Cephalomedullary Nailing of the Proximal Femur
Thomas A. Russell
DEFINITION
Fractures of the proximal femur are usually grouped into four major types reflecting differences in the anatomic and physiologic character of these regions:
Femoral head fractures
Intracapsular femoral neck fractures
Pertrochanteric fractures (also referred to as intertrochanteric and peritrochanteric), which include proximal extracapsular fractures of the femoral neck region to the region along the lesser trochanter before the development of the medullary canal
Subtrochanteric fractures
Cephalomedullary nailing is the surgical stabilization of the fracture with an intramedullary device usually inserted through the piriformis fossa, the tip or lateral greater trochanter, or the medial greater trochanter.
The cephalic or femoral head portion of the fixation construct is one or more screw or blade devices interlocked with the nail component of the construct.
Cephalomedullary nails are most commonly indicated in extracapsular peritrochanteric and subtrochanteric fractures. Although there is occasional overlap of these regions, the personality of the fracture will be predominantly one of these major types.
ANATOMY
The transitional anatomy from the femoral head to the subtrochanteric region affords very different fracture pathogeneses, affecting the surgical opportunity for repair.
Intracapsular fractures of the femoral neck are critically dependent on the vascular supply from the medial femoral circumflex artery for fracture repair and maintenance of vascularity of the femoral head to avoid avascular necrosis.
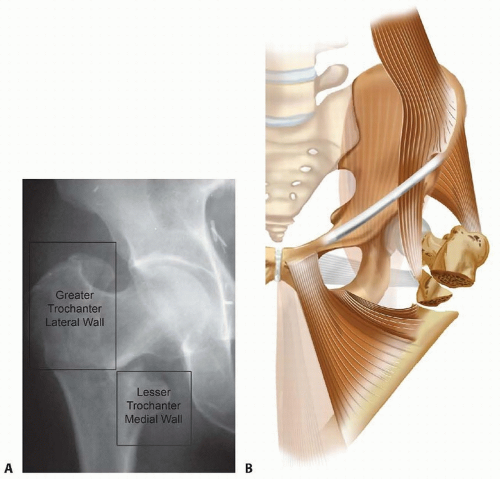
Conversely, the well-vascularized pertrochanteric region is dependent on the structural integrity of an essentially solid cancellous bone block (calcar or Adam’s arch) extending from the femoral head inferiorly along Ward triangle to the lesser trochanter, where the solid nature of the structure changes to a tubular construct with the origin of the femoral medullary canal3, 8 (FIG 1A).
Subtrochanteric fractures incur the highest stresses in the proximal femur owing to their tubular anatomy and the moment arm generated from the short proximal femoral region
and associated musculotendinous insertions, which place high degrees of stress on the implants used for their fixation.
The muscular attachments of the gluteus medius in the lateral aspect of the greater trochanter and the iliopsoas insertion in the lesser trochanter are key determinants in the deforming forces associated with fracture displacement and functional recovery after injury (FIG 1B,C).
PATHOGENESIS
Fractures of the proximal femur fall into three mechanistic categories:
Low-energy, same-level falls, predominantly in the senior population (50 to 80 years), often associated with osteoporosis and muscular atrophy
High-energy trauma in the 18- to 45-year age group from motor vehicle collisions and falls from greater heights, resulting in fractures with marked displacement and comminution
Pathologic fractures, often the first indication of a neoplastic process
NATURAL HISTORY
To obtain any real hope of ambulatory recovery, surgical treatment is necessary for complete fractures, as the resulting deformity of a nonoperatively treated hip invariably results in significant shortening and varus deformity.
Functional recovery is actually very poor despite surgical treatment of these fractures with conventional techniques in the 50- to 80-year age group.
The American Academy of Orthopaedic Surgeons estimates a 24% mortality rate in patients older than 50 years within 1 year after fracture, and only 25% of patients make a full recovery.2
PATIENT HISTORY AND PHYSICAL FINDINGS
Pertinent history for a hip fracture patient focuses on the mechanism of injury for insight into the potential quality of bone available for repair and associated injuries in high-energy trauma.
Associated injuries or premorbid diseases may coexist with the fracture diagnosis. Syncopal episodes resulting in a fall may bring attention to cardiovascular and neurologic disease states.
A history of any tumor or malignant disease, including the last mammogram and breast examination in women older than 45 years and the last prostate examination in men older than 40 years, may suggest an underlying pathologic etiology for the fracture.
Drug use, either illicit or prescribed, is a confounding and contributing factor affecting anesthesia and postoperative pain and rehabilitation management.
Unfortunately, nursing home and institutionalized patients must be examined for potential neglect and abuse.
The physical findings of a displaced hip fracture are shortening of the extremity, deformity of rotation compared to the contralateral extremity, and pain or crepitance with motion at the hip.
Shortening and rotational deformity may be the result of varus deformity at the hip from associated muscular pull or telescoping of 100% displaced fragments.
Examination should also include the Lippmann test (auscultation). Decreased tone or pitch implies fracture. Sound conduction through the pelvis and hip from the pelvis is interrupted by any discontinuity from the patella, femur, or pelvis articulations.
Swelling and discoloration with hematoma are signs of injury but are usually not acutely present.
Lacerations, Morel-Lavallée lesions, and decubitus ulcers may complicate the surgical approach.
Extracapsular proximal femur fractures extravasate blood into the surrounding tissues.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs, including an anteroposterior (AP) view of the pelvis, AP and cross-table lateral views of the affected hip, and AP and lateral radiographs, are required for diagnosis and preoperative planning.
If a long nail implant is a consideration, AP and lateral radiographs of the affected femur to the knee are required, with special attention to femoral bow and medullary canal diameter.
Computed tomography (CT) or magnetic resonance imaging (MRI) scans are rarely required for displaced fractures but may be useful in establishing the diagnosis in nonobvious fractures and atypical fractures in high-energy trauma patients.
If a pathologic etiology is suspected, however, an MRI or positron emission tomography (PET) scan of the body should be considered as part of the initial workup.
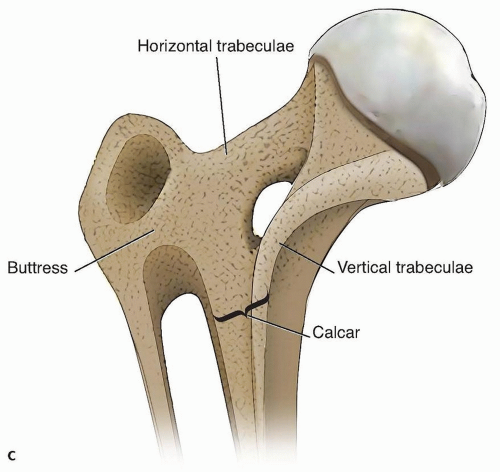
Intraoperative or preoperative traction radiography or fluoroscopic C-arm views may be helpful in delineating the extent of complex fractures.
Intraoperative length measurements with the C-arm of the normal femur may be helpful in selecting the correct nail length in complex fractures (FIG 2).
DIFFERENTIAL DIAGNOSIS
Painful arthropathy (osteoarthritis, rheumatoid arthritis, septic)
Established nonunion of the proximal femur
Pathologic deformity (ie, Paget disease, fibrous dysplasia of the hip)
Pubic rami fracture
Acetabular fracture
Contiguous femoral fracture
Hip fracture-dislocation (rare)
NONOPERATIVE MANAGEMENT
Nonoperative treatment is frequently the best option in nonambulatory or chronic dementia patients with pain controllable with analgesics and rest, patients with terminal disease with less than 6 weeks of life expected, patients with irresolvable medical comorbidities that preclude surgical treatment, and patients with active infectious diseases that preclude insertion of a surgical implant.
An exception is incomplete pertrochanteric fractures diagnosed by MRI, which have been shown to heal with nonoperative measures in selective patients.1
Nonoperative management must include attentive nursing care with frequent positioning to avoid decubiti, attention to nutrition and fluid homeostasis, and adequate analgesia or narcotic pain suppression. Patients may be mobilized from bed to chair as tolerated, usually after 7 to 14 days, with careful support and elevation of the affected extremity. Inadequate pain control is a contributing factor to dementia and increased complications.
Fracture callus at 3 weeks markedly decreases motion-related pain, and by 6 weeks, most patients can be lifted into a wheelchair or reclining chair.
Ambulatory ability may be possible after nonoperative treatment of displaced fractures.17
SURGICAL MANAGEMENT
Surgical management, once selected, should be performed as soon as any correctable metabolic, hematologic, or organ system instabilities have been rectified. Usually, this is within the first 24 to 48 hours for most patients.
The literature is inconclusive as to increased mortality after this time, but patient suffering and hospital efficiencies demand timely intervention.
Preoperative Planning
Standard AP pelvis and AP hip radiographs are usually obtained. Cross-table lateral and films in traction are useful if the hip fracture pattern is complex. Hip fractures are three-dimensional entities, and this is readily apparent in high-energy trauma cases. Full-length radiographs of good quality are required before surgery to evaluate the full extent of damage to the femur, to estimate the length and diameter of implant selections, and to avoid neglect of skip lesions or segmental damage to the femur.
Classifications for peritrochanteric and subtrochanteric hip fractures have not been particularly helpful in clinical situations, although increased surgical complexity is associated with unstable fracture patterns.9
Unstable characteristics include posteromedial large separate fragmentation, basicervical patterns, reverse obliquity patterns, and displaced greater trochanteric or lateral wall fractures.
The Evans, Kyle, AO Orthopaedic Trauma Association (AO/OTA), and Russell-Taylor classifications are commonly referred to in the literature.
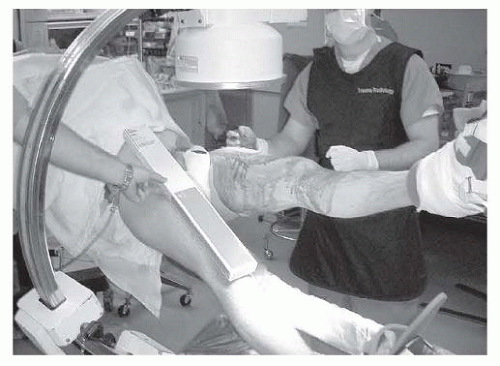
The Russell-Taylor classification assists in implant selection for the proximal femur by drawing attention to the high-risk attributes of the proximal femoral anatomy, particularly the absence or presence of fracture extension into the greater trochanter (lateral wall), referred to as group I (intact greater trochanteric region) and group II (fracture extension), and secondly the absence or presence of medial cortical stability in the lesser trochanteric region, referred to as type A (stable contact possible) and type B (fracture instability)22 (FIG 3).
Russell-Taylor type IA fractures are in reality high diaphyseal femoral fractures within 5 cm of the lesser trochanter and are preferentially treated with conventional interlocking nails, with the surgeon’s choice of either trochanteric or piriformis entry devices.
Russell-Taylor type IB fractures are fractures at the diaphyseal-metaphyseal junction of the proximal femur with medial instability due to fracture comminution of the medial calcar and lesser trochanter. The greater trochanter
and lateral wall are intact, and cephalomedullary nails, either of the reconstruction nail class or gamma nail class, are indicated, with either a trochanteric or piriformis entry type of device with the respective portal.
Russell-Taylor type IIA fractures are fractures involving the greater trochanter and lateral wall but have the possibility of restoration of medial cortical stability.
Reverse obliquity patterns fall into this group. If the greater trochanter is displaced, open reduction and stabilization are required. Trochanteric portal cephalomedullary nails are recommended if a nail technique is preferred. Piriformis nails may not obtain sufficient stability of the proximal femur. Open plate and screw reduction with an indirect reduction technique and trochanteric buttress plating may be preferred in this group of patients especially if the greater trochanter is displaced cephalad.11
Russell-Taylor type IIB fractures are the most unstable fractures, with fracture extension into the greater trochanteric region, and they have lost medial cortical stability by disruption of the lesser trochanteric region. Trochanteric cephalomedullary nails are the preferred nail option for this group if a stable nail construct can be obtained, or alternatively, a proximal femoral locking plate if comminution of the greater trochanter precludes nail stability in the proximal fragment. If the anterior femoral neck is comminuted, accessory fixation and reduction of the anterior wall in conjunction with proximal femoral locked plate fixation is advised.5
Reverse obliquity patterns and lateral wall fractures occurring in the perioperative period have been identified as high-risk patterns for sliding compression hip screwtype implants. Failure by excessive collapse of femoral neck length and medialization of the shaft is a form of dynamic failure of the implant, and although the implant may survive, the resultant deformity will compromise the patient’s functional recovery. Our ability to differentiate stable from unstable pertrochanteric fractures has been shown to be the result of unstable malreductions and unappreciated osteopenia in the shaft and femoral head fixation with implant bone interface failure as the etiology of failure.7, 16
Determination of the preoperative neck-shaft angle and medullary canal diameter is paramount to selection of the correct nail device, as different manufacturers have different neck-shaft angle and diameter nails. Another important consideration is nail curvature for long nails. Curved nails with a 1.5- to 2-m radius are applicable to most situations, but the surgeon must beware of patients with excessive curvature or tertiary curves in the distal third of the femur, as distal penetration of long nails has been reported.14
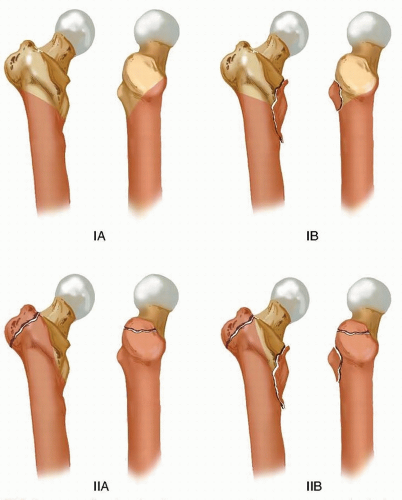
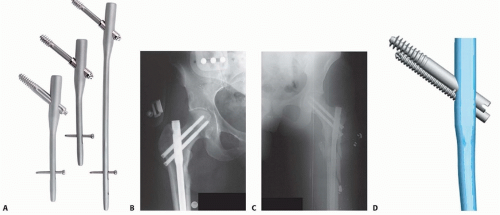
Cephalomedullary nailing involves fixation of the femoral head coupled with an intramedullary shaft implant (FIG 4). These implants are designed to have a piriformis portal for insertion, usually with the shaft component straight in the AP plane or a trochanteric portal with the shaft component laterally angulated proximally.
Modern trochanteric designs have moved to a 4- to 6-degree proximal bend positioned above the lesser trochanteric region, which seems to be most compatible with anatomic restoration of the fracture.15
Reconstruction design nails (two smaller screws into the head) (Russell-Taylor reconstruction nail and TriGen, Smith & Nephew, Memphis, TN) have the usual advantage of a smaller head diameter (average 13 to 15 mm) and may be of a piriformis or trochanteric portal design, whereas the traditional trochanteric portal (Gamma, Stryker-Howmedica, Mahwah, NJ), intramedullary hip screw (IMHS; Smith & Nephew), and trochanteric fixation nail (TFN; DePuy Synthes, Warsaw, IN) have a single large-diameter femoral head fixation screw or blade and have proximal shaft diameters around 16 to 18 mm.
New-generation cephalomedullary nails are moving to smaller geometries of 12 to 15.5 of the head to maximize bone conservation in the proximal femur and avoid excessive bone removal from the lateral wall.
New designs in femoral head fixation are also in use with constraint in the reconstruction-type two-screw design to minimize Z-effect (Targon PFN, Braun, Bethlehem, PA) and integrated interlocking two-screw fixation (InterTAN, Smith & Nephew) with the design goal of improving fracture construct rotational and translational stability.
Positioning
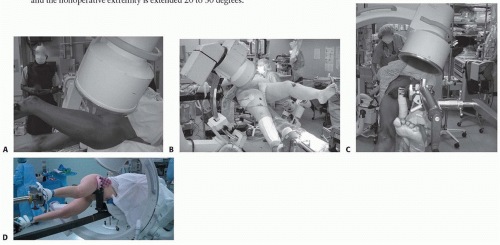
Intramedullary techniques for the proximal femur are best managed with a modern fracture table with image intensification (C-arm) capabilities.
Although the lateral decubitus approach may be helpful for reverse obliquity patterns, the supine position is usually preferred because of the ease of setup and radiographic visualization in a familiar frame of reference.
We prefer bilateral foot traction with knees in extension with the legs scissored, although attachment to the fracture table via skeletal traction through the distal femur or proximal tibia is used if there are other injuries about the knee, leg, or foot.
The operative leg is raised to about 20 to 30 degrees of flexion and the nonoperative extremity is extended 20 to 30 degrees.
The legs are pulled in line with the body to avoid varus positioning of the hip.
The C-arm is brought in from the opposite side with the base parallel to the operative extremity, centered on the midfemur such that the cephalocaudal movement of the C-arm gives good visualization of the femoral head and shaft in AP and lateral views.
With this type of setup, the true AP of the hip is usually obtained with 10 to 20 degrees of rotation of the C-arm over the top and the true lateral corresponds to about 15 to 30 degrees over the horizontal position (FIG 5A-C). The lateral decubitus position will also require adjustment of the C-arm to correct parallax error (FIG 5D).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree