Chapter 33 Cardiac Rehabilitation
Historical Development
Herrick first described a myocardial infarction (MI) in 1912. Bed rest for 2 months was prescribed because activity was believed to induce congestive heart failure (CHF), ventricular aneurysm, cardiac rupture, and sudden death. By 1930, pathologic studies revealed stable scar formation by 6 weeks.133 Bed rest was recommended for 6 weeks, strenuous activity limited for longer, and return to an active lifestyle or work was infrequent. By the 1950s, early ambulation programs at 4 weeks157 and then at 14 days35 after MI were implemented. These reduced the complications of prolonged bed rest, including deconditioning, venous thrombosis, and pulmonary embolism. During the 1970s and 1980s, hospital lengths of stay shortened because of economic pressures and studies on determinants of return to social functioning.240 Similar outcomes and safety with early ambulation were noted, with no significant difference in occurrence of angina, reinfarction, CHF, or death.1
Formalization of post-MI activities into what is now considered phase 1 inpatient CR was initially described by Wenger et al.236 Patients progressed from bed rest to independence in activities of daily living (ADL), household ambulation, and stair climbing within 2 weeks. Patients were then discharged home.
Advances in technology and medical management have significantly reduced hospital lengths of stay for MI. Changes in managed care and Medicare policy, the prospective payment system for inpatient rehabilitation, and the “75% rule” for admission to inpatient rehabilitation units have also influenced hospital lengths of stay and inpatient CR. According to Medicare claims in the United States, CR use is relatively low among beneficiaries despite convincing evidence of its benefits.200 To assess the benefits of CR in an older diverse population, analysis of more than 600,000 U.S. Medicare beneficiaries who were hospitalized for HD or a revascularization procedure was conducted. Mortality rates at 1 and 5 years were compared in CR users and nonusers. Depending on the analysis method, CR reduced 5-year mortality by 21% to 34%. Moreover, a survival benefit was apparent in all demographic and clinical subgroups of patients, including those with MI, those who underwent revascularization, and those with heart failure. On final analysis, subjects who completed 25 or more sessions of CR were 19% less likely to die over 5 years than matched users who completed fewer sessions (p < 0.001). Just 12.2% of subjects used CR, and the average number of sessions was 24.201 Patients are now discharged within 3 to 5 days after an uncomplicated MI, and 5 to 7 days after cardiac surgery. Reductions in hospital lengths of stay greatly affect the early phases of CR.
Epidemiology of Cardiovascular Disease
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in men and women in the United States. In 2006 an estimated 81.1 million American adults (more than 1 in 3) had 1 or more types of CVD. Of these, 38.1 million were estimated to be 60 years or older.126 Prevalence increases with advancing age: 51% of men and 48% of women between the ages of 55 and 64 years have CVD, and 71% of men and 79% of women older than 75 years are affected.43 In the United States there is one coronary event every 26 seconds, and one death every minute from HD. There are more than 600,000 new MIs each year, and more than 300,000 recurrent MIs. In 2006 a total of 935,000 new and recurrent MIs occurred.126 Within 1 year of an MI, 25% of men and 38% of women will die, and 50% will die within 8 years. An average of 11.5 years of life is lost secondary to an MI.
From 1996 to 2006, the total number of inpatient cardiovascular operations and procedures in the United States increased 33%, from 5,444,000 to 7,235,000 annually. Hospital-based interventions for the management of HD show that in the United States the number of cardiac catheterizations decreased slightly from 1996 to 2006, from 1,161,000 to 1,115,000 annually. In 2006 an estimated 1,313,000 percutaneous coronary interventions (previously referred to as percutaneous transluminal angioplasty) were performed in the United States. Also in 2006, 253,000 patients underwent a total of 448,000 coronary artery bypass procedures (defined by procedure codes). Coronary artery bypass graft (CABG) volumes have declined nationally over the past decade. A total of 2163 heart transplantations (HTs) were performed in 2008, virtually the same number that were performed annually for almost two decades. In 2006, 114,000 implantable cardioverter defibrillators and 418,000 pacemakers were placed.126
Economic costs are also rising in the United States, with costs in 2010 for all HD estimated to be $316.4 billion. Half is for hospital, physician, and medication costs, and half is due to the lost productivity resulting from morbidity and mortality. The estimated total direct and indirect cost of CVD and stroke in the United States for 2010 is $503.2 billion.126
By modifying risk factors for HD, mortality rates have fallen from 228 per 100,000 population in 1970, to 178 per 100,000 in 2001, to 142 per 100,000 in 2006. Life expectancy in the United States is currently 77.7 years (2006 population data).126 If all CVD was eliminated, the estimated life expectancy would increase by 7 years8 (based on turn-of-the-century mortality and population data). The impact of CVD is not limited to the United States. Globally the World Health Organization estimates nearly 20 million people die annually of CVD, contributing to nearly a third of all deaths.
Risk Factors for Coronary Artery Disease
Risk factors for coronary artery disease (CAD) are summarized in Box 33-1.
Physical Inactivity
Physical inactivity accounts for 250,000 deaths annually. More than 60% of adults in the United States do not participate in regular physical activity. Single women, the elderly, the less educated, the less affluent, African Americans, and Hispanics are more likely to be inactive.216 The American College of Sports Medicine recommends at least 30 minutes of moderate-intensity physical activity on most days of the week, approximating to 600 to 1200 calories expended per week through exercise. Total energy expenditure, rather than duration or type of activity, has the greatest influence on the development of CAD. Higher levels of energy expenditure predict significantly lower CAD risk.121
Physical activity improves other modifiable risk factors for CAD (Box 33-2). Physical activity also reduces the incidence of CAD25,120 and associated morbidity.216 A study of more than 40,000 men in the United States shows that a healthy lifestyle might prevent a majority of coronary heart disease events.45 The protective effect is maintained only with lifelong exercise.163 Physical activity and exercise in adults without HD is extremely safe, with the risk for a cardiac event ranging between 1 in 400,000 and 1 in 800,000 hours of exercise. The risk for an event is significantly lower among regular exercisers.64 In a study of more than 6200 men, exercise capacity was found to be a more powerful predictor of mortality than other established risk factors for CVD.152 A cohort of more than 5700 women followed up over 8 years determined that the same applies to women.86
Hypertension
Normal blood pressure and hypertension are classified in Table 33-1.
Table 33-1 Classification of Hypertension
| Systolic Blood Pressure (mm Hg) | Diastolic Blood Pressure (mm Hg) | |
|---|---|---|
| Normal | <120 | <80 |
| Prehypertension | 120-139 | 80-89 |
| Stage 1 hypertension | 140-159 | 90-99 |
| Stage 2 hypertension | >160 | >100 |
Approximately one billion people worldwide have hypertension, and 7.1 million die annually of its complications. Hypertension is the most significant risk factor for death worldwide.251 It affects mostly elderly people,38 and the incidence increases with age.225 Nearly 25% of adults in the United States have hypertension that requires treatment.90 Despite intensive education campaigns, however, 30% of people with hypertension do not know they have it. Hypertension is suboptimally controlled with medication in 25% of patients, and 11% are not medicated. Only one third of patients with hypertension have their blood pressure controlled with medication,44 and many elderly patients are not treated to an optimal level.24 Recent public health programs have improved awareness of and treatment rates for hypertension.
Risk for MI and death increase as blood pressure rises above 115/75 mm Hg.125 The presence of other CAD risk factors compounds the risk from hypertension.7 It is significant that a blood pressure reduction of 5 mm Hg produces a 9% reduction in mortality from CAD.238
Management of hypertension requires lifestyle modifications, including increased physical activity and dietary changes238 for weight management, as well as restriction of sodium and alcohol intake. Among other benefits, high-intensity interval walking might be protective against age-associated increases in blood pressure.156
In an extensive review of the evidence for prescribing exercise as therapy in chronic disease, strong evidence was found for the positive effects of training on the pathogenesis, symptoms specific to the diagnosis, physical fitness and strength, and quality of life (QOL) in hypertension.166 Lifestyle modification without medication is recommended in stage 1 hypertension for 12 months in those with no other risk factors, or 6 months in people with other risk factors. It can lower systolic blood pressure (SBP) between 3.7 and 4.3 mm Hg.10 Medications are recommended for stage 2 hypertension, or when lifestyle modifications do not normalize blood pressure.
Smoking
Cigarette smoking is the leading preventable cause of illness and premature death in the United States. More than a third of all smoking-related deaths are caused by CVD,42 and up to 30% of all CAD deaths in the United States annually are attributable to smoking.215 Patients who continue to smoke after CABG have increased morbidity and mortality compared with those who stop smoking.102 Financial costs are also significant, with more than $157 billion annually in medical care and lost productivity.42
Prevention of smoking and smoking cessation are essential. With education, fewer youths are starting to smoke, and since 1965 smoking rates have dropped 40% in American adults. Of the 45% of patients who stop smoking spontaneously after a coronary event, 70% relapse within 1 year.176 A nicotine withdrawal syndrome is responsible for the significant difficulty most people have in quitting smoking.6 The benefits of smoking cessation are significant. The risk for developing CAD is reduced by 50% within 1 year, and there is a substantial decrease in CAD mortality.79,184,192 Mortality rates by 3 to 5 years after MI are reduced by 50%,248 and sudden cardiac deaths are also reduced.76 A combination of behavioral support, nicotine replacement, and bupropion provides the highest success rates for smoking cessation, approaching 20%.173
Dyslipidemia
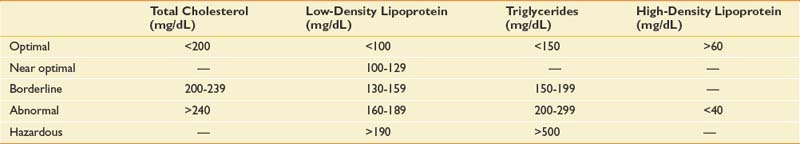
Dyslipidemia is defined in Table 33-2.153
About 105 million adults in the United States have total cholesterol levels of 200 mg/dL or higher, and 50% have a low-density lipoprotein (LDL) level of 130 mg/dL or higher. Up to 40% of white men have a high-density lipoprotein (HDL) level below 40 mg/dL. A raised LDL level over 100 mg/dL is an independent risk factor for CAD245 and predicts risk for recurrent events in preexisting CAD.250 Reducing the LDL level is associated with fewer CAD events.33 Elevated triglyceride levels are also correlated with CAD.14 A low HDL level is an independent risk factor for CAD, reversed by raising HDL.245 Although genetics is the main factor, 50% of HDL levels are accounted for by overweight, inactivity, smoking, and diabetes.
Achievement of optimal lipid levels is initially done by lifestyle modification, including dietary changes, increased physical activity, and weight loss. Aerobic exercise, including the use of a bicycle ergometer,50 and strength training can lower LDL and triglyceride levels, raise the HDL level, and reduce the risk for CAD. This benefit is maintained as long as exercise is ongoing.212 The effects of therapeutic exercise on the pathogenesis of dyslipidemia, as well as on specific symptoms of the condition, physical fitness, and strength are supported by strong evidence.166
Reduction of LDL levels through dietary changes reduces CAD incidence. Plant stanols and sterols, and soluble fibers including oats, barley, and psyllium can lower LDL levels.78 Dietary guidelines for lipid management are summarized in Table 33-3. Medications, including statins,188 are also effective in reducing total cholesterol, LDL, and triglyceride levels, and increasing HDL levels, as well as reducing the risk for developing CAD and recurrent events.184
Table 33-3 Dietary Guidelines for Lipid Management
| Calorie Source | Total Daily Calories (%) |
|---|---|
| Total fat | 30 |
| Polyunsaturated fat | 10 |
| Monounsaturated fat | 20 |
| Saturated fat | <7 |
| Carbohydrates | 50 |
| Proteins | 15 |
| Cholesterol | <200 mg/day |
| Fiber | 20-30 g/day |
Overweight and Obesity
More than 60% of American adults are overweight, defined as a body mass index greater than 25 kg/m2. Approximately 30% of all white and African American men, and 50% of African American women are obese (body mass index >30 kg/m2). Increasing numbers of children are overweight. Currently 22% of African American children are overweight.196 Childhood obesity is linked to a greater risk for adult mortality from CVD.
Overweight is associated with 300,000 deaths annually from all causes.4 Obesity is also related to increased morbidity and poorer QOL.65,67 Overweight contributes to hypertension, dyslipidemia, diabetes, and the metabolic syndrome. A 10-lb weight gain increases the risk for CVD and mortality.134 Conversely, a weight loss of 10% reduces risk factors for CAD.154 Direct economic costs of obesity-related CAD, diabetes, and hypertension approach $43 billion. Indirect costs total $31 billion, approximately 9.4% of the U.S. health care expenditure.48 Strong evidence for the positive effect of training has been established on pathogenesis, diagnosis-specific symptoms, physical fitness and strength, and QOL in obesity.166
Diabetes
A fasting blood glucose level greater than 125 mg/dL defines diabetes. A normal fasting blood glucose level is less than 110 mg/dL, and a level between 110 and 125 mg/dL is considered an impaired fasting glucose level.60 About 17 million people in the United States and 5% of all adults have diabetes, and 14.5 million have impaired fasting glucose levels. There are 800,000 new cases of type 2 diabetes diagnosed annually. One third of all people with diabetes are undiagnosed and untreated.95 African Americans and Hispanic Americans have twice the incidence of diabetes as that of white persons.193 The prevalence of diabetes in the United States is currently 7%, and increasing in parallel with increasing rates of obesity and physical inactivity.94
Impaired fasting glucose229 and diabetes increase the incidence of and mortality from CAD.39 In 65% of patients with diabetes, mortality is due to CAD.73 CAD can go undetected because myocardial ischemia is often silent in people with diabetes as a result of autonomic dysfunction.247 Adequate diabetic control in patients with CAD reduces the incidence of MI, decreases the need for cardiac interventions and surgery, improves QOL, and extends survival.190 Dietary modification for weight loss and increased physical activity are first-line therapy for hyperglycemia. Strong evidence supports the prescription of therapeutic exercise in type 2 diabetes, improving outcome on pathogenesis, symptoms specific to the diagnosis, physical fitness and strength, as well as QOL.166 The addition of oral medications or injectable insulin might be needed to optimize control.
The metabolic syndrome (see following discussion) is a combination of insulin resistance with dyslipidemia, hypertension, and a prothrombotic state.81 This syndrome can precede the development of overt diabetes.
Metabolic Syndrome
Key components of the metabolic syndrome are noted in Box 33-3. Three or more of components 1 through 5 must be present for diagnosis.153 Approximately 47 million people in the United States have metabolic syndrome. Prevalence increases with age. It is noted in nearly 45% of people older than 60 years and in one third of overweight or obese people.66 Metabolic syndrome is an independent risk factor for CAD89 and predisposes to diabetes and increased mortality.116 Treatment focuses on management of underlying risk factors including overweight, physical inactivity, and poor diet. Medications for dyslipidemia, hypertension, hyperglycemia, and thrombosis are considered to optimize control. There is strong evidence that in the metabolic syndrome, the pathogenesis of insulin resistance, specific symptoms, physical fitness, strength, and QOL are all affected by exercise.166
Emerging Risk Factors
Other emerging factors associated with CAD risk are summarized in Table 33-4.
Table 33-4 Emerging Risk Factors for the Development of Coronary Artery Disease
| Risk Factor | Treatment |
|---|---|
| Lipoprotein (a)52 | Nicotinic acid9 |
| Homocysteine239 | Folic acid, vitamins B6 and B12132 |
| Prothrombotic states144 | Aspirin101 |
| High-sensitivity C-reactive protein114 | Statins147,160,175 |
Nonmodifiable Risk Factors
The risk for CAD increases with age, and men have higher rates of CAD at any age than those of women. Women lag about 10 to 15 years behind men in the incidence of CAD.245 A previous personal history of CAD, peripheral vascular disease (PVD), and CVD increases the chance of a future cardiac event. Family history also correlates with risk for CAD, although the influence of genetic predisposition is not easily separated from environmental factors and learned behaviors.187 Men and postmenopausal women are more likely to develop CAD, as are many minorities, partly because of higher rates of hypertension, obesity, and diabetes in these populations.
Exercise Physiology
Energy Substrates
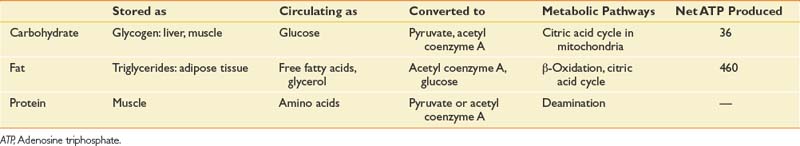
Energy substrates are the fuels used in metabolic pathways (Table 33-5).
Carbonic acid is rapidly converted to water (H2O) and carbon dioxide (CO2):
Oxygen Consumption
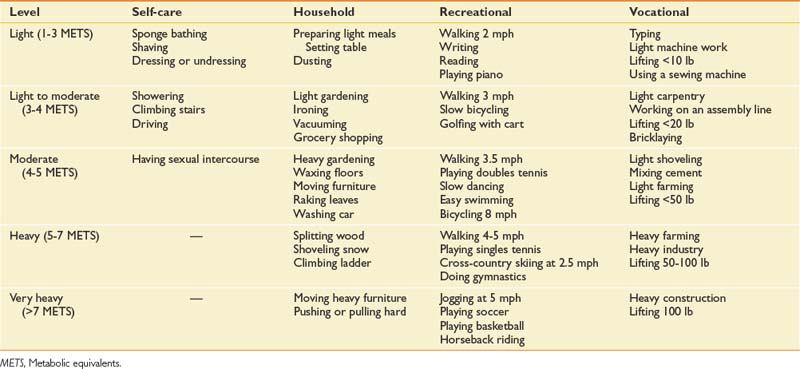
O2 is measured using a metabolic cart, and is the volume of oxygen consumed at any level of activity. Under controlled conditions, at rest, an average 70-kg man consumes 3.5 mL of oxygen per minute for every kilogram of body weight. The unit of oxygen consumption at resting, or “basal metabolic rate,” is referred to as one metabolic equivalent (1 MET). Any increment in activity will produce greater oxygen consumption, or METs. Many tables exist of the MET level equivalent for varying intensities of exercise and different activities, such as in Table 33-6.
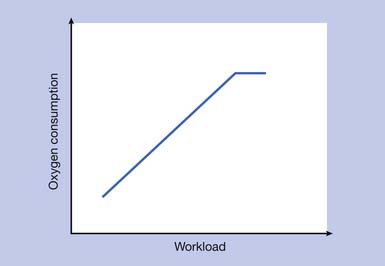
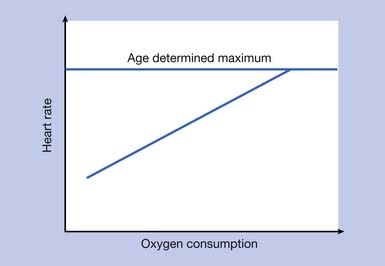
For any given level of aerobic training, as exercise intensity increases past a critical point, the ability of physiologic systems to provide oxygen is outstripped by the body’s oxygen requirements. This represents anaerobic threshold, and using metabolic gas analysis, no further increase in O2 is seen (Figure 33-1). A rate of maximal O2 has been reached (O2max, or aerobic capacity). If further exercise is done after this point, anaerobic mechanisms produce the energy required. Because of lactic acid accumulation, only a short duration of further exercise is possible.
The Fick Equation
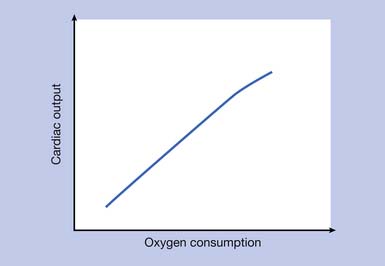
Cardiac output at any degree of aerobic training is a product of the heart rate (HR) and stroke volume (SV; the volume of blood expelled by the left ventricle during one contraction). The major determinant of SV is the diastolic filling volume. However, diastolic filling volume decreases as HR increases. With slow HR at low exercise intensities, cardiac output initially increases because of increased SV, but at higher intensity levels it increases because of increased HR.63
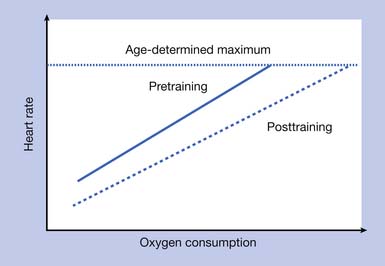
The relationship of exercise intensity to cardiac output is essentially linear (Figure 33-2). HR also increases in a linear relationship to exercise intensity (Figure 33-3).
The arteriovenous oxygen difference reflects the ability of the muscle to extract oxygen from the blood for use with muscle metabolism and energy production. Determinants include the pulmonary, hematopoietic, vascular, and muscular systems (Box 33-4).
Aerobic Training
Training is “muscle group–specific,” and changes in the cardiopulmonary response to exercise will be noted only when the trained muscle groups are tested. For example, a treadmill training program will not significantly improve the cardiovascular response to bicycling. When designing aerobic training programs, a combination of different aerobic machines using multiple muscle groups is recommended. Significant functional, musculoskeletal, cardiovascular, and psychologic adaptations are noted in 6 to 10 weeks after training is started, depending on the intensity and frequency (see Box 33-4). Biochemical changes are noted within 10 days of starting training. Lack of activity or bed rest can significantly reverse these beneficial effects over the course of 2 to 3 weeks.
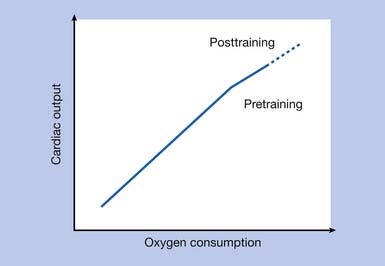
Aerobic training influences all determinants of the Fick equation. After a standard aerobic training program, a small but significant increase is noted in cardiac output at higher work intensities. At rest and submaximal work intensities, however, cardiac output remains the same as that before training (Figure 33-4).
HR at rest and submaximal work intensities are actually reduced compared with the untrained state, because of enhanced vagal tone producing cardiac slowing. So it is the increased SV noted at rest and at submaximal and maximal work intensities after training that is responsible for the increased cardiac output. The reduced HR allows for a longer diastolic filling time (Figure 33-5). The arteriovenous O2 difference is also increased after training (Box 33-5).
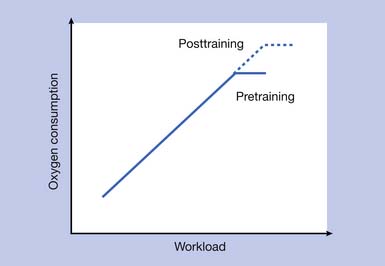
The increased peripheral oxygen utilization by aerobically trained muscles accounts for the majority of the increase in O2max seen after aerobic training programs. At rest and during submaximal levels of exercise intensity, however, there is no difference in O2 before and after the aerobic training program (Figure 33-6).
Myocardial Oxygen Consumption
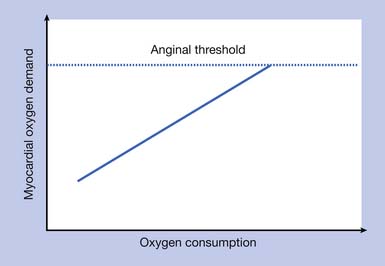
Myocardial oxygen consumption (MO2) increases in a linear fashion with increasing exercise intensity. In a normal heart the supply of blood and oxygen matches the MO2. The major determinant of myocardial blood flow is the diameter of the coronary arteries, which normally dilate to increase capacity as myocardial oxygen demand increases. In coronary arteries affected by atherosclerosis, a point is reached where the supply can no longer be increased, and further demand produces a relative lack of myocardial oxygen, or ischemia or angina. The exercise intensity when this point is reached is considered the ischemic or anginal threshold (Figure 33-7).
Measurements of myocardial blood flow and MO2 are only possible with invasive techniques and are not clinically applicable. An estimation of MO2 can be made from the product of HR and SBP, or the double product (DP):
Exercise training does not affect the ischemic threshold. Only catheter-based coronary interventions or CABG will alter the anatomy of the coronary arteries and enhance blood flow. Combined intensive programs of lifestyle changes, very-low-fat vegetarian diets, aerobic exercise, stress management, smoking cessation, and group psychologic support have also produced significant regression of coronary atherosclerosis compared with control subjects, with a significant decline in cardiac events.162
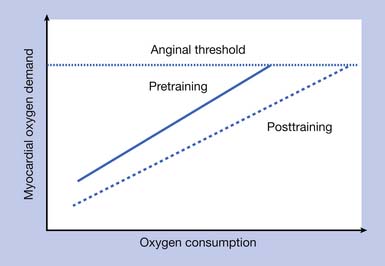
MO2 after an aerobic training program is lower at rest and submaximal levels of exercise intensity. This is clinically relevant for patients with CAD, who will be able to perform activities at a greater intensity after an aerobic training program before reaching ischemic threshold as compared with before training. For the same intensity of activity performed after training, a lower MO2 is achieved, providing a wider margin of safety for those with CAD (Figure 33-8).
Cardiac Evaluation
History
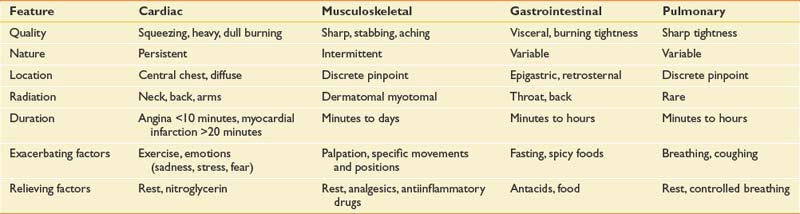
Cardiac causes of chest pain must be differentiated from noncardiac causes (Table 33-7). Besides chest pain, cardinal symptoms likely to materialize in CR, such as palpitations, dyspnea, edema, cough, and dizziness, are important to evaluate. For their significance, relevant textbooks in cardiology are recommended. It is also important to note that deconditioning, depression, medications including β-blockers, and poor sleep are common noncardiac causes of fatigue. Patient education that cardiac fatigue worsens with further rest and improves with physical exertion is important for compliance with exercise recommendations.
Physical Examination
Pulse rhythm and rate are important. A normal sinus rhythm is a regular pulse between 60 and 100 beats/min with a P wave preceding every QRS complex on the ECG. Bradycardia is a rate less than 60 beats/min. It can be physiologic in athletes because of increased vagal tone to the heart, and can be pharmacologic as a result of medications including β-blockers. It can also be pathologic, as in sick sinus syndrome, heart block, and junctional or ventricular escape rhythms. Tachycardia, a rate above 100 beats/min, is normal only after exertion. Other causes include pain, dehydration, anemia, CHF, hypotension, and hyperthyroidism.Fear and anxiety can also play a role during CR in a patient who is unfamiliar with the rehabilitation process. Medication (β-blocker and calcium channel blocker) noncompliance can produce rebound tachycardia.
Peripheral pulses should be examined. Carotid bruits and diminished or absent lower extremity pulses indicate widespread vasculopathy. Skin integrity of the feet can be impaired, producing ulceration and gangrene (see Chapter 56). Lower limb amputation requires special consideration when planning CR.
Cognitive examination is helpful, because atherosclerosis underlies CAD, CVD, and some dementias. Post-MI or post-CABG confusion can be caused by preexisting dementia or indicate a new cerebral event. Anesthesia, hypoxia, and medications can result in significant temporary orpermanent cognitive deficits, with safety and dependency issues. “Pump head” is a slang term for an acute confusional state after cardiopulmonary bypass used for cardiac surgeries. Some patients who go through surgery “off pump” also experience confusional states. A fluctuating cognitive state after a cardiac event or surgery is consistent with a toxic encephalopathy. This usually resolves over days to weeks. Magnetic resonance imaging (MRI) of the brain can also reveal a “shower” of cerebral emboli, originating from an aortic atheroma or the left ventricle during surgery. Recovery is usually complete. Monitoring for safe use of exercise equipment is necessary during CR in cognitively impaired patients.
Cardiac Testing
Cardiac electroshock therapy (EST) is generally safe, and adverse outcomes are infrequent.197 Absolute and relative contraindications to EST are summarized in Box 33-6.75