10
Cartilage Healing
1. Discuss the composition and function of articular cartilage.
2. Identify common causes of injury to articular cartilage.
3. Describe the sequence of healing and the extent of intrinsic repair of articular cartilage.
4. Define invasive and noninvasive techniques of stimulating articular cartilage repair.
5. Define and describe the composition and function of fibrocartilage.
6. Identify and discuss common mechanisms of injury to fibrocartilage.
7. Describe the mechanisms of intrinsic healing of the meniscus.
ARTICULAR CARTILAGE
Composition
Articular cartilage covers the ends of bones of synovial joints. It is composed primarily of water (approximately 65% to 80%),11,13 which provides for load deformation of the cartilage surface.16 The tensile strength of articular cartilage depends on type II collagen, which is approximately 20% of the total composition of articular cartilage.19 Proteoglycans contribute 10% to 15% of the structure of articular cartilage. These proteoglycans are made up of glycosaminoglycans, which are in part responsible for bearing the compressive strength of articular cartilage. Finally, chondrocytes (mature cartilage cells) make up 5% of the articular cartilage.16,19
Articular Cartilage Zones
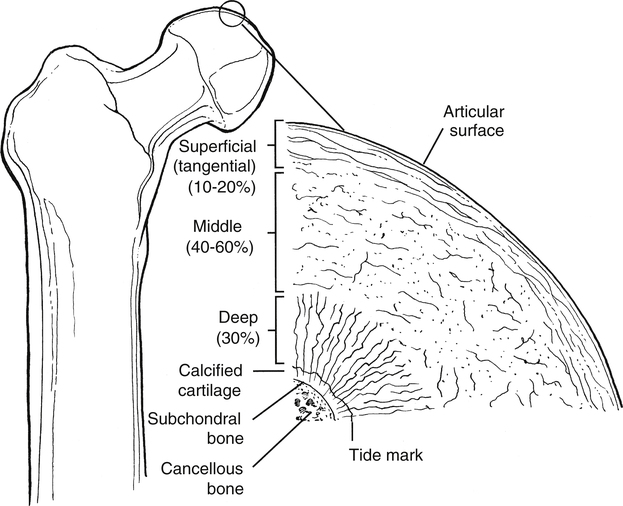
Articular cartilage is not homogeneous. The composition of articular cartilage varies considerably among four distinct zones. The superficial zone of articular cartilage is composed of water and parallel, highly organized collagen fibrils with very limited concentration of proteoglycans.14 The middle or transitional zone of articular cartilage demonstrates randomly arranged, large diameter collagen and rounded chondrocytes.14 The deep zone is rich in proteoglycans and lowest in water concentration. In this zone, collagen is large with a more organized structure that is arranged vertically.14 The zone of calcified cartilage is the deepest zone that separates cartilage tissue from subchondral bone. This small distinct layer is composed mainly of cells, cartilage, matrix, and inorganic salts (Fig. 10-1 and Table 10-1).
Table 10-1
| Layer | Width (μm) | Characteristic | Orientation | Function |
| Gliding zone (superficial) | 40 | ↓ Metabolic activity | Tangential | vs. Shear |
| Transitional zone (middle) | 500 | ↑ Metabolic activity | Oblique | vs. Compression |
| Radial zone (deep) | 1000 | ↑ Collagen size | Vertical | vs. Compression |
| Tidemark | 5 | Undulation barrier | Tangential | vs. Shear |
| Calcified zone | 300 | Hydroxyapatite crystals | Anchor |
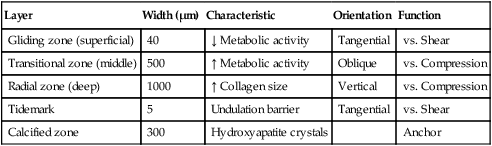
From Brinker MR, Miller MD: Fundamentals of orthopaedics, Philadelphia, 1999, Saunders.
Collagen in Articular Cartilage
Articular cartilage is an extremely unique biological tissue with both durable and permeable characteristics. Collagen represents more than 50% of the entire dry weight of articular cartilage.14 The vast majority of collagen in articular cartilage is type II; however, the extracellular matrix also contains types IV, V, VI, X, and XL.
Clinicians must recognize the composition of various collagen types to fully appreciate the remarkable resilience of articular cartilage tissue. Collagen in general contains various amounts of proline, hydroxyproline, and hydroxylysine. The proline content of collagen provides a structure that is highly resistant to tensile forces. Conversely, hydroxyproline composition of collagen provides for the compressive stability of articular cartilage. Articular cartilage is composed of collagen types that are distinct in organization, structure, and fiber arrangement that are consistent with the zones of cartilage and their unique physiologic requirements of compression, tension, stiffness, strength, and durability (Table 10-2).14
Table 10-2
| Type | Location |
| I | |
| II | |
| III | |
| IV | Basement membrane |
| V | Articular cartilage (in small amounts) |
| VI | Articular cartilage (in small amounts) |
| VII | Basement membrane |
| VIII | Basement membrane |
| IX | Articular cartilage (in small amounts) |
| X | |
| XI | Articular cartilage (in small amounts) |
| XII | Tendon |
| XIII | Endothelial cells |

From Brinker MR, Miller MD: Fundamentals of orthopaedics, Philadelphia, 1999, Saunders.
Vascular Supply of Articular Cartilage
Vascularized tissues heal in an organized, predictable fashion. Trauma to vascular tissue incites an intense cascade of events characterized by hemorrhage, inflammation, and fibrin clot formation. Angiogenesis, or neovascularization, is the hallmark of intrinsic repair through mobilization of repair molecules and undifferentiated cells capable of synthesizing matrix and new tissue.14
Conversely, articular cartilage is a nonhomogeneous and avascular structure that lacks the ability to stimulate, regulate, or organize intrinsic repair.1 Without an intense vascular response to injury, articular cartilage cannot form a fibrin scaffold or mobilize cells to repair the defect. Chondrocytes are essentially trapped within the dense extracellular matrix and are therefore incapable of traveling to the damaged site via a vascular access channel.14
Function
The viscoelastic structure of articular cartilage, by virtue of its component parts of collagen, water, and proteoglycans, makes articular cartilage incredibly durable.16,19 Generally, articular cartilage is only 2 to 4 mm thick, yet it is capable of bearing compressive loads many times greater than body weight.24 Articular cartilage is resistant to wear; has an extremely low coefficient of friction; and is responsible for influencing and dissipating compression, shear, and tension forces within synovial joints.1,16,19,24
Articular cartilage is also permeable. The chondrocytes within the cartilage must receive nutrition to remain viable. The synovial fluid surrounding the articular cartilage provides the necessary nutrients through diffusion, convection, or both.19 Diffusion and convection are achieved through joint motion and normal physiologic weight bearing. Therefore normal joint motion is needed to maintain the cartilage integrity, fluid movement (lubrication between articulating surfaces), and nutrition of hyaline cartilage.19
Immobilization and Response to Healing
Articular cartilage requires physiologic stress (e.g., cyclical compression) to maintain its unique environment as a strong, tough, fatigue-resistant, permeable, and low friction tissue.14,15 The biochemical components of proteoglycans or glycosaminoglycans (GAGs), chondrocytes, matrix-molecules, and collagen significantly contribute to its structure, composition, and mechanical properties.14,15
Just as collagen is varied and distinct among the zones of articular cartilage, so are proteoglycans distributed in different concentrations between zones. Because these proteoglycan molecules—including chondroitin sulfate, keratan sulfate, and dermatan sulfate—bind and attract water (hydrophilic), their concentration and distribution among zones influence the various mechanical wear characteristics of articular cartilage.14,15 The removal of normal physiologic loading, unloading, and joint motion have profoundly negative effects on the biochemical and mechanical characteristics of articular cartilage.14,15
The significance of articular cartilage atrophy and degeneration is related to the magnitude and duration of immobilization. Joint contact surfaces suffer greater degenerative changes than noncontact areas of articular cartilage (Table 10-3).14,15
Table 10-3
Biochemical Changes of Articular Cartilage
| Biochemical Structure | Aging | Osteoarthritis (OA) |
| Water content (hydration; permeability) | ↓ | ↑ |
| Collagen | Content remains relatively unchanged | |
| Proteoglycan content (concentration) | ↓ (Also the length of the protein core and GAG chains decreases) | ↓ |
| Proteoglycan synthesis | ↓ | ↑ |
| Proteoglycan degradation | ↓ | ↑ |
| Chondroitin sulfate concentration (includes both chondroitin 4- and 6-sulfate) | ↓ | ↑ |
| Chondroitin 4-sulfate concentration | ↓ | ↑ |
| Keratin sulfate concentration | ↑ | ↓ |
| Chondrocyte size |