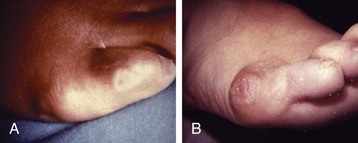
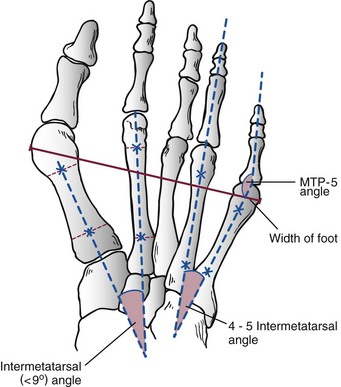
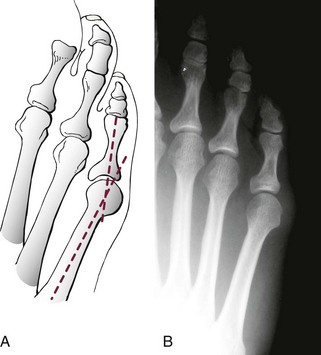
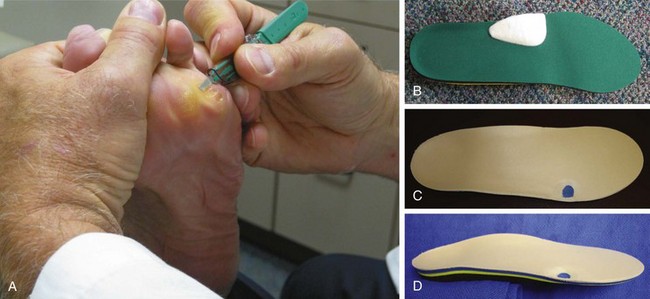
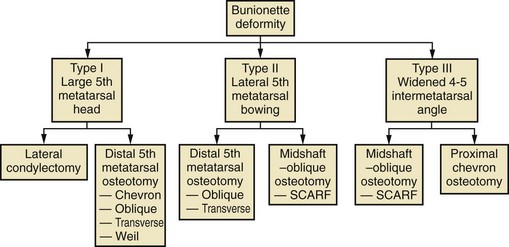
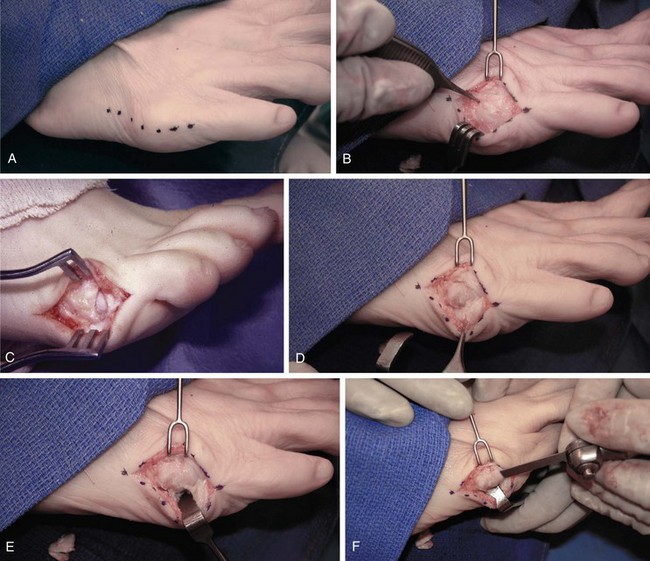
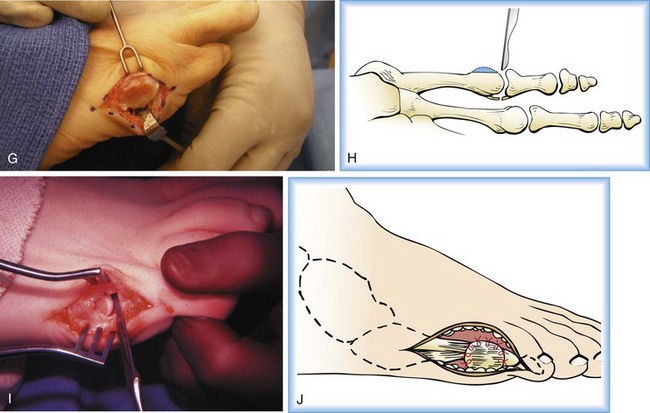
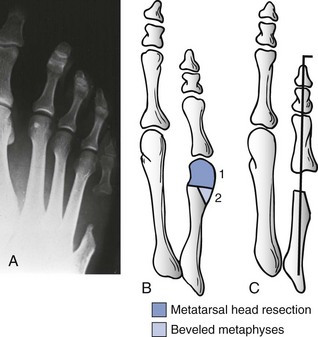
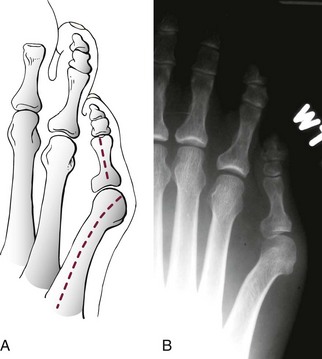
Chapter 9 DIAGNOSTIC AND RADIOGRAPHIC EXAMINATION Fifth Metatarsal Head Resection Distal Fifth Metatarsal Osteotomy Distal Transverse Medializing Osteotomy with Steinmann Pin Fixation Distal Chevron Osteotomy (Video Clip 43 Distal Oblique Osteotomy (Video Clip 45 Capital Oblique Osteotomy (Video Clip 44 Midshaft (Diaphyseal) Osteotomies (Video Clip 46 AUTHOR’S PREFERRED METHOD OF TREATMENT A bunionette deformity, or tailor’s bunion, is characterized by a painful prominence of the lateral eminence of the fifth metatarsal head. Davies16 observed that pressure over the lateral condyle of the fifth metatarsal head led to chronic irritation of the overlying bursa (Fig. 9-1). The position of a tailor sitting in a cross-legged position has given rise to the term tailor’s bunion.75 Friction between an underlying bony prominence and constricting footwear can lead to the development of a keratosis over the lateral aspect22,33,42 (Fig. 9-2A) or the plantar lateral aspect31 of the fifth metatarsal head (Figs. 9-2B and 9-3A). The fifth toe deviates in a medial direction at the fifth metatarsophalangeal (MTP) joint (Fig. 9-3B), and the fifth metatarsal deviates laterally with respect to the fourth metatarsal. Figure 9-3 A, Plantar keratosis associated with bunionette deformity. B, Abduction deformity of the fifth toe. Kelikian35 described a prominent fifth metatarsal lateral eminence of a bunionette deformity as being “analogous to the medial eminence of the first metatarsal head” in a hallux valgus deformity. DuVries22 described several anatomic variations in the fifth metatarsal head that can lead to a symptomatic bunionette. Thus the etiology and anatomic variations that occur with a bunionette deformity are much more complex than what was originally described by Kelikian35 and Davies.16 Although painful symptoms can be localized to the fifth MTP joint region, an abnormal alignment of the fifth metatarsal may be associated with a bunionette deformity. The major subjective complaints of a patient with a symptomatic bunionette deformity are pain and irritation caused by friction between constricting footwear and an underlying bony abnormality. On physical examination, an inflamed bursa,31,68,69 a lateral keratosis (see Fig. 9-2),20 a plantar keratosis (see Fig. 9-3),28,31,51 or a combined plantar lateral keratosis20,33 may be present. Diebold and Bejjani20 noted that two thirds of the patients in their series had significant pes planus. They reported that a third of the patients in their series developed a plantar keratosis, whereas half had a lateral keratotic lesion. The remaining had a combined plantar and lateral keratosis. Coughlin14 noted that 10% of the patients in his series had developed a plantar keratosis, 70% had developed a lateral keratosis, and 20% had developed a combined plantar and lateral keratosis. Some osteotomies do not allow elevation of the capital fragment with correction of the bunionette deformity; these procedures should be avoided in the presence of a plantar keratosis. The examination of the patient with a symptomatic bunionette is performed with the patient sitting and standing. The presence of pes planus, an Achilles tendon contracture, or other forefoot abnormalities must be recognized and treated appropriately if they are symptomatic. A key to preoperative planning is the recognition of a plantar keratosis in combination with a lateral keratosis because this differentiation can affect the choice of surgical procedure. In examining the bunionette deformity, an abducted fifth toe, as well as a digital rotational component to the axial deformity, must be recognized. A hammer toe deformity of the fifth toe might also be present. A bunionette can develop as an isolated deformity, but it can also develop in combination with a hallux valgus deformity. An increased angle between the fourth and fifth metatarsals (4-5 intermetatarsal [IM] angle), in combination with an increased angle between the first and second metatarsals, results in a very wide splayed-foot abnormality.3,16,31,34,65 Likewise, the need for other forefoot surgical procedures affects the ambulatory capacity of a patient and must be considered as well. A neurovascular examination is important for determining the suitability of the patient for surgical correction. Radiographic evaluation of a symptomatic bunionette deformity includes standing anteroposterior (AP) and lateral radiographs. The significant angular measurements that define a bunionette deformity are the angle of the fifth metatarsophalangeal joint (MTP-5 angle) (Fig. 9-4) and the 4-5 IM angle. The MTP-5 angle allows one to calculate the magnitude of medial deviation of the fifth toe in relation to the longitudinal axis of the fifth metatarsal shaft. Nestor et al53 reported that in normal feet the MTP-5 angle averaged 10.2 degrees, and Steele et al66 noted that in 90% of normal cases, the angle was 14 degrees or less. Nestor et al53 and Coughlin14 have reported that in feet with bunionettes the MTP-5 angle averaged 16 degrees. The 4-5 IM angle is a measure of the divergence of the fourth and fifth metatarsals and is the angle measured by the intersection of lines bisecting the axis of the fourth and fifth metatarsals.61 Divergence of the fourth and fifth metatarsals leads to pressure over the lateral eminence of the fifth metatarsal head.18,34,39 Fallat and Buckholz24 stated that the 4-5 IM angle in normal feet averaged 6.2 degrees (range, 3 to 11 degrees). Although some3,4,23,34,61 have noted that a 4-5 IM angle greater than 8 degrees can be considered abnormal, Fallat24 and Coughlin14 have reported the 4-5 IM angle on average to be greater than 9 degrees. In general, however, angular measurements serve only to describe a bunionette deformity; it is the symptoms and not the magnitude of deformity that necessitates specific surgical treatment. The width of the foot is determined by a diagonal line drawn from the medial edge of the medial eminence of the first metatarsal to the lateral aspect of the fifth metatarsal head. A prominent lateral condyle of the fifth metatarsal head can lead to a type 1 bunionette deformity (Fig. 9-5).22,24,68 Hypertrophy of the lateral condyle has been reported by DuVries22 and others.24,69,71 The incidence of a type 1 deformity is reported to vary in incidence from 16% to 33%.4,14,40 Zvijac et al75 noted a variance in width of the fifth metatarsal from 11 mm at the smallest to 14 mm at the widest, and Fallat24 stated that the normal width of the fifth metatarsal head was 13 mm. Throckmorton and Bradlee69 and Fallat and Buckholz20 both reported that with excessive pronation of the foot, the lateral plantar tubercle of the fifth metatarsal head rotated laterally to create the radiographic impression of an enlarged fifth metatarsal head. Fallat and Buckholz24 also reported a 3-degree increase in the 4-5 IM angle in the presence of a pes planus deformity. Whether true hypertrophy of the fifth metatarsal head occurs or prominence of the fifth metatarsal head results from pronation of the foot, a prominent lateral condyle of the fifth metatarsal head can become symptomatic without an increase in the 4-5 IM angle. Lateral bowing of the diaphysis of the fifth metatarsal shaft can lead to the development of a symptomatic prominence of the lateral condyle of the fifth metatarsal head* and is classified as a type 2 bunionette deformity (Fig. 9-6). Although the proximal fifth metatarsal shaft maintains a normal IM alignment, a lateral curvature develops in the diaphysis of the fifth metatarsal, which leads to a symptomatic bunionette deformity. A prominent lateral condyle of the fifth metatarsal head can also be caused by divergence of the fourth and fifth metatarsals, which is classified as a type 3 bunionette deformity (Fig. 9-7). Figure 9-6 Type 2 bunionette deformity is characterized by lateral bowing of the fifth metatarsal head. Figure 9-7 Type 3 bunionette deformity is characterized by an abnormally wide 4-5 intermetatarsal angle. Kitaoka et al,39 in evaluating a series of patients with a symptomatic bunionette deformity, reported that an increase in the 4-5 IM angle was most often associated with a symptomatic bunionette deformity. Fifth metatarsal bowing or an enlarged fifth metatarsal head was observed to be a cause in less than 10% of these cases, but Coughlin14 noted the incidence of lateral bowing of the fifth metatarsal to be 23%. Koti41 has suggested an additional type that involves two or more components of the other three types. This adds unnecessary complexity and does not aid in defining a treatment plan. Regardless of the underlying MTP joint orientation and fifth metatarsal angulation, the common symptom in all patients with a bunionette deformity is increased pressure over the lateral aspect of the fifth metatarsal head caused by constricting footwear. The female-to-male ratio is reported to vary from 3 : 1 to 10 : 16,8,26,53 in series of patients with symptomatic bunionettes that required surgical intervention. The increased frequency of occurrence of a bunionette deformity in the female population is most likely attributable to their predilection for high-fashion footwear. With time, the development of a hypertrophic keratosis or a thickened bursa can lead to increased symptoms. Harris mat studies can help in the assessment of increased pressure beneath a symptomatic fifth metatarsal head in association with a plantar keratosis (Fig. 9-8). It is important for a patient to recognize that the use of constricting footwear is a significant cause of symptoms and places increased pressure on a prominent fifth metatarsal head.15 Chronic irritation, pain, and swelling of the bursa overlying the fifth metatarsal head can be reduced by roomy, well-fitted shoes (Fig. 9-9).* Shaving of a hypertrophic callus (Fig. 9-10A) and padding (Fig. 9-10B-D) of a prominent fifth metatarsal head41,53 can reduce symptoms significantly. A prefabricated or custom orthotic device may be used to diminish pronation and, as a result, reduce discomfort over a prominent fifth metatarsal head (see Chapter 4). Conservative methods can be effective in a large number of patients. However, as painful plantar and lateral keratoses develop, surgical intervention may be necessary to relieve symptoms (Fig. 9-11). Various reported techniques are presented in this section. Preferred surgical methods are noted and discussed later in the chapter. Numerous surgical techniques have been described to correct a symptomatic bunionette deformity. These include lateral condylectomy,* fifth metatarsal head resection,21,35,37,51,72 fifth metatarsal implant arthoplasty,1 fifth-ray resection,5 distal metatarsal osteotomy,† diaphyseal osteotomy,‡ and proximal fifth metatarsal osteotomy.§ Correction of the underlying disorder is necessary for preventing a recurrence of deformity. Likewise, preservation of the function of the fifth MTP joint can prevent such complications as recurrence, subluxation, dislocation, or development of a transfer lesion. The main indication for a lateral condylectomy is an enlarged lateral condyle.10,58 In this situation, a condylectomy can produce an adequate repair, although a distal metatarsal osteotomy might still be the procedure of choice. A second indication is for the treatment of localized infection overlying the lateral fifth metatarsal head.10,41 Although lateral condylectomy might not achieve MTP joint realignment, it might alleviate the acute or chronic infection. Preoperative radiographs are important in the evaluation of a bunionette deformity. With lateral angulation of the fifth metatarsal shaft in relationship to the fourth metatarsal shaft (increased 4-5 IM angle; type 3 deformity) or with lateral bowing of the fifth metatarsal shaft (type 2 deformity), a condylectomy does not effectively reduce a prominent fifth metatarsal lateral eminence. With an enlarged 4-5 IM angle, a fifth metatarsal osteotomy is necessary to correct this divergence.45 The significant recurrence rate after lateral condylectomy is attributable to the use of a lateral condylectomy when a fifth metatarsal osteotomy is indicated. Kelikian35 noted that “at best a lateral condylectomy is a temporizing measure like simple exostectomy on the medial side of the foot; in time deformity will recur.” 1. The patient is positioned in a semilateral decubitus position. 2. The extremity is cleansed in a normal fashion. 3. A longitudinal skin incision is centered over the lateral condyle of the fifth metatarsal head and extends from the interphalangeal joint to 1 cm proximal to the fifth metatarsal condyle. The dorsal cutaneous nerve of the fifth toe is protected (Fig. 9-12A and B). 4. An inverted L-shaped capsular incision is used to detach the dorsal and proximal fifth metatarsal capsule. The weakest portion of the capsule is detached, and the strongest capsular attachments to the proximal phalanx and plantar capsule are maintained (Fig. 9-12C-E). 5. A sagittal saw (or osteotome) is used to resect the lateral condyle of the fifth metatarsal head (Fig. 9-12F-G). 6. The fifth metatarsal head is exposed, and with traction placed on the fifth toe, the MTP joint is distracted and the medial capsule is released with a scalpel (Fig. 9-12H and I). 7. The MTP capsule is closed by approximating it to the fifth MTP metatarsal metaphyseal periosteum and to the abductor digiti quinti muscle proximally (Fig. 9-12J). (For improved fixation, a drill hole in the fifth metatarsal dorsolateral metaphysis may be used to anchor the capsule repair.) A meticulous capsule repair is necessary to prevent recurrence of the deformity or lateral subluxation of the MTP joint. 8. The skin is closed routinely, and a compression dressing is applied. Although this procedure has been frequently recommended for the repair of a bunionette deformity,* in general, only anecdotal follow-up has been published for series using a lateral condylectomy. Reported postoperative complications include recurrence of deformity (Fig. 9-13),* subluxation of the MTP joint (Fig. 9-14),33,38,65 and poor weight bearing with excessive resection.42 Kitaoka and Holiday36 reported on 16 patients (21 feet) who had undergone a lateral condylar resection for a symptomatic bunionette (average follow-up, 6.4 years). Seventy-one percent of the patients were satisfied with their result. Twenty-three percent reported some element of forefoot pain, although half these patients considered it mild. The average preoperative 4-5 IM angle measured 12.3 degrees, and postoperatively it measured 11.1 degrees, for an average correction of 1.2 degrees. Much of this correction can be accounted for by the measurement techniques. The metatarsophalangeal-5 angle averaged 17.0 degrees preoperatively and 14.6 degrees postoperatively. This correction was not significant on statistical analysis. Furthermore, the authors concluded that no correlation existed between the amount of correction and the level of patient satisfaction. In two feet, the MTP joint subluxated postoperatively as the fifth toe displaced medially. A tight capsule closure with excision of redundant MTP joint capsule was recommended to minimize this postoperative complication. The authors also concluded that although only a limited degree of correction of the deformity was possible with this procedure, a lateral condylectomy was often successful in relieving symptoms. No transfer lesions were reported in this series. With an intractable plantar keratotic lesion beneath the fifth metatarsal head, the authors believed that a simple condylectomy was contraindicated. Although a lateral condylar resection is a simple treatment for a bunionette deformity, the authors recognized the significant limitations of the procedure. A meticulous fifth metatarsal capsule repair can prevent subluxation and recurrence of a bunionette deformity.48,65 Attention to repair of the abductor digiti quinti muscle and fifth metatarsal capsule can prevent later dislocation of the MTP joint.33 The failure of a lateral condylectomy as an effective treatment of a bunionette deformity has resulted in the recommendation for more extensive resection procedures. Excision of the fifth metatarsal head (Fig. 9-15),1,21,22,37 resection of the distal half of the fifth metatarsal (Fig. 9-16),51 and fifth-ray resection (Fig. 9-17)5 have all been advocated as treatment for a symptomatic bunionette deformity. McKeever51 advocated excision of the fifth metatarsal head and one half to two thirds of the fifth metatarsal shaft; Brown5 found that resection of almost the entire fifth ray and a fifth toe amputation adequately narrowed the foot and relieved symptoms. Kelikian35 recommended McKeever’s technique but syndactylized the fourth and fifth toes to avoid a symptomatic flail fifth toe deformity. 1. The patient is positioned in a semilateral decubitus position. 2. The extremity is cleansed in a normal fashion. 3. A longitudinal incision is centered over the lateral eminence, extending from the midportion of the proximal phalanx to 1 cm above the lateral eminence. (With plantar ulceration, a dorsal incision may be used. With rheumatoid arthritis when multiple metatarsal heads are excised, a longitudinal IM incision may be placed in the fourth IM space.) 4. The capsular structures are released, and the fifth metatarsal head is exposed. 5. The fifth metatarsal shaft is transected in the metaphyseal region with a sagittal saw or a bone-cutting forceps (see Fig. 9-16A and B). 6. The prominent lateral and plantar aspects of the metatarsal shafts are beveled with a rongeur. 7. A 0.045-inch Kirschner wire is introduced at the base of the proximal phalanx and driven distally through the tip of the toe (see Fig. 9-16C). It is then driven in a retrograde manner into the metatarsal diaphysis to align and stabilize the fifth toe. With plantar ulceration or infection, Kirschner wire stabilization is contraindicated. 8. The capsule is plicated with interrupted absorbable suture. The skin edges are approximated in a routine manner. Although fifth metatarsal head resection has been recommended for treating a symptomatic bunionette deformity, in general, only anecdotal experience has been reported. McKeever51 reported success in the treatment of 60 cases, but no specific criteria were used for the postoperative evaluation, and no complications were noted. Extensive metatarsal head resection can lead to retraction of the fifth toe,21,37,42 subluxation of the fifth toe,33,37 and development of a transfer lesion beneath the fourth metatarsal head.21,37,42 The development of a flail fifth toe deformity might require syndactylization to the fourth toe. With fifth metatarsal head resection in seven patients (11 feet), at an average 8-year follow-up, Kitaoka and Holiday37 reported 82% fair or poor results. Complications, which occurred in 64% of cases, included severe shortening of the toe (36%), transfer lesions or unresolved plantar callosities (75%), stiffness (25%), and continued symptoms (27%). The preoperative 4-5 IM angle, which averaged 11 degrees, was noted to increase to 15.5 degrees after surgery. Fifth-ray shortening averaged 10 mm. Because of such complications as fifth-ray shortening, transfer metatarsalgia, malalignment of the fifth toe, and loss of MTP joint function of the fifth ray, Kitaoka and Holiday37 concluded that excisional arthroplasty was not indicated as a primary procedure. In 21 patients who underwent fifth metatarsal head excision (average follow-up, 17 months), Dorris and Mandel21 reported malalignment of the fifth toe in 59% of patients. Although 84% of patients were satisfied with the results at postoperative evaluation, limited short-term follow-up of as little as 3 months raises a question as to the long-term efficacy and durability of this procedure in light of the report of Kitaoka and Holiday.37 Armstrong et al2 used fifth metatarsal head resection for plantar ulcerations in patients with diabetes, and reported excellent resolution of symptoms with this technique in 22 cases. Addante et al1 reported on 35 patients (50 cases) after fifth metatarsal head resection and placement of silicone spheric implants. They reported an 84% success rate. Complications occurred in 16% of cases and included traumatic dislocation of the implant, chronic subluxation, silicone inflammatory reaction, wound dehiscence, abscess formation, intractable plantar keratosis (IPK), and transfer metatarsalgia. An osteotomy of the fifth metatarsal may be used to correct alignment of the fifth metatarsal. Davies16 stated that it was “unnecessary and unsatisfactory” to perform a fifth metatarsal osteotomy. Lelièvre,44,45 however, recognized that an increased 4-5 IM angle should be corrected as a part of a bunionette repair. Kelikian35 cautioned that delayed healing can occur after a fifth metatarsal osteotomy. The location of the osteotomy and the surgical technique performed have a significant effect on the ultimate success of a metatarsal osteotomy. Distal, diaphyseal, and proximal metatarsal osteotomies have all been recommended in the treatment of symptomatic bunionette deformities. Many types of distal fifth metatarsal osteotomies have been recommended for the treatment of symptomatic bunionettes.* Although less correction of an increased 4-5 IM angle is achieved than with more proximal osteotomies, a distal fifth metatarsal osteotomy achieves significantly more correction than with a lateral condyle resection. Instability of some types of distal metatarsal osteotomies has caused concern regarding the loss of alignment,29,33 development of a subsequent transfer lesion, and recurrence of deformity.34 Hohmann32 and later Steinke67 described a distal fifth metatarsal osteotomy, reporting on the use of a transverse osteotomy of the fifth metatarsal neck. Kaplan et al33 advocated a distal closing-wedge fifth metatarsal osteotomy that was internally fixed with a Kirschner wire. They suggested internal fixation because the distal osteotomy was unstable and might rotate postoperatively, with resulting loss of correction. Haber and Kraft31 used a distal fifth metatarsal crescentic osteotomy. They did not use internal fixation to stabilize the osteotomy site and reported excessive callus formation at the osteotomy site and delayed healing. Catanzariti et al9 performed a distal oblique fifth metatarsal osteotomy without internal fixation and reported a 26% recurrence rate and transfer lesions in 35% of cases. Throckmorton and Bradlee69 and others4,7,13,38 described a distal fifth metatarsal transverse chevron osteotomy. Because of the stable shape of this osteotomy, Throckmorton did not use internal fixation. Boyer and DeOrio4 have used an absorbable fixation pin for internal fixation of a chevron osteotomy. A reverse Mitchell procedure,42,65 distal chevron osteotomy,4,26,38,52,69 distal transverse osteotomy,32,33,67 distal crescentic osteotomy,31 scarf,17,30,58,62 and distal oblique osteotomy* have all been recommended as distal fifth metatarsal osteotomy techniques. Nonetheless, a distal fifth metatarsal osteotomy might help to achieve adequate correction of a symptomatic bunionette deformity. With a type 1 deformity (enlarged head) or a moderate type 2 or type 3 deformity, a distal fifth metatarsal osteotomy may be used to achieve adequate surgical correction. The choice of a specific type of osteotomy depends on the experience of the surgeon and the anatomic variation present. Internal fixation is preferable because it stabilizes the correction obtained at surgery. Usually, a Kirschner wire, if used for internal fixation, can be removed without difficulty in an office setting a few weeks after surgery. An absorbable pin fixation has been used with success and provides an alternative to later hardware removal.4,26 Screw fixation, may be left indefinitely because it is usually asymptomatic.
Bunionettes
![]() )
)
![]() )
)
![]() )
)
![]() )
)

Anatomy
Clinical Symptoms
Physical Examination
Diagnostic and Radiographic Examination

Treatment
Conservative Treatment
Surgical Treatment
Surgical Techniques
Lateral Condylectomy
Indications
Contraindications
Surgical Technique
Results and Complications
Fifth Metatarsal Head Resection
Surgical Technique
Results and Complications
Distal Fifth Metatarsal Osteotomy
Indications
Distal Transverse Medializing Osteotomy with Steinmann Pin Fixation29,43,73