Callus Distraction Principles and Indications
Dennis E. Martin
The technique of callus distraction has been employed since the early 1900s, but it has only been recently that the methodology has evolved and surgeons have taken advantage of this alternative surgical approach to bone grafting (1). There are a number of potential indications for callus distraction, and these include the correction of a number of congenital, hereditary, traumatic, and septic sources of foot and extremity deformity. In this chapter the principles, science, and indications for callus distraction are discussed.
HISTORY
The origins of callus distraction can be traced back to the early 1900s. Although Codivilla (1) is most commonly cited as the first surgeon to address a shortened limb by distraction and traction concepts, the contributions of several other pioneers from this era cannot be overlooked (2,3). Codvilla performed an oblique osteotomy of the femur that was then lengthened by placing a sudden and intense pull on a steel rod inserted through the calcaneus. The correction was then maintained by a plaster cast that incorporated the steel bars until healing occurred. If greater lengths were needed, the process was repeated at later intervals.
Steinmann (2) modified this technique by placing his newly developed Steinmann pin through the distal tibia as opposed to the calcaneus. Correction was secured by applying traction with weights to the extremity. Freiberg (2) placed a steel rod through the posterior process of the os calcis and connected it to a traction screw via a heavy picture wire. A spring-loaded scale was used and served as a dynamometer. Forces as high as 45 kg were often needed to achieve the desired length. Any subsequent lengthening that was needed was performed without anesthesia. All of these procedures were quite traumatic and poorly tolerated by the patients.
In 1913, Magnunson (3) attempted to improve this technique by making it simpler and less risky for patients. He executed a Z-osteotomy of the femur and separated the two fragments by traction and countertraction with weights. Once the desired length was obtained, a plug was placed between the bone ends and the weights were removed. The bony fragments were fixed with absorbable ivory screws. Despite what appeared to be an excellent attempt at improving patient morbidity, all patients were greatly traumatized, and one patient died. The frustration and disappointment resulting from these complications resulted in surgeons abandoning the techniques of callus distraction for a short period of time.
Interest in bone lengthening via traction increased again in the late 1920s and early 1930s. In 1927, Abbott (4) described a procedure that, with some modification, became a popular operation in the United States. He was the first to use the tibia as his target tissue for lengthening. Following osteotomy of the fibula and insertion of Steinmann pins in the proximal and distal ends of the tibia, the tibial osteotomy was performed and the distraction apparatus applied. He cautioned against correcting over 5.08 cm of deformity. Abbott also performed a lengthening to the Achilles tendon as part of his correction. Carrell (5) was concerned about forward angulation of the fragments secondary to the bowstring action of the tightened leg muscles. He attempted to offset these forces by placing a third pin in front of the fragments. Unfortunately, this led to significant skin damage in adjacent areas and proved to be unsuccessful. Brockway and Fowler (6) used an off-center pin on the proximal end of the osteotomy to try to address the potential angulation problem. Two pins were inserted on each side of the osteotomy and the more distal of the two proximal pins was placed slightly more anterior. Some surgeons preferred Kirschner wires (K-wires) to Steinmann pins (7,8).
Haboush and Finkelstein (8) were the first to emphasize the importance of maintaining the periosteum at the level of the osteotomy. The sleeve of periosteum that was preserved resulted in a quicker deposition of callus and more rapid healing. Bosworth (9) also advocated the Abbott technique and suggested a delay of 10 days between execution of the
osteotomy and the initiation of lengthening. He was also one of the earliest surgeons to report positive results with few complications.
osteotomy and the initiation of lengthening. He was also one of the earliest surgeons to report positive results with few complications.
In 1934, Putti (10) described a femoral osteotomy that was gradually lengthened over an 18- to 21-day period. He designed an apparatus that allowed for traction and countertraction forces to be applied during the lengthening period. With this technique, he typically achieved between 6.35 and 10.16 cm of length.
Despite these efforts to improve the success of the procedure and to reduce patient morbidity, complications persisted and leg lengthening through traction techniques became unpopular again in the late 1930s. Compere (11) stated that all surgeons performing leg lengthening procedures had encountered some degree of complication. He divided complications into three broad categories: (a) overstretching, (b) interference of blood supply to the fragments, and (c) insufficient fixation of the fragments.
Following World War II, there was a renewed interest in leg-lengthening procedures. The emphasis during this era was placed on trying to develop better means of fixation. Attempts were made to not only improve the strength of fixation but to make the devices less traumatic. Allan (12) created an apparatus that allowed the K-wires used for fixation to be placed in stirrups and clamped in a carrier. One of the pairs of wires was fixed while the other was capable of moving in a direction away from the stationary counterparts. Allan also advocated leaving the periosteum intact while performing an oblique osteotomy. He recognized the importance of preserving as much soft tissue as possible around the lengthening site. Once the desired length was obtained, he secured the position with screws. Allan’s modification was also short lived owing to a variety of complications that arose.
Other authors tried to improve on the type of fixation used to stabilize the osseous fragments. McCarroll (13) used a slotted plate with traction, whereas Bost and Larsen (14) proposed use of an intramedullary rod to hold the alignment as traction was applied.
In an effort to improve success rates and reduce patient morbidity, alternative techniques were investigated. Several surgeons (15,16) attempted epiphyseal growth plate stapling with modest results. However, there was still a need for a more effective, yet less complicated procedure owing to the limited amount of correction that could be obtained through epiphyseal stapling. This led Anderson (17), in 1952, to return to bone lengthening through traction. He performed the correction in two stages. The first stage consisted of a fibular osteotomy and a slotting technique of the distal fibula under an osteoperiosteal flap of the adjacent tibia. Once it was confirmed that there was no continuity to the fibula (approximately 6 weeks later), the tibial lengthening was started. Several surgeons modified this technique further in an effort to accomplish the correction in one stage. Coleman and Noonan (18), Gross (19), and Mitchell (20) all provided immediate fixation of the fibula to the tibia, along with executing the tibial osteotomy and assembling the distraction frame.
Agerholm (21) modified the osteotomy design by making it zigzag in effort to increase stability to the osseous fragments. Kawamura (22) made an important addition to Anderson’s technique by performing the osteotomy through the cortex only in an attempt to preserve the nutrient vessels and endosteal tissue. These developments during Anderson’s era mark the beginning of positive progress that continued over the next 30 years.
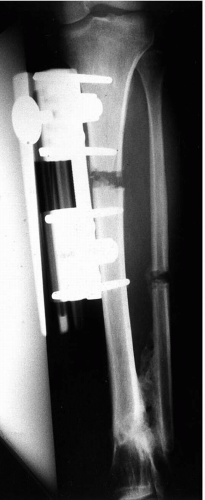
Modern day advancements in the science of callus distraction for bone lengthening actually began with the work of Wagner (23) in the early 1970s. Although his suggestions of sectioning the periosteum at the level of the osteotomy and his choice of a mid-diaphyseal location are points of controversy, Wagner made many positive contributions. He recognized the importance of slow gradual lengthening versus sudden extreme corrections. His device allowed for 1.5 mm of lengthening per complete revolution, which was executed with one full turn daily. Wagner also noted the importance of maintaining function to the limb and advocated partial weight bearing with the frame in place to allow joint motion to be preserved. This was a definite improvement over the Anderson device, the latter of which required the patient to be confined to bed. Furthermore, Wagner’s device was smaller and lighter, with a simpler method of elongation. He employed a unilateral frame with 6-mm Schanz pins. This device is very similar to the modern day external fixators (Fig. 1).
The final era in the development of callus distraction is that dominated by the concepts of Ilizarov. Ilizarov (24) began working on and publishing his ideas on bone transport as early as the 1950s in Russia. However, owing to the political climate of that time and difficulties in translation, it was not until many years later that individuals in other countries noted his work. He felt strongly about preserving the contents of the intramedullary canal during osteotomy to improve osteogenesis and decrease consolidation time. However, the actual significance of this aspect of the technique remains a controversial issue. He also expanded the understanding regarding the timing of initiating the lengthening and the rate of subsequent distraction. A delay of 5 to 7 days following osteotomy was recommended to allow for better consolidation (25). He also showed that a lengthening of 1.5 mm per day, as proposed by Wagner, is dangerous and can lead to ischemic changes. Ilizarov believed that slower, more frequent lengthening would allow for better osteogenesis and elongation of soft tissues.
These ideas are very important and have shaped our understanding of today’s science of callus distraction. Ilizarov was also a proponent of early mobilization and weight bearing, and actually prescribed participation in calisthenics for his patients while they were still in their frames.
Although these contributions changed the course of bone lengthening as a science, it was actually Ilizarov’s fixator that led to his notoriety. He popularized the concept of a ring fixator with multiple transfixation pins to stabilize the osseous fragments. By fixing each of the segments at more than one level, he was able to increase bending stiffness, but because of the flexibility afforded by the smaller size wires (1 to 2 mm), axial loading resulted in some motion. This axial movement has been thought to be very beneficial for osteogenesis in the lengthening gap. Hence, here lies the wisdom in early weight bearing following execution of the osteotomy. This continues to be one of the most popular methods used to distract and lengthen bone. This device is discussed and demonstrated in detail in Chapter 4.
PHYSIOLOGY AND HISTOLOGY
Fracture Repair
The histologic events that take place in callus distraction are quite similar to those seen in normal fracture repair. The natural sequence of repair is interrupted at the “soft callus” stage, and a distraction sequence is started. Therefore, a basic knowledge of the histophysiologic features behind fracture repair is helpful in understanding the overall process.
The intrinsic process of bone healing has been broadly referred to as callus formation. Generally speaking, there are two types of callus formation: (a) periosteal or extrinsic callus and (b) endosteal callus. External or periosteal callus is the type that is most familiar to clinicians. It represents the expanding cuff of healing bone that is often seen on a radiograph in a fracture that is undergoing repair (Fig. 2). Its formation is related to the periosteal activity and the mechanical stability or instability of the fracture. Although it is less appreciated on radiographs, endosteal callus formation also plays an important role in bone healing. This type of fracture repair is most commonly seen in metaphyseal or short bones.
The basic process of repair begins with hemorrhage at the fracture site created by tearing of osseous and periosteal vessels. Hematoma then forms and fills the gap between the fracture fragments. As the hematoma begins to organize, it is invaded by a variety of cells with different functions. Macrophages dominate the early phase of healing as they enter to remove the necrotic blood and tissue debris. Within several days, fibroblasts from the surrounding periosteal and mesenchymal tissues invade the organized clot and begin to lay deposits of collagen and fibrocartilage. This allows for stiffening of the clot and aids in decreasing motion between the bone ends. As a result of several factors, including low oxygen tension at the clot site, fibrocartilage is the basic ground substance produced at this early callus production stage. Resorption of necrotic bone occurs as the haversian system begins the process of removal of nonviable osseous tissue.
Vascularization of the maturing hematoma or procallus begins to occur simultaneously. This vascular infiltrate comes from three separate areas. Capillaries infiltrate from the external periosteal vessels and internally from the endosteal
tissue. The haversian system of the surrounding cortical bone also supplies vascular elements. This latter source of vascularity accompanies the haversian structure and consists of a leading edge of osteoclastic cells with a trailing deposition of osteoblasts. As the oxygen tension of this procallus increases, the product of the osteoprogenitor cells becomes that of osteoid. The calcium hydroxyapatite that comprises the deposited osteoid allows more rigidity and stiffening between the fragments. It is at this stage that the repair becomes radiographically visible. The mechanical stability of the fracture will determine how much callus is formed. The callus will then mature and create clinical union between the fragments. This callus will eventually be replaced with the normal architecture of the primary osseous structure.
tissue. The haversian system of the surrounding cortical bone also supplies vascular elements. This latter source of vascularity accompanies the haversian structure and consists of a leading edge of osteoclastic cells with a trailing deposition of osteoblasts. As the oxygen tension of this procallus increases, the product of the osteoprogenitor cells becomes that of osteoid. The calcium hydroxyapatite that comprises the deposited osteoid allows more rigidity and stiffening between the fragments. It is at this stage that the repair becomes radiographically visible. The mechanical stability of the fracture will determine how much callus is formed. The callus will then mature and create clinical union between the fragments. This callus will eventually be replaced with the normal architecture of the primary osseous structure.
In the science of callus distraction, controlled mechanical instability is induced at the stage of soft callus production just before or simultaneous with mineralization. Fracture stability is then reestablished when the desired correction is obtained.
Callus Distraction
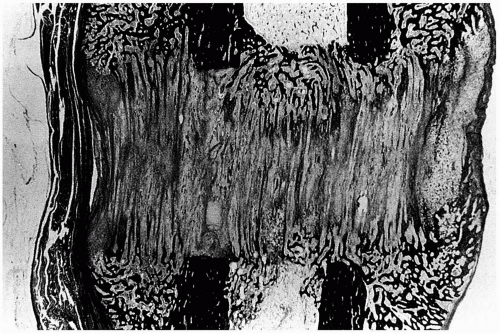
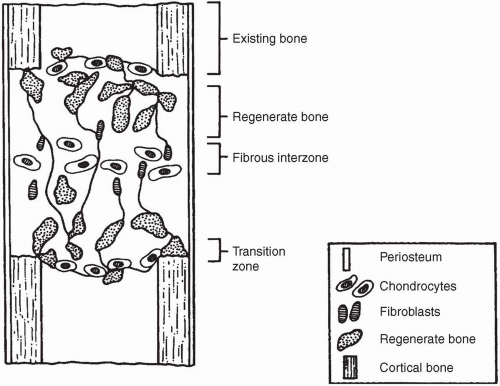
When distraction of an osteotomy is initiated, a gap is created and filled with hematoma and fibrous exudate. Within days, the gap is invaded by immature connective tissue. Vascular channels then appear, and at approximately 3 weeks, callus begins to form as fine cancellous bone is laid down in columns (Fig. 3). The callus is initially represented by longitudinally oriented collagen fibers, around which bone spicules eventually form. Some of these fibers span the entire distance between bone ends (Fig. 4). At either end of the gap, fibrocartilage is seen between the bone end and the ossified or sclerotic edge of the distraction zone. The central growth zone appears in the center of the gap and is primarily composed of fibroblasts and chondrocytes (Fig. 5).
Regenerating bone continuously matures during and after lengthening. The radiolucent growth zone becomes ablated approximately 4 weeks after distraction has been stopped (Fig. 6). Cortex formation, called corticalization, takes place around 4 to 6 months after surgery and continues to remodel over a period of a year or more. Radiographically, the difference between regenerate bone and fracture callus is the organized longitudinal striations seen in callus distraction. Fracture callus is typically more bulbous in shape and lacks longitudinal striations.
 FIG. 4. Radiograph 6 weeks postoperatively, demonstrating the axial callus formation spanning the distance of the osteotomy site. |
There are also differences seen histologically between regenerate and normal bone, at least in the early stages of repair. Walsh et al. (26) determined that the tensile properties of the lengthened bone improved and increased with time following the cessation of distraction. However, they remained significantly weaker (50%) than the controls, even at 12 weeks. Hamdy et al. (27) added that even when 80% to 90% of the cortices regained their continuity, the strength of the lengthened bone was only 50% to 60% that of normal controls. Hence, the importance of initiating a slow gradual return to normal activity. Sferra et al. (28) found that on torsional testing of the lengthened tibia, five out of six bones fractured within the diaphysis but outside the regenerate area. These findings suggested that the strength of the lengthened segment exceeded that of the original diaphysis, which was exposed to stress shielding by the external fixator.
Periosteum
In the early years of bone lengthening, the exact role of the periosteum during the reparative process was unclear. It is now well accepted that preservation of the periosteum is critical to timely and efficient callus production. Most authors agree with this concept, and convincing evidence has been derived in the laboratory (29). In this study, the role of the periosteum and endosteum were evaluated. A group of 27 rabbits was divided into one of three groups: (a) The periosteum was sutured following osteotomy and the bone ends were repositioned; (b) the periosteum was removed from the segments around the osteotomy and no attempt at repairing it was made; (c) the endosteum was scraped out from the bone ends on each side of the osteotomy, and the periosteum was sutured. The most successful group consisted of those who had the endosteum maintained and the periosteum repaired. When the periosteum was removed, callus formation was greatly disturbed and there was failure of bone healing. In contrast, scraping of the endosteum had little effect on the healing process. Clinically, this would allow the surgeon to execute the osteotomy, recognizing that violating the endosteum would not result in a delayed healing so long as the periosteum is repaired.
Soft Tissue Lengthening
The vast majority of attention surrounding the science of callus distraction is dedicated to the cellular and physiologic changes occurring in the bone and the distraction zone. Although this knowledge is important to understanding the science of the procedure, the effects of the peripheral soft tissues cannot be overlooked. In order for this technique to be successful, the muscles, ligaments, and neurovascular structures must be able to accommodate the amount and rate of lengthening. There is considerable research being performed on these particular structures. Several studies have already shown that muscle and nerve will respond to a slow gradual distraction process (30,31). The smaller and more frequent distracting sequence, suggested earlier for bone, also appears to be optimal for soft tissues. However, excessive amounts of sudden lengthening (2 mm) can lead to permanent damage to the muscles and other soft tissues (30). This may result in muscle weakness and imbalance, as well as neurovascular damage and prolonged edematous changes. Although more work needs to be done in this particular area, a good rule of thumb is to use the same distraction parameters for soft tissues that are suggested for bone.
Understanding the physiology behind callus distraction can be summarized by reviewing Ilizarov’s law of tension-stress (32). The law states that living tissue, when it is subject to slow steady distraction, can become metabolically activated in both the biosynthetic and proliferative pathways. This theory has been tested and confirmed more recently by several other surgeons (33, 34, 35, 36, 37, 38).
PARAMETERS OF DISTRACTION
Once the concepts of callus distraction were understood at the histologic level, the next stage was to choose a set of distraction parameters that would provide for the quickest and most efficient means of bone consolidation. Important parameters to consider included osteotomy versus corticotomy, level of osteotomy, latency period, amount and rate of distraction, and the ossification period.
Osteotomy versus Corticotomy
There is still some debate over whether there is any benefit to performing a corticotomy as opposed to a complete osteotomy. A corticotomy refers to a technique in which sequential drill holes are placed circumferentially around the bone and are eventually connected by an osteotome or scalpel. The potential benefits include preservation of the endosteum with perhaps a more timely consolidation period. However, the benefit of preserving the endosteum has been found to be of little clinical significance (29). In addition, performing a corticotomy alone is at times technically difficult owing to the juxtaposition of other anatomic structures that may prevent full access to the bone. Obviously, preservation of the endosteum might be optimal if it is anatomically feasible and if this can be accomplished with minimal disruption to the surrounding soft tissues.
Level of Osteotomy
One of the most important decisions relative to callus distraction is the determination of the proper level in which to perform the osteotomy. Potential sites may include the proximal metaphysis, diaphysis, distal metaphysis, and the growth plate, if it is still present. Considerations when making this decision include the level of deformity, the amount of length and angulation needed for correction, the size and the extent of the vasculature in the area, the amount of soft tissue coverage in the vicinity, and the technical ease with which the osteotomy can be performed, and the available access for accurate insertion of the fixation pins.
Diaphyseal Osteotomies
Much of the early literature identifies the diaphysis as the location of choice for placement of the osteotomy (4, 5, 6,9). Although metaphyseal lengthening is becoming increasingly popular, diaphyseal osteotomy is still recommended and performed by many surgeons (39, 40, 41). This area typically allows for easier access, and surgery is often less demanding. The osteotomy site is usually well defined, and accurate pin placement is easier. Diaphyseal locations also offer easier manipulation of the periosteum. A periosteal sleeve can be created and resutured following osteotomy. This is more difficult to accomplish in metaphyseal bone.
However, there are differing opinions regarding diaphyseal osteotomies. The bone is this area is relatively less active metabolically when compared with the rich cancellous bone found in the metaphysis. This cancellous network combined with the increased soft tissues around the metaphysis should allow for faster, more homogeneous osteogenesis. Additionally, the mechanical strength of a structure varies with the
square of its diameter when subjected to bending loads. This means that at any given stage of lengthening, if the diameter of the metaphysis is twice that of the diaphysis, then the strength is greater by a factor of four (41). Therefore, a wider segment of bone will tend to be more stable throughout the lengthening process, and should lead to a stronger end result (Fig. 7).
square of its diameter when subjected to bending loads. This means that at any given stage of lengthening, if the diameter of the metaphysis is twice that of the diaphysis, then the strength is greater by a factor of four (41). Therefore, a wider segment of bone will tend to be more stable throughout the lengthening process, and should lead to a stronger end result (Fig. 7).
Metaphyseal Osteotomies
Despite the fact that callus distraction has worked well when the osteotomy is performed in the diaphysis, most surgeons prefer to perform the osteotomy in the proximal metaphysis (36, 37, 38,41, 42, 43, 44, 45). As suggested previously, performing the osteotomy in the metaphyseal area of bone may have certain advantages, one of which is a greater surface area for distraction. The increase in stability and strength afforded by the larger diameter of bone at the level of distraction helps balance some of the osteopenic changes that result from disuse during the lengthening period. This becomes important when weight bearing is initiated or when the concept of dynamization is desired. Dynamization is a concept based on the assumption that longitudinal compression stimulates bone formation in long bones. In practical terms, this means that the surgeon allows some degree of well-controlled weight bearing to be applied to the bone before final consolidation. This can be provided by deliberately loosening of the frame, or it can be a characteristic of the frame itself, such as in the Ilizarov device.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree