Cervical Osteotomy
Justin W. Miller
Rick C. Sasso
Techniques for spinal osteotomy have evolved over the past 75 years, and although basic principles remain the same, certain technical advances have occurred. Smith-Petersen et al. (7) were among the first to describe such techniques with their series of posterior lumbar osteotomies in 1945. LaChapelle (2) followed soon thereafter with his description of staged anterior and posterior lumbar osteotomies in 1946. Mason et al. (3) described his osteotomy of the cervical spine in 1953.
In 1972, Simmons (6) popularized the idea that cervical osteotomy could be performed in ankylosing spondylitis (AS) patients under local anesthesia with continuous neurologic monitoring. Urist (8) is credited with first describing this awake-sitting technique under local anesthesia in 1958. Urist also recommended that the osteotomy occur at the C7-T1 junction if possible. There are several benefits of performing the osteotomy at the cervicothoracic junction: (a) the spinal canal is relatively wide with more space available for the neural elements, (b) damage to the cord and/or nerve roots at this level would be less catastrophic than if in the midcervical region, and (c) the risk of injuring the vertebral artery is less, as the artery typically passes anterior to the transverse processes in this region.
Simmons (6) advocated a posterior wedge-shaped osteotomy to perform the correction. Removal of the lamina and spinous processes from C6 to T1 is done. Facetectomies are performed bilaterally to widely expose the C8 nerve roots. The head is extended in order to perform an osteoclasis of the anterior and middle columns of the cervical spine with the instantaneous axis of rotation at the base of the C7 pedicle. This causes lengthening of the anterior spine while the posterior elements are shortened. No instrumentation was used, and a halo was applied until fusion occurred. This technique was associated with a 4% mortality and 2% incidence of nerve root lesions.
Bohlman (1) expanded on Simmons’ cervical osteotomy technique with the addition of instrumentation to stabilize the cervical spine after the osteotomies were performed. Bohlman utilized a small Luque rectangle with Drummond wires and buttons supplemented by autograft. Patients, however, were still immobilized postoperatively in halo vests. Like Simmons and Urist, Bohlman preferred to perform his osteotomy at the C7-T1 junction.
In order to limit the possibility of sagittal translation during the Simmons osteotomy technique, Mehdian and Arun (4) devised a more controlled method of reduction at the osteotomy site. The Mehdian method involves the use of a posterior cervicothoracic screw-rod system that is implanted prior to completion of the osteotomy. Provisional, malleable rods are temporarily inserted. These rods allow the thoracic pedicle screws to slide along the rod as the reduction is performed without allowing translation. This allows for a more controlled reduction maneuver before the definitive titanium rods are placed.
INDICATIONS/CONTRAINDICATIONS
The primary indication for cervical osteotomy is the correction of a fixed cervical kyphotic deformity. This can occur in patients with AS, previous trauma, or prior surgery. This deformity may result in difficulty with activities of daily living, respiratory compromise, difficulty eating, loss of horizontal gaze, and/or disabling pain. Cervical osteotomy is contraindicated when the major deformity is in the thoracolumbar spine, when a flexion contracture of the hip is present, or if the cervical kyphosis is flexible. Other general contraindications include significant medical comorbidities that would prohibit normal recovery and rehabilitation.
PREOPERATIVE PREPARATION
Patient Evaluation
Medical comorbidities should be noted, evaluated, and optimized. Special attention should ensure that the cardiopulmonary status of the patient is satisfactory to undergo a spinal reconstructive procedure. Patients with AS, for instance, often have significantly restricted chest expansion due to ankylosed costovertebral joints. The surgeon should be aware of such issues.
Routine preoperative lab work should exclude anemia and coagulopathy. We recommend a lengthy discussion with the patient regarding the potential risks and benefits of surgery. Major surgical risks of cervical osteotomy include dysphagia, infection, malunion, nonunion, neurologic injury, vertebral artery injury, and death.
Preoperative Radiographic Evaluation
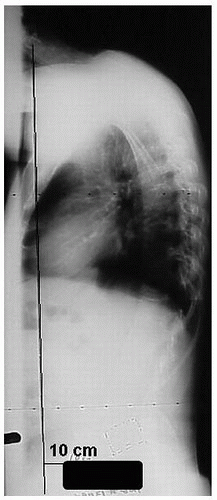
Cervical kyphotic deformities can occur at any age and may be associated with thoracic and/or lumbar deformities. It is important, therefore, to look at global sagittal and coronal balance (with full-length PA and lateral 36-inch scoliosis x-rays) in these patients to ensure that the planned correction does not cause decompensation in overall spinal balance (Fig. 5-1). You must assess cervical, thoracic, and lumbar sagittal alignment individually as well as globally and define the site of maximal deformity. The degree of correction to be obtained depends on the angle of the cervical deformity and the chin-brow to vertical angle. Meticulously plan the procedure on printed or digital x-ray including the size of the osteotomy and hardware position. Determination of osteotomy size/ angle can be done via radiographic tracing and film cutout or simple mathematical calculation (5). Planning is crucial to ensure you do not overcorrect the deformity. In addition, we recommend preoperative radiographic evaluation with computed tomography (CT), and magnetic resonance imaging (MRI). Sagittal and coronal reconstructions are helpful to better visualize the deformity. The CT scan is useful to measure the dimensions of the vertebral bodies, the cervical pedicles, and the cervical lateral masses. This information is crucial for selection of the appropriate implants and accurate planning. The MRI is useful to evaluate not only spinal cord and nerve root compression but also size and position of the vertebral arteries.
TECHNIQUE
Anesthetic Considerations
Intubation of a patient with a significant cervical deformity can be challenging. A real potential exists for spinal cord injury during intubation, as well as throughout the case due to hemodynamic changes or direct cord injury. Consequently, modern anesthetic techniques involve monitoring the cardiovascular and neurologic status of the patient. To this end, arterial line placement and motor evoked (MEP) and somatosensory evoked potentials (SSEP) are recommended to monitor blood pressure and spinal cord integrity respectively throughout the case. Subclavian central line placement for monitoring the central venous pressure can also be done if deemed necessary. We caution, with regard to neuromonitoring, that SSEPs are not always accurate and there have been cases where changes in evoked potentials have not been accompanied by changes in neurologic status (i.e., false positives). There have also been cases where a neurologic injury occurred without accompanying changes in the evoked potentials (i.e., false negatives).
One relatively safe method of intubation is awake, nasotracheal, fiberoptic intubation. Performing the intubation awake is important because the patient’s neurologic status can be continuously assessed. The abnormal fixed chin-brow vertical angle does not allow for the patient’s head to be extended, and fiberoptic intubation is necessary to visualize the vocal cords and ensure appropriate placement of the endotracheal tube. Orotracheal intubation with a chin-on-chest deformity is difficult at best due to restricted access to the oral cavity. Nasotracheal intubation is easier and can proceed after the nasal cavity has been anesthetized.
The choice of anesthetic agents is critical when evoked potentials are utilized. Paralytics and nitrous oxide are not used in these cases as they blunt the MEPs and SSEPs respectively. Total IV anesthesia is ideal in the setting of neuromonitoring.
It is important to obtain pre- and post-general anesthesia baseline readings of the evoked potentials. Since changes in the anesthetic regimen can cause changes in the evoked potentials, we do not recommend changing the drugs or dosages throughout the case.
Ensuring adequate spinal cord perfusion throughout the case is crucial. The patient’s mean arterial pressure (MAP) prior to intubation is assessed, and this MAP is maintained throughout the case (even in the face of blood loss). We do not hesitate to use transfusions and/or pressors as needed throughout the case to maintain the MAP.
Osteotomy Considerations
Numerous osteotomy techniques have been described as previously mentioned. All include some variation of opening versus closing wedge osteotomy. We will describe two cervical techniques felt to be the most efficacious and biomechanically sound depending on where the apex of the deformity occurs. The majority of deformities involving the cervical region are most severe at the cervicothoracic junction, which is also an ideal place for the osteotomy due to the reasons discussed earlier. Deformities, however, may be within the actual cervical region and necessitate osteotomy above the cervicothoracic junction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree