Cerebral Palsy
CASE PRESENTATION
A 17-year-old male with hemiplegia presents to discuss the possibility of surgery to improve his functional use of his involved right hand and the aesthetics of his arm and hand before he leaves for college next year. He is past skeletal maturity. He has done extensive therapy in the past, including splinting during growth spurts. He did not feel botulinum toxin A (Botox, Allergan Pharmaceuticals, Inc., Irvine, CA) injections helped him. On exam, he has a 20-degree elbow flexion contracture with reactive biceps spasticity, a forearm pronation contracture without evidence of active supination, a wrist palmar flexion and ulnar deviation deformity with no active wrist extension evident, and a thumb-in-palm deformity. He does have active digital extension and, with this, has evidence of dynamic swan neck deformity of his index through small fingers. His two-point discrimination is between 5 and 10 mm. He is an A/B student in a mainstream classroom.
CLINICAL QUESTIONS
What causes cerebral palsy (CP)?
How often does it occur?
How are the motor deficits in CP classified?
What are the typical patterns of muscle imbalance in the upper limb?
When is Botox indicated in the upper limb in a child with CP?
What are the surgical indications for CP patients?
What are the expected outcomes for hemiplegic upper limb surgery?
THE FUNDAMENTALS
Golf is a game that is played on a five-inch course—the distance between your ears.
—Bobby Jones
Children, and later adults, with CP never have normal motor function, and most have permanently altered sensibility. Aside from limb disorders, most have visual and cognitive abnormalities that clearly negatively impact function. Their problem is in their brain, and, as musculoskeletal and peripheral neurologic surgeons, we deal with the peripheral manifestations of their central nervous system (CNS) disorder. To completely fix their problem, someone would have to have the ability to resolve their brain disorder. That is not yet possible. However, with therapy, Botox, indicated surgery, and a multidisciplinary approach, collectively we can have a positive impact on their function and well-being. Our orthopaedic and hand surgery interventions are designed to improve their motor control and, therefore, increase their functional independence and aesthetics. A little can go a long way for these patients. We also need to counsel against unrealistic expectations or interventions that will not help improve their lives.
Etiology and Epidemiology
As defined by William Little in 1860, CP is a motor disorder due to a nonprogressive CNS lesion. The CP disorder occurs in about 1-6:1,000 live births, depending on geographic location and timing of study analysis. In the developed world, it is about 2:1,000 live births.1, 2 and 3 The disorder is more prevalent in lower socioeconomic classes. The CP disorder is the most common cause of spasticity of the limbs. Less common causes of spasticity include CNS tumors and their post-treatment sequelae, head injuries, encephalitis, embolism, and cerebrovascular accidents.
The causes of a neonatal brain injury are many. Epidemiologic and neuroimaging studies have shown it is not predominately due to birth asphyxia, as was once thought. Most neonatal brain injury is metabolic, whether from transient ischemia-reperfusion events or from defects in inherited metabolic pathways. Neonatal encephalopathy results in 15% to 20% of affected infants dying during the newborn period and an additional 25% having permanent disability.3
Causative timing for CP appears to be in utero in about 75% of cases, during delivery in about 5%, and postnatal in about 15%.4 It is most common in premature infants (40% to 50% of all CP cases are premature infants), especially those with a birth weight <1,500 g. Overall
prevalence of CP in premature infants born between 22 and 32 weeks of gestation is 8%, with 20% prevalence in the 24- to 26-week infants and 4% in the 32-week infants. An abnormal neonatal ultrasound is predictive of motor disability at 2 years, though up to 33% of CP patients had a normal neonatal ultrasound.5 Multiple gestation pregnancies and intrauterine infections are other common risk factors. Coagulation and genetic abnormalities (such as factor V Leiden mutation) may be a risk factor for vascular thrombosis and spastic hemiplegia.3,6 The relative risk of CP increases approximately four times with neonatal sepsis.7 Neuroimaging can define the CNS lesion(s) and etiologic cause in >95% of cases.
prevalence of CP in premature infants born between 22 and 32 weeks of gestation is 8%, with 20% prevalence in the 24- to 26-week infants and 4% in the 32-week infants. An abnormal neonatal ultrasound is predictive of motor disability at 2 years, though up to 33% of CP patients had a normal neonatal ultrasound.5 Multiple gestation pregnancies and intrauterine infections are other common risk factors. Coagulation and genetic abnormalities (such as factor V Leiden mutation) may be a risk factor for vascular thrombosis and spastic hemiplegia.3,6 The relative risk of CP increases approximately four times with neonatal sepsis.7 Neuroimaging can define the CNS lesion(s) and etiologic cause in >95% of cases.
Clinical Evaluation
The CP disorder is classified by (1) limb involvement (monoplegia [one limb], hemiplegia [same-sided arm and leg], diplegia [both legs], triplegia [three limbs], and quadriplegia/tetraplegia [all four limbs]) and (2) motor involvement (spasticity, flaccidity, athetosis, and other movement disorders). Most CNS lesions are in the motor cortex and corticospinal tract resulting in spasticity (70% to 80% of CP cases). An athetoid or dyskinetic movement disorder occurs in about 20% to 25% of CP cases and represents injury to the basal ganglia and extrapyramidal and/or pyramidal motor tracks. Ataxia is due to injury to the cerebellum and is seen in approximately 10% or less of patients with CP. Distinguishing spasticity from the less common athetosis is critical for management decisions, especially surgical indications. In this text, we will focus predominately on hemiplegia and less so quadriplegia, as they are the conditions that involve the pediatric hand and upper limb specialist. However, all of these patients require a multidisciplinary approach that includes pediatric orthopaedics, neurology, physiatry, nursing, social services, and physical and occupational therapy, among others. Their psychosocial, educational, and other medical issues (vision, seizures, developmental delays) are all major factors in their progress to be as functionally independent an adult as possible.
Physical exam findings vary by age.8 Most patients have already had an accurate diagnosis and workup by the time of referral to the pediatric hand and upper extremity specialist. However, inevitably there are infants and children referred with an inaccurate diagnosis (brachial plexus birth palsy) who have a CNS lesion (hemiplegia). Understanding the discriminating fundamentals of a history and diagnostic physical exam is important. In the infant, there is usually progression from initial hypotonia to a hypertonic muscle exam. There will be persistent neonatal reflexes (asymmetric tonic neck, Moro) and delay in normal motor development. Understanding the basic time frames for gross and fine motor development is essential to recognizing the child who is outside the lines (sitting on average 6 months, walking on average 13 months with outside normal range of 19 months, fine motor pinch by 15 to 18 months on average). Provocative spasticity of the pronator teres (PT) in the upper limb; adductor, hamstrings, and gastrocnemius-soleus in the lower limb; and hyperreflexia of the involved limb may be all that is indicative of subtle hemiplegia. As trite as it may sound, believe a mother’s intuition when she tells you that something is not right about her child.
Magnetic resonance imaging (MRI) is diagnostic, providing accurate anatomic information about the CNS lesion and, to some degree, the prognosis.9,10 Treatable conditions, such as hydrocephalus or vascular malformations, are identified. In a large European study of CP patients, MRI scans showed that periventricular leukomalacia was the most common cause (42.5%) of white-matter damage, followed by basal ganglia lesions (12.8%), cortical/subcortical lesions (9.4%), malformations (9.1%), focal infarcts (7.4%), and miscellaneous lesions (7.1%). Only 11.7% of these children had normal MRI findings. There were good correlations between the MRI and clinical findings.11 At this stage, almost all infants and children with CP will have at least one MRI scan as a part of evaluation and treatment planning.12,13
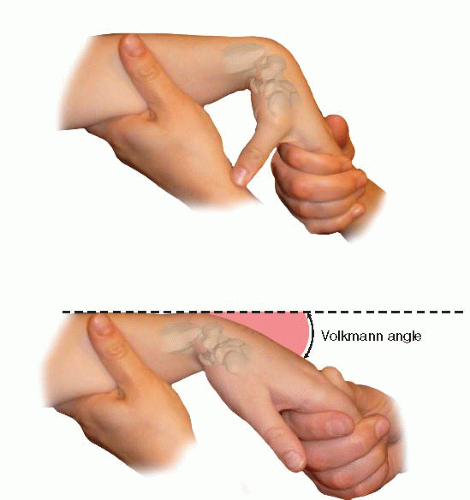
Established spastic hemiplegia has a classic exam for the upper limb: (1) adduction, internal rotation at the shoulder; (2) elbow flexion and forearm pronation; (3) wrist and finger flexion; (4) thumb-in-palm deformity; and (5) swan neck deformity fingers (Figure 22-1). Each posture represents asymmetric muscle tone, strength, and reactivity around that joint. The involved limb will be smaller in both length and girth.14 Distinguishing spasticity alone from secondary joint contracture is important. This often requires a calm setting; gentle, repeated exams; and, at times, videotaped therapy sessions with standard protocols. Passive and active motion, voluntary control, involuntary movements, and degree of joint contracture are recorded with each visit and compared with previous visits. Grasp, pinch, and release functions are assessed and classified, specifically Volkmann angle for finger flexor tightness (Figure 22-2) and Zancolli classification of finger extension. Discriminatory sensibility by two-point, stereognosis (object recognition) and graphesthesia are recorded and compared to the uninvolved side in hemiplegia. The majority of CP patients have discriminatory sensibility deficits, and this affects motor use.15
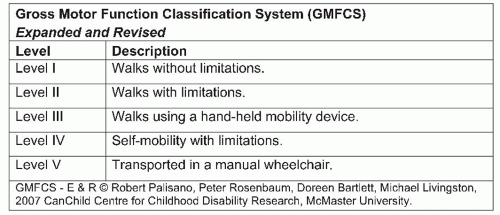
Many classification systems are used for CP patients. The Gross Motor Function Classification System (GMFCS)16 is now commonplace in most CP centers and is used to assess natural history and the effectiveness of therapeutic interventions (Figure 22-3). The Jebsen-Taylor test for hand function, the House classification (Figure 22-4),17 the Melbourne Assessment of Unilateral Upper Limb Function,18 the Assistive Hand Assessment, and the Shriner’s Hospital Upper Extremity Evaluation (SHUEE)19 are among the validated measurement tools for hand and upper limb function in children with CP.20
 FIGURE 22-1 Posture of severe spasticity with elbow flexion, forearm pronation, wrist flexion, thumb-in-palm, and mild digital flexion even in this extreme position of wrist flexion. |
These instruments provide accurate assessment of therapeutic interventions. Of note, the parents’ concept and children’s self-concept of their functional capabilities have been shown to differ greatly by objective assessment.21,22 This implies we need to gather as much information as possible from the child and to use other objective tools. Kinematic 3-D analysis and standardized videotaping of classification testing before and after intervention provide validated scoring and comparisons.23, 24, 25 and 26 In a disorder as complex as CP hand function, validated instruments are imperative. Dynamic electromyography is used to define in-phase, out-of-phase, and continuous firing activity of agonists and antagonists at specific joints and muscles in certain centers. This can be useful with highly skilled interpretation to determine the best muscles for tendon transfers.
Treatment Indications
Putting is like wisdom…partly a natural gift and partly the accumulation of experience.
—Arnold Palmer
The options for care of the hand and upper limb in CP patients include, among others: (1) natural history27, (2) occupational and physical therapy, (3) splinting, (4) serial casting, (5) electrical stimulation and biofeedback, (6) constraint therapy, (7) botulinum toxin type A (Botox, Allergan Pharmaceuticals, Inc., Irvine, CA) injections, (8) surgery, and (9) a combination of any or all of the above. The goals for each child are to prevent contractures and to maximize grasp, pinch, and release motor functions. Ultimately, interventions are designed to improve functional independence as an adult28,29 and a sense of well-being.
Almost all the children with CP have occupational and physical therapy as a part of their comprehensive care plan. Static splinting is used to prevent contractures due to muscle imbalance and hypertonicity. Most often this is at night or during leisure time so as not to impair functional activities. Daytime static or dynamic splints should truly improve function. These can include wrist extension support, thumb palmar abduction, and swan neck silver ring finger splints if warranted.30
Constraint-induced movement therapy has been shown to improve motor efficiency and quality of movement in some hemiplegic patients.31, 32 and 33 The constraint methods have included casting, sling use, and restrictive gloves. Repeated constraint therapy has been used effectively.34 However, there are limitations to the levels of evidence on this treatment method.35
Botox injections have been shown to be effective in children with no fixed contractures, good motor control, and a high motivation to rehabilitate.36, 37 and 38




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree