stretch reflexes in both upper and lower extremities (Table 27.2). It is important to check for evidence of upper motor neuron pathology as manifested by brisk reflexes, clonus, Hoffman sign in the upper extremity, and Babinski sign in the lower extremity.
Spurling test is used to assess root compression. The test involves turning the head to the affected side and applying downward pressure. The test is positive if the patient experiences increased pain into the shoulder and into the hand in a radicular pattern. The sensitivity of the Spurling test to nerve root pathology on CT scan was 95% and specificity was 94% (1). One has to observe for facet joint line tenderness and myofascial trigger points.
IMPAIRMENTS, ACTIVITY LIMITATIONS, AND PARTICIPATION RESTRICTIONS ASSOCIATED WITH CERVICAL RADICULOPATHY
Impairments associated with cervical radiculopathy include decreased range of motion of the neck, weakness, and decreased sensation in the neck and upper extremities. These impairments can limit activities such as driving, overhead movements, and lifting, which can in turn restrict ability to work and engage in avocational activities. Neck pain at night can impair sleep, leading to daytime drowsiness.
TABLE 27.2 Neurologic Deficits in Radiculopathies
Psychosocial implications due to cervical radiculopathy can include anxiety and depression due to the limitations in social activities and hobbies with friends and family. Work restrictions can lead to loss of/decreased productivity, reduction in wages, and even potential loss of employment. Prescription drug overdose and prescription drug diversion can also be potential problems.
TREATMENT PLAN FOR THE PATIENT WITH NECK PAIN
The treatment plan for neck pain is developed once an accurate diagnosis has been made. The differential diagnosis of neck pain is quite broad; however, some examples include the following: (a) myofascial pain syndrome, (b) cervical radiculopathy, (c) facet joint pathology, (d) cervical spinal stenosis, (e) cancer (primary vs. metastatic disease), (f) infectious, and (h) systemic (e.g., rheumatoid arthritis). Diagnosis is based on a combination of factors that include the history and physical examination as well as appropriate imaging and electrodiagnostic studies as needed. It is not uncommon to have one or more concurrent diagnoses such as cervical radiculopathy, myofascial pain, and degenerative disease of the spine.
The treatment plan for nociceptive and/or neuropathic pain originating in the neck that is noninfectious or nonmalignant in nature often includes a combination of interventions such as (a) medications (e.g., steroids, nonsteroidal anti-inflammatory drugs, muscle relaxants, antiepileptics, opioids), (b) injections (e.g., trigger point injections, spinal injections—epidural, transforaminal, medial branch blocks), (c) physical therapy, (d) chiropractic care, and (e) acupuncture.
MEDICAL KNOWLEDGE
GOALS
Demonstrate knowledge of established and evolving biomedical, clinical, and epidemiological sciences pertaining to cervical radiculopathy, as well as the application of this knowledge to guide holistic patient care.
OBJECTIVES
1. Describe the anatomy, physiology, and pathophysiology of cervical radiculopathy.
2. Identify the pertinent laboratory and diagnostic studies important in the evaluation of cervical radiculopathy.
3. Review the treatment of cervical radiculopathy.
Cervical radiculopathy is a disorder in which conduction along the nerve root is blocked, resulting in objective neurologic signs such as numbness or weakness, and/or a condition in which the blood supply to a nerve root is compromised, resulting in paresthesias (2).
Cervical radiculopathy is a very common cause of neck pain in the United States, and is one of the most common reasons for a patient to seek physician care. The most frequently presenting symptom is pain, although not all patients with cervical radiculopathy will have pain, especially in medial disc protrusion (3). There are many potential pain generators in the cervical spine. They include the intervertebral disc, the facet joint, the atlanto-occipital joint, the ligaments of the muscles, and the bone of the cervical spine region. The intracanalicular structures include the meninges, blood vessels, and the neural tissue of the spinal cord. There are 7 cervical vertebrae and 8 cervical nerve roots. The intervertebral discs are located between the vertebral bodies of C2 to C7. Each intervertebral disc is composed of an outer annulus fibrosis and an inner gelatinous nucleus pulposus, providing transmission of axial loads to dissipate forces throughout various ranges of motion. Apart from the nerve roots, structures such as the intervertebral discs, zygapophyseal joint, posterior longitudinal ligament, and the muscles can also serve as pain generators and produce somatic referral of pain into the upper limb. Biomechanical and/or biochemical insults to nonneural structures can trigger nociceptive nerve fibers via stretching, compression, or inflammation, causing pain referral. Mechanical stimulation of the cervical zygapophyseal joints or their innervating nerves is well documented in studies to produce head and neck pain with upper limb referral patterns.
After a thorough history and physical is obtained, imaging studies should be performed to diagnose the etiology of the cervical radiculopathy. Imaging should begin with basic anteroposterior (AP) and lateral x-rays to evaluate vertebral body alignment and disc space height, evaluate facet joints for arthritis, and exclude bony lesions (lytic and blastic), and then progress to a CT or MRI if appropriate diagnosis is still unclear.
Plain radiographs have limited value in diagnosing etiology of cervical radiculopathy, as these studies focus primarily on the bony structures. Thus, MRI remains the gold standard in imaging for cervical radiculopathy, as it can accurately visualize all soft-tissue structures within the cervical spine.
The author follows a simple “ABC” approach to reviewing an MRI of the cervical spine looking for
A | = | Alignment: Evaluate for spondylolisthesis. |
B | = | Bone: Evaluate for bony infiltrates due to metastasis, infections, or fractures. |
C | = | Canal/Cord: Evaluate for central canal stenosis and spinal cord myelomalacia. |
Then at each level, look for disc pathology, epidural lesions, facet hypertrophy, and foraminal stenosis.
Electrodiagnosis has a role in evaluating radiculopathy. It can help localize a nerve injury (e.g., cervical root), determine its severity, determine if it is acute or chronic, and provide some information regarding prognosis for recovery. Laboratory studies such as uric acid or rheumatoid factor, erythrocyte sedimentation rate (ESR), and C-reactive protein can evaluate for inflammatory arthropathy.
Once the diagnosis is made, various treatment options can be considered. Initial care should focus on controlling pain and inflammation to curb the injury response and ensure participation in a functional restoration program. Nonsteroidal anti-inflammatory drugs (NSAIDs) should be initiated early to reduce the inflammatory response and the release of thromboxane and prostaglandins. Muscle relaxants, antineuropathic agents, and antidepressants can be used as adjuvants for pain control. Opiates can be used as a modality; however, they carry the risk of opiate-induced morbidity and mortality. Initially, the patient should be advised to avoid any actions that aggravate the symptoms. Physical therapy should be initiated soon after the pain symptoms begin to diminish and should include modalities such as massage, superficial and deep heat, and electrical stimulation. Use of a soft cervical collar remains controversial and may be beneficial for short periods of time, but may cause atrophy-related immobilization if used excessively. Transcutaneous electrical nerve stimulation (TENS) may also be used to modulate musculoskeletal pain. Once the acute pain symptoms have resolved, proper spinal biomechanics should be emphasized, and therapy should focus on proper movement patterns. Proprioceptive training, balance, and postural conditioning should be incorporated into the patient’s therapy regimen. Once the patient is entirely pain free and able to perform a full cervical range of motion, then dynamic exercises can be initiated.
Unfortunately, a subset of patients with cervical radiculopathy will not improve with general physical therapy and modalities, and interventional spine techniques will need to be considered. Cervical steroid injections can be considered in the treatment of radicular pain. Cervical epidural steroid injections (i.e., interlaminar and transforaminal epidurals) can be performed under radiographic guidance. Transforaminal epidural steroid injections can be utilized to both diagnose and treat the radiculopathy. Cervical transforaminal epidural steroid injections carry a high risk for spinal cord and brain infarction. Particulate steroid can act as an embolus. Inadvertent intravascular injection of the blood vessels in the vicinity of the transforaminal can compromise the blood supply to the spinal cord and the brain. Approximately one-third of patients with cervical radiculopathy who are treated nonoperatively have persistent symptoms, and should be referred to a surgical spine specialist for consideration of surgical intervention (4).
PRACTICE-BASED LEARNING AND IMPROVEMENT
GOALS
Demonstrate competence in continuously investigating and evaluating patient care practices for cervical radiculopathy, appraising and assimilating scientific evidence, and continuously improving patient care practices based on constant self-evaluation and lifelong learning.
OBJECTIVES
1. Describe key components of self-assessment and lifelong learning for the physiatrist with respect to continuing professional development as related to cervical radiculopathy.
2. Describe the importance of clinical reflection in the professional growth of the physiatrist taking care of a patient with cervical radiculopathy.
3. Identify resources, including websites and professional organizations, for clinical guidelines, evidence-based practice, and continuing medical education and professional development as it pertains to cervical radiculopathy.
4. Describe the key elements of effective patient education methodology as it applies to the care of the patient with cervical radiculopathy, as well as educating families, residents, and the interdisciplinary team.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




