Calcaneal Fractures
Meagan M. Jennings
John M. Schuberth
Calcaneal fractures account for about 2% of fractures and 60% of major tarsal injuries (1). Falls from a height account for 75% of these injuries, usually averaging a height of 14 feet but have been reported from as little as 3 feet (2,3). The age of incidence is usually between 30 and 50 years with a 5:1 male to female ratio (4,5,6,7,8,9,10 and 11). Up to 70% of the patients sustaining a calcaneal fracture have another associated injury with 10% to 20% having concurrent spinal compression fractures particularly of the thoracolumbar segment (T12-L2) (2,3,5,12). Other extremity injuries account for about 26% (2,13), 7% occur bilaterally, and 98% are closed injuries (11). Seventy-five percent are intra-articular in adults, whereas only 25% are intra-articular in children (4,14). Motor vehicle accidents, avulsion-type injuries from an Achilles tendon contraction, and stress fractures in athletes are other etiologies for calcaneal fractures (9,15,16).
The calcaneus is the largest bone in the foot and serves as the posterior limb of the longitudinal arch. It serves to transmit high-tensile, binding, and compressive forces (17). Inherently, the calcaneus with both traction and compression trabeculae is separated by a “neutral triangle.” It is thought to represent a vascular conduit (18) with the base of the triangle often being vulnerable during axial impaction of the talus into the calcaneus, resulting in a vertical fracture through it, which is often referred to as the “primary fracture line,” first coined by Essex-Lopresti (14). For more detail on the distinct anatomy of the calcaneus, one should refer to a foot and ankle atlas.
MECHANISMS OF INJURY
Typically, the biomechanical forces that act on the calcaneus when it fractures are not within a single dimension. Shearing forces from twisting or rotary type movements often can account for fracture of the sustentaculum, the anterior superior process, or the medial tuberosity. Avulsion-type injuries include the posterior superior process and anterior superior process. These injury patterns are often the result of tensile forces that are exerted via various ligaments and tendons at their points of attachment.
INITIAL EVALUATION
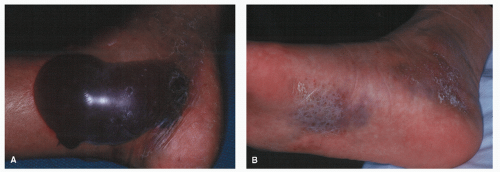
The initial evaluation of patients with calcaneal fractures must include the axial and appendicular skeleton to rule out other associated injuries and appropriate radiographs should be ordered. Simultaneously, the skin and soft tissues should be examined for open lacerations, blisters, and swelling (Fig. 107.1A). Ecchymosis into the plantar arch is often present and termed “Mondor sign.” (Fig. 107.1B).
Both hemorrhagic and nonhemorrhagic blisters can occur, indicating the extent of the soft tissue envelope with hemorrhagic typically indicating a deeper soft tissue injury. These should thus be avoided when planning surgical approaches. Nonhemorrhagic blisters indicate a more superficial injury and viable epidermal cells often remain. Inspection for areas of pressure necrosis is also essential. Indicators of potential problematic areas are designated by blanching or tenting of the skin by underlying displaced bone fragments. Often, the posterior heel deserves thorough inspection due to the potential of necrosis with displacement of the calcaneal tuberosity in tongue-type or tuberosity avulsion fractures. Signs of necrosis warrant early reduction and fixation to relieve pressure on the skin due to the potential disastrous consequences of skin loss, especially overlying the posterior calcaneus.
DIAGNOSTIC IMAGING
Obtaining complete understanding of the fracture is probably the most crucial piece in the treatment scheme of calcaneal fractures. If the treating physician does not thoroughly understand the fracture pattern, appropriate care cannot be delivered. Radiographs and computed tomography (CT) scans are the two key diagnostic imaging technologies.
Standard radiographs should typically include a minimum of three views, which would include a dorsal-plantar (DP) foot, lateral foot/ankle, and a Harris axial view of the hindfoot. An internal oblique ankle view can often nicely demonstrate the congruency of the posterior facet of the calcaneus as well. Radiographs of the spine should not be overlooked in the patient with any complaints of accompanying back symptoms because a high incidence of associated fractures has been reported (2,3,12).
RADIOGRAPHIC VIEWS
Dorsal-Plantar View
The DP view is the most effective view to examine for extension in to the calcaneocuboid joint, which has been reported to occur in approximately 25% of calcaneal fractures (19). One can also determine medial talar displacement, lateral wall blowout, and other foot fractures.
Lateral View
The lateral view is probably the most telltale view for a calcaneal fracture and provides information regarding the ankle joint, the talus, and the anterior and posterior superior processes. It is instrumental in evaluating key angles including the Böhler angle (tuberosity joint angle) and the crucial angle of Gissane (20). These two angles are useful in revealing a depressed posterior facet or fracture of the calcaneal body such as the superior tuberosity fracture. When comparing coronal CT scans with lateral radiographs, authors found underestimation of the
amount of depression and rotation of the posterior facet on coronal CT and concluded sagittal CT or lateral radiographs to better estimate fracture displacement (21).
amount of depression and rotation of the posterior facet on coronal CT and concluded sagittal CT or lateral radiographs to better estimate fracture displacement (21).
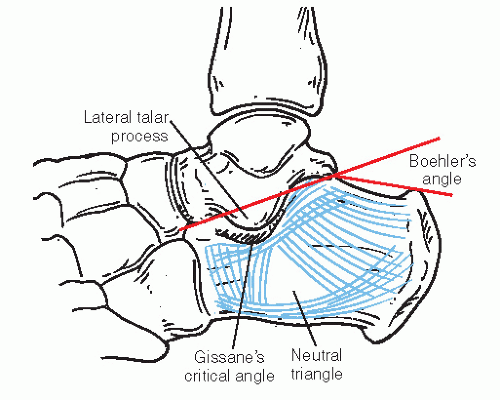
Tuberosity Joint Angle (Böhler Angle)
Böhler (7) described this angle in 1931 as the angle, which is formed by the intersection of the line from the highest point of the anterior process of the calcaneus to the peak of the posterior articular surface and a line from the highest point of the posterior articular surface to the highest point or “peak” of the tuberosity (Fig. 107.2). A wide variance of measurements for this angle has been described ranging from 10 to 40 degrees (22), although Böhler described it between 30 and 35 degrees. A contralateral film can always be ordered for comparison.
Böhler theorized that the dorsal displacement of the calcaneal tuberosity was induced by contraction of the gastrocnemius-soleus complex. Although the Böhler angle can significantly decrease or even reverse with a severe calcaneal fracture, it does not necessarily correlate to intra-articular extension and distortion (22,23,24 and 25), which has been demonstrated by other authors.
Critical Angle of Gissane
Gissane (20) first described this critical or crucial angle in 1947. This angle reveals the angular relationship of the calcaneal facets and parallels the lateral process of the talus on a lateral radiograph (see Fig. 107.2). The cortical density represents the subchondral bone beneath the posterior, anterior, and middle facets. The angular measurements vary from 130 to 145 degrees (22). The disruption of this angle typically can be attributed to the lateral process of the talus being driven through the posterior facet in a wedge-like manner during axial load. Thus, it correlates to intra-articular distortion.
Harris Calcaneal Axial View
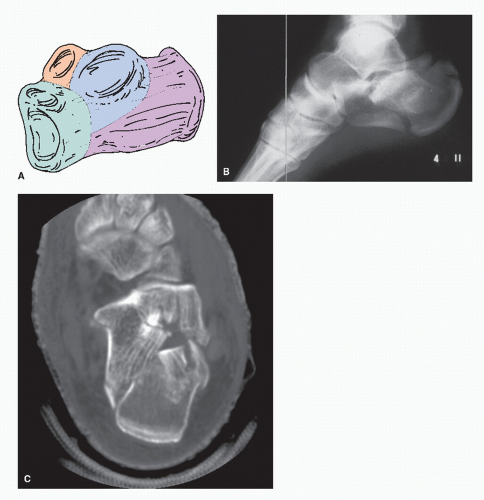
While sometimes difficult to obtain with patient injury, the Harris axial view can serve as a valuable view to assess the posterior facet as well as medial and lateral walls of the calcaneus (Fig. 107.3). This view may also allow visualization of the primary fracture line and splitting of the calcaneus into two major fragments—the superomedial or sustentacular fragment and the lateral tuberosity fragment. This view is obtained with the beam approaching from posterior to anterior distal, 30 degrees to the film, which is placed flat on the platform. Dropping the central beam 5 to 25 degrees with respect to the horizontal should also allow visualization of the middle facet.
Brodén Views
In developing this projection technique, Brodén attempted to demonstrate the anteroposterior profile of the posterior facet (27). The Brodén views are probably most helpful intraoperatively when CT imaging is not available to allow the surgeon radiographic visualization of the subtalar joint (STJ) for fracture reduction purposes. This radiographic projection has the patient’s foot and leg internally rotated 45 degrees with the ankle at neutral dorsiflexion. The central beam is directed 2 to 3 cm anterodistal to the lateral malleolus, and four projections are taken at 10-degree intervals off of the perpendicular (Fig. 107.4). This view can often capture the middle facet.
Computed Axial Tomography
The application and advancement of CT imaging has allowed significant progress in the
approach and treatment of calcaneal fractures. CT allows both two-dimensional as well as three-dimensional reconstruction images, thus helping with the evaluation of a fracture pattern and determining definitive treatment. Typically, small incremental cuts of approximately 1.5 mm as perpendicular to the posterior facet as possible are recommended. This orientation allows visualization of the posterior facet in what is closest to the coronal plane. Due to the usefulness of CT imaging, classification schemes developed based solely on the use of CT exist and are standardized to help surgeons in fracture assessment and reduction (28,29 and 30).
approach and treatment of calcaneal fractures. CT allows both two-dimensional as well as three-dimensional reconstruction images, thus helping with the evaluation of a fracture pattern and determining definitive treatment. Typically, small incremental cuts of approximately 1.5 mm as perpendicular to the posterior facet as possible are recommended. This orientation allows visualization of the posterior facet in what is closest to the coronal plane. Due to the usefulness of CT imaging, classification schemes developed based solely on the use of CT exist and are standardized to help surgeons in fracture assessment and reduction (28,29 and 30).
Intraoperative CT scan is a technology that is being developed and improved upon. One study has shown that the information obtained from the scan led the surgeon to alter the reduction or screw placement during the procedure in 41% of the patients with high accuracy and quality as well as clinical benefit (31).
CLASSIFICATIONS
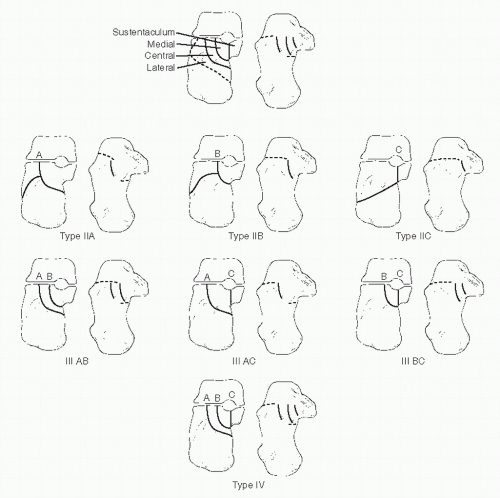
As with any fracture, there are a number of different classification schemes for calcaneal fractures, which are used to communicate to others the description of a fracture pattern, the possible underlying etiology, as well as prognosis. The most important and helpful ones tend to consider the underlying etiology and reliability as a prognostic indicator. Authors reviewing calcaneal fracture classification schemes found that the most prevalent systems utilized were the Essex-Lopresti (14), Zwipp’s Hannover (29) scheme (Fig. 107.5), and Sanders et al (28) (Fig. 107.6). Although each classification system had a positive correlation with outcomes, none have shown a direct correlation with treatment (32).
Extra-articular fractures comprise 25% to 30% and intraarticular fractures account for 70% to 75% of all adult calcaneal fractures. The Pre-CT classifications, understandably limited, offer the primitive distinction between outcomes of intra-articular versus extra-articular fractures, which was originally made by Essex-Lopresti (14). In fact, Essex-Lopresti’s (14) descriptions of intra-articular fractures are still used by most today in lieu of Rowe types IV and V, whereas Rowe succinctly describes extra-articular calcaneal fractures.
Essex-Lopresti (14) described two primary intra-articular fracture patterns: the “tongue type” (type A) and the “joint depression” (type B). He postulated that both fractures share a common primary fracture line that extends vertically from the angle of Gissane to the plantar surface of the calcaneus. The secondary fracture line, being what separates the two patterns, extends posterior from the vertex of Gissane angle directly posterior to the posterior tuber of the calcaneus, including one large posterior fragment that is usually divided into medial and lateral parts. With a joint depression fracture, the secondary fracture extends from the same vertex; however, it continues posterior and dorsal to encircle the lateral portion of the fractured articular surface of the posterior facet. This is often referred to as the “thalamus” or “thalamic portion” as first coined by Soeur and Remy (35). Regardless, the tongue-type and joint depression fractures are essentially both joint depression fractures.
The Sanders CT classification scheme is based on the concept established by Soeur and Remy but utilizes CT to determine the location and fracture lines through the posterior facet and the resulting number of articular fragments produced by the injury. Of the CT classification schemes, it tends to exhibit a higher prognostic value (30) and typically is useful for classification of intra-articular calcaneal fractures (32).
Zwipp’s Hanover classification scheme for calcaneal fractures demonstrates that fracture lines could be divided into a relatively constant primary fracture, running from the posterior STJ surface to the tuber calcanei, and highly
variable secondary fractures. The calcaneus is divided into four segments: the sustentacular segment, the posterior STJ segment, the segment of the anterior process, and the tuberosity segment. In addition, the posterior STJ, the anterior STJ, and the calcaneocuboid joint are used in the classification scheme. Classification is by the number of segments (x) and the number of joints (y) affected and accordingly is labeled as x-segment, y-joint fracture. The addition of both numbers is used to grade the severity of the fracture (29) (see Fig. 107.5).
variable secondary fractures. The calcaneus is divided into four segments: the sustentacular segment, the posterior STJ segment, the segment of the anterior process, and the tuberosity segment. In addition, the posterior STJ, the anterior STJ, and the calcaneocuboid joint are used in the classification scheme. Classification is by the number of segments (x) and the number of joints (y) affected and accordingly is labeled as x-segment, y-joint fracture. The addition of both numbers is used to grade the severity of the fracture (29) (see Fig. 107.5).
EXTRA-ARTICULAR FRACTURES
Extra-articular fractures of the calcaneus most commonly involve the posterior tuberosity of both tubercle fractures and tuberosity body fractures, sustentaculum tali, anterior process, and the posterior beak that may or may not be of the avulsiontype fracture pattern.
PLANTAR TUBERCLE FRACTURES
Plantar tubercle fractures are thought to most commonly result from a fall with the heel in valgus, which subjects the medial process to a shearing force that produces the fracture. It is uncommon for this type of fracture to displace due to the extensive soft tissue attachments and septal connection of the plantar heel pad. If it is displaced, closed reduction should be attempted followed by casting. Nondisplaced or minimally displaced fractures are treated with below-knee immobilization for typically 4 to 6 weeks. Early weight-bearing can often be initiated after the subsidence of pain and edema. After healing has commenced, any persistent discomfort can be addressed with a viscoelastic heel insert.
SUSTENTACULUM TALI FRACTURES
These fractures are fairly uncommon and are considered to represent the initial stage of a joint depression fracture. At a
single institution, Della Rocca et al (36) cited an incidence of 20 sustentacular type fractures without posterior facet involvement in a series that included over 300 operative calcaneal fractures. Of these 20 cases, 15 underwent open reduction and internal fixation (ORIF) utilizing a medial approach as previously described by Burdeaux Jr (37). An inverted foot position at the time of impact can allow the talus to impact medially onto the cortical ledge, thus shearing the sustentaculum off of the main body. Clinically, edema and ecchymosis directly below the medial malleolus will present and occasionally, passive dorsiflexion of the hallux can produce pain beneath the sustentaculum. Subtalar inversion produces acute discomfort medially in contrast to deltoid injury, which tends to be more symptomatic with eversion. Radiographically, obtaining a calcaneal axial view is essential. Displacement of this fragment should warrant ORIF (Fig. 107.7).
single institution, Della Rocca et al (36) cited an incidence of 20 sustentacular type fractures without posterior facet involvement in a series that included over 300 operative calcaneal fractures. Of these 20 cases, 15 underwent open reduction and internal fixation (ORIF) utilizing a medial approach as previously described by Burdeaux Jr (37). An inverted foot position at the time of impact can allow the talus to impact medially onto the cortical ledge, thus shearing the sustentaculum off of the main body. Clinically, edema and ecchymosis directly below the medial malleolus will present and occasionally, passive dorsiflexion of the hallux can produce pain beneath the sustentaculum. Subtalar inversion produces acute discomfort medially in contrast to deltoid injury, which tends to be more symptomatic with eversion. Radiographically, obtaining a calcaneal axial view is essential. Displacement of this fragment should warrant ORIF (Fig. 107.7).
ANTERIOR PROCESS FRACTURES
The anterior process fracture is commonly caused by either avulsion secondary to the bifurcate ligament, extensor digitorum muscle belly, and/or calcaneocuboid ligament. It has been reported that these types of fractures account for 15% of calcaneal fractures (38). More commonly seen in females, this is thought to be due to the wearing of high-heeled shoes (39,40 and 41) and has been referred to as a “sprain fracture” (42). The mechanism is that of an adduction/plantarflexion force that places tension on the bifurcate ligament and results in an avulsed portion of bone.
The compression fracture type of the anterior process fracture is typically due to one of two mechanisms: (I) dorsiflexion-eversion type of mechanism or (II) a forced abduction of the forefoot with the hindfoot fixed causing impaction of the lateral column (43,44). This same mechanism can be associated with avulsion of the navicular tuberosity. Dagan et al classified these injuries as follows: type I is a nondisplaced fracture usually involving the tip of the anterior process, type II is a displaced fracture not involving the articular surface, and type III is a large displaced fragment involving the calcaneocuboid joint and have the poorest prognosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree